Medullary thyroid carcinoma (MTC) is an uncommon subtype of thyroid carcinoma with an intermediate prognosis between differentiated and poorly differentiated thyroid carcinomas. We report the clinical case of a patient diagnosed with sporadic MTC with lymphatic metastases and review its course, treatment, and response to the tyrosine kinase inhibitor sorafenib.
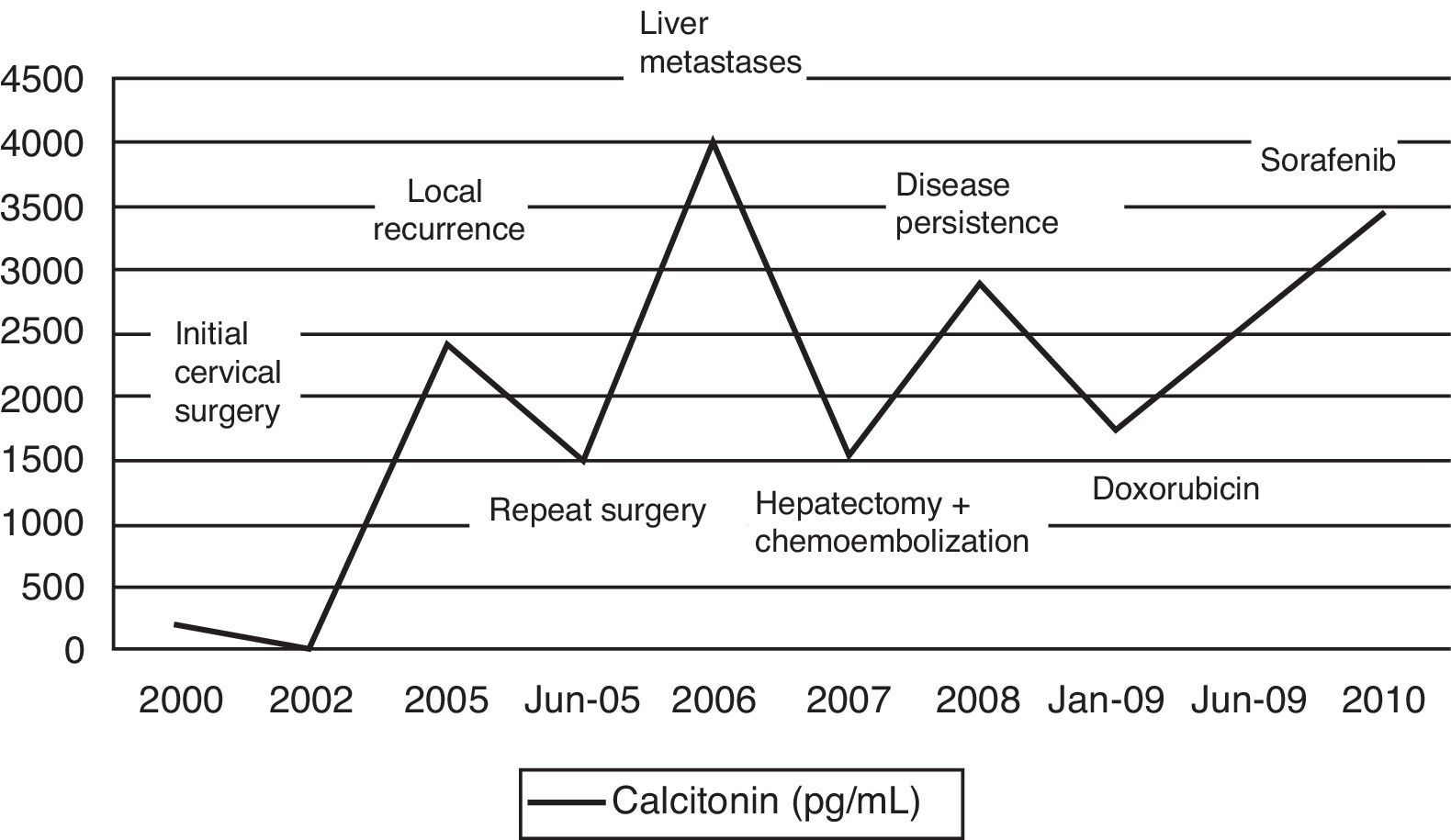
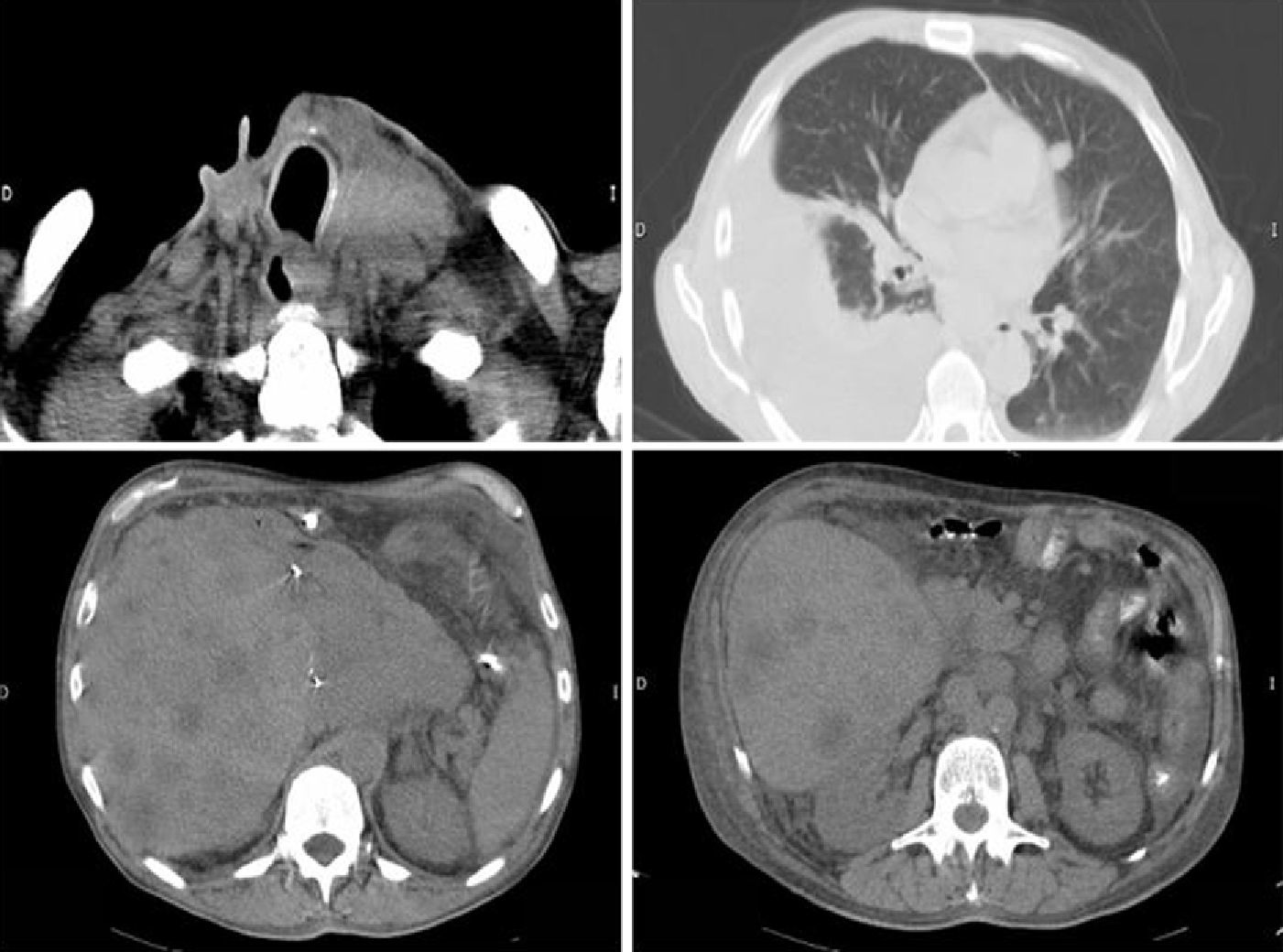
The patient was a 58-year-old male who consulted in 1999 for rapidly growing left thyroid nodules and underwent surgery consisting of total thyroidectomy with central lymphadenectomy. Pathological diagnosis was MTC with cervical lymph node metastases. A genetic study for the RET proto-oncogene was negative. External radiotherapy was administered, and in 2000 the patient was referred to our center for specialized assessment and repeat surgery of local recurrence. An extension study showed multiple liver metastases which were treated by subtotal hepatectomy, radio frequency, and chemoembolization. In mid-2008, marked elevations occurred in calcitonin and carcinoembryonic antigen (CEA) levels, and positron emission tomography revealed the persistence of mediastinal and liver lymph node metastases and a new local recurrence. The patient was assessed by the oncology department and completed systemic chemotherapy with doxorubicin in 2009. Tumor markers initially decreased, but increased again six months after chemotherapy (Fig. 1). In July 2010, treatment was started with the tyrosine kinase inhibitor sorafenib (400mg/12h). At five months, the patient was admitted for diffuse abdominal pain associated with anorexia, weight loss, and lower limb edema. The requested tests showed biochemical tumor progression with elevated calcitonin levels (Fig. 1) and clinical signs of lung micrometastases, right pleural effusion, and a retroperitoneal adenopathic mass infiltrating the inferior vena cava (Fig. 2). The drug was therefore discontinued, and palliative symptomatic treatment was continued. The patient died two months later.
