To estimate the prevalence of obesity and its associated cardiovascular risk in the general population of a health area in Extremadura.
Materials and methodsA cross-sectional study on a random population sample aged 25–79 years from the Don Benito-Villanueva (Badajoz) health area. Risk factors and cardiovascular disease were examined. Anthropometric and blood pressure measurements were collected, and a blood sample was taken. Obese subjects were categorized into different risk levels as proposed by the Spanish Society for the Study of Obesity, and the influence of obesity on estimation of the risk of ischemic heart disease was studied using the Framingham function, as adapted for Spain.
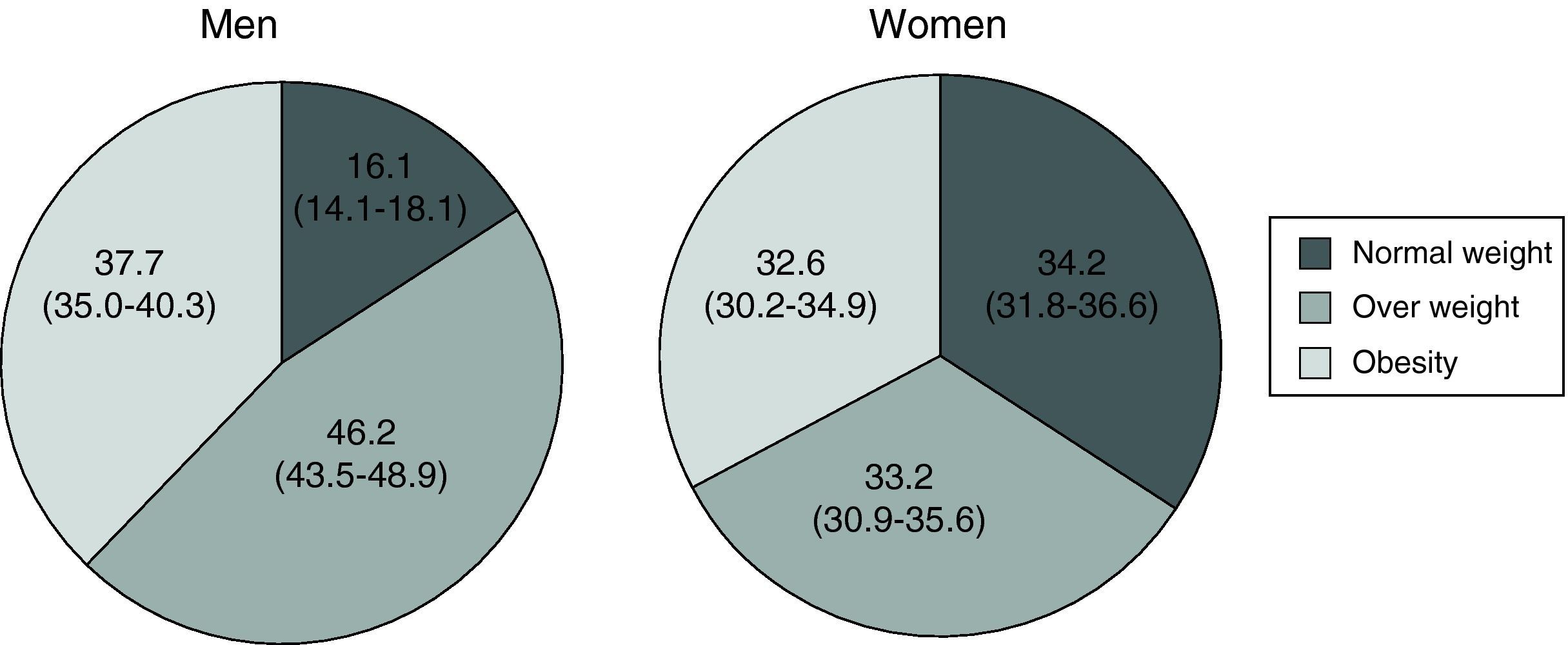
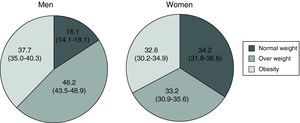
ResultsA total of 2833 of the 3521 subjects screened (80.5%) participated in the study. Mean age was 51.2 years (SD 14.7), and 46.5% were males. Male subjects had a greater prevalence of overweight and obesity (46.2% and 37.7% respectively) as compared to females (37.7% and 32.6%) (p<0.005 and p<0.05, respectively). Only 10% of obese subjects had no increased cardiovascular risk. Obesity was associated to an 8-fold increase in the presence of a high risk for ischemic heart disease in females (p<0.001), as compared to a 1.4-fold increase in males (p=0.095).
ConclusionsObesity is highly prevalent and affects, together with overweight, 74.1% of the population in an Extremadura health area. A vast majority of obese subjects have an increased cardiovascular risk, which is very marked for ischemic heart disease in females.
Estimar la prevalencia de la obesidad y el riesgo cardiovascular asociado en la población general de un área de salud de Extremadura.
Material y métodosEstudio transversal sobre una muestra aleatoria de población entre 25 y 79 años procedente del área de salud de Don Benito-Villanueva (Badajoz). Se estudió la presencia de factores de riesgo y enfermedad cardiovascular. Se recogieron medidas antropométricas, de presión arterial y muestra sanguínea. Se categorizó a la población obesa en distintos niveles de riesgo tal como propone la Sociedad Española para el Estudio de la Obesidad y se estudió la influencia de la obesidad en la estimación del riesgo de cardiopatía isquémica según la función de Framinghan adaptada para España.