Surgery is currently the only curative treatment for MTC. The most significant prognostic factors are the initial stage and extrathyroid extension of the primary tumor.1 Because of the high recurrence risk in these patients, particularly in those with nodal involvement or large tumor size, adjuvant radiotherapy has been proposed. However, radiotherapy causes extensive fibrosis, which makes subsequent surgical treatment difficult. It is therefore reserved as a palliative treatment for local disease when a surgical approach is not feasible. Repeat cervical or mediastinal surgery is preferred, and achieves normalization of calcitonin levels in up to one-third of cases.2 In our patient, both options were used to control cervical disease and decreased tumor marker levels (Fig. 1). Distant metastases occur in 5% of cases and are most common in the liver. Available therapies at this level only achieve a reduction in size and number when less than 30% of the liver is involved.3 Chemotherapy is an effective alternative in a limited proportion of patients (20–30%), but at the expense of a high toxicity. Different agents, such as doxorubicin, dacarbazine, or 5-fluorouracyl, have been tested as monotherapy.4 Other alternatives include somatostatin analogs labeled with the radiopharmaceutical yttrium-90 (DOTATOC) or the administration of metaiodobenzylguanidine (MIBG).5
New RET inhibitors such as motesanib, sunitinib, vandetanib, and sorafenib are currently being used. These molecules prevent the activation of various cell proliferation pathways by binding to the tyrosine kinase domains of the receptor encoded by the RET gene. Some of them also have activity against the vascular endothelial growth factor receptor and fibroblast growth factor.4 Studies have focused on the treatment of differentiated thyroid carcinoma, but there are also studies of a significant number of patients with MTC. A preclinical study with sorafenib showed direct effects on calcitonin gene expression, decreasing levels before tumor size was reduced.6 In a small study, five patients with MTC were treated with sorafenib, and a favorable response was reported in two of them (including a complete remission) after six months of treatment. Symptom improvement was also seen in all cases.7 In a Phase II clinical trial of sorafenib, a response was seen in 30% of cases.8 Partial response was also reported in three out of six patients with MTC participating in a Phase I study of the combination of sorafenib and a farnesyltransferase inhibitor, tipifarnib.9
Sorafenib has been approved by the Food and Drug Administration to treat advanced renal cell carcinoma and unresectable hepatocellular carcinoma, but is being used, as noted above, in metastatic, progressive differentiated thyroid carcinoma. It is usually well tolerated, and its most common adverse events include hand–foot syndrome, skin rash, hypertension, asthenia, and hair loss. In our patient, the use of this drug for five months was well tolerated, but had to be discontinued due to biochemical and clinical disease progression, and was replaced by palliative measures.
To sum up, the management of patients with metastases should consist of a multidisciplinary approach that includes various treatments to achieve stabilization of the disease. A combination of such treatments allows for a survival rate of approximately 40% at 10 years of diagnosis. Research and development of new therapeutic molecular targets may improve the survival rates of patients not cured with surgery.
Please cite this article as: García-Martín A, et al. Manejo terapéutico del carcinoma medular de tiroides metastásico: papel de los nuevos inhibidores de la tirosincinasa. Endocrinol Nutr. 2013;60:152–3.