ResultadosDe los 3.521 sujetos seleccionados participaron 2.833 (80,5%). La edad media fue 51,2 años (DE 14,7) y el 46,5% fueron hombres. La prevalencia de sobrepeso y obesidad fue superior en hombres (46,2 y 37,7%) con respecto a las mujeres (37,7 y 32,6%) (p<0,005 y p<0,05 respectivamente). Solo el 10% de los obesos no mostraron un riesgo cardiovascular aumentado. La obesidad se asoció a un incremento de presentar riesgo alto de cardiopatía isquémica de 8 veces en la mujer (p<0,001) por 1,4 veces en el hombre (p=0,095).
ConclusionesLa obesidad es muy prevalente y afecta junto al sobrepeso al 74,1% de la población de un área de salud de Extremadura. La amplia mayoría de los obesos tienen un riesgo cardiovascular aumentado, siendo de gran magnitud para la cardiopatía isquémica en la mujer.
The prevalence of obesity is increasing worldwide. It is estimated that there are approximately 1000 million people with overweight and 500 million people with obesity.1 According to estimates made one decade ago, the prevalence of obesity in Spain was approximately 15% in the adult population and 30% in non-institutionalized people over 65 years of age.2 However, its prevalence also appears to have increased, according to more recent studies.3
Obesity is the sixth leading cause of death worldwide, and its presence in subjects aged 40 causes the loss of 7 potential years of life.4 Diseases favored by obesity include cardiovascular diseases (CVDs), but controversy still exists as to whether it acts as an independent risk factor5,6 or through the classical cardiovascular risk factors7 with which it is strongly associated. The fact that obesity is not included in the most recent predictive equations as an independent risk factor8 suggests that it acts mainly through these factors.
Because of this limitation and in order to demonstrate the increased risk conferred by obesity, the Spanish Society for the Study of Obesity (SEEDO) proposed a classification that stratified the chance of disease based on adipose tissue distribution and some other associated conditions or comorbidities.9 This evaluation was proposed in order to make interventions against obesity more effective.
This study was intended to determine firstly, the prevalence of obesity in a general population sample. A second objective was to assess the risk of suffering cardiovascular disease associated with obesity according to the most recent SEEDO consensus and to assess the risk of ischemic heart disease using the Framingham equation as adapted for Spain.
Materials and methodsStudy design and populationA cross-sectional study of cardiovascular risk factors was conducted on a population sample in Extremadura, Spain. The study methods, response rate, and demographic variables have previously been reported.10 A sample of 2833 subjects aged 25–79 years randomly selected from the database of the Extremadura health system, with universal healthcare coverage (99.4%) at the time of the study, was surveyed between 2007 and 2009. Subjects came from the Don Benito-Villanueva de la Serena (Badajoz) healthcare area. The target population consisted of 75,455 inhabitants. The sample size was 2.400 and was calculated so as to estimate the prevalence of the different risk factors with the maximum degree of indeterminacy and a 2% precision.
VariablesA history of CVD and risk factors was collected from each participant using a standardized protocol. Surveys used and a detailed description of procedures are available at the study website.11 Two previously trained nurses measured subject weight, height, and waist circumference (WC) in accordance with international recommendations. Blood pressure was measured three times in each arm using an electronic monitor, and a fasting blood sample was drawn.
Body mass index (BMI), defined as weight (kg)/height2 (m2), was stratified into three categories9: normal weight if BMI <25, overweight if BMI 25–29.9, and obesity if BMI ≥30. WC was considered pathological based on the cut-off points of high risk for a Caucasian population of >102cm in men and >88cm in women.12 Subjects were considered to suffer diabetes, high blood pressure, or hypercholesterolemia if they were taking drugs for each of these conditions or had blood glucose levels ≥126mg/dL, mean blood pressure levels ≥140/90mmHg, or total cholesterol levels ≥240mg/dL at baseline laboratory tests respectively. Smoking was defined as current smoking or smoking cessation less than one year before.
The sample was classified based on BMI and WC, assigning a relative risk value to each category compared to baseline, which agreed with the anthropometric measures of lower risk, as proposed by the 2007 SEEDO consensus.9 The obese population, defined by a BMI ≥30, was also categorized in risk levels based on the different associated clinical conditions proposed by this same consensus:
- •
Very high risk: the presence of a history of CVD (ischemic heart disease, stroke, arterial revascularization in any territory or lower limb amputation for ischemia) or diabetes (defined as current drug treatment for diabetes or basal blood glucose levels ≥126mg/dL.
- •
High risk: compliance with metabolic syndrome criteria according to the latest proposed definition12 or any two of the following conditions:
- ∘
A family history of early mortality for CVD (under 55 years in men and 65 years in women).
- ∘
Active smoking or smoking cessation less than one year before.
- ∘
Systolic or diastolic blood pressure values ≥130/85mmHg respectively.
- ∘
LDL cholesterol ≥130mg/dL.
- ∘
HDL cholesterol <40mg/dL in men or <50mg/dL in women.
- ∘
Impaired fasting glucose ≥100mg/dL and <126mg/dL.
- ∘
Triglyceride levels >150mg/dL.
- ∘
Age ≥45 years in men; for women, age ≥55 years or postmenopausal.
- •
Baseline risk: if none of the above criteria were met.
Coronary risk was assessed using the Framingham equation as adapted for Spain13 in participants aged 35–74 years, excluding those who already had CVD. Risk was compared based on the presence of obesity and a pathological WC. Risk levels were categorized based on the latest recommendations by their authors14 as low (<5%), moderate (5–9.9%), high (10–14.9%), and very high (≥15%). High and very high risk categories were pooled because it is at these categories where treatment intensification is recommended and due to the low number of cases in the latter group. This risk function was used because it is the only one validated for Spain.15
Statistical analysisQuantitative variables are presented as mean and standard deviation (SD), and qualitative variables as absolute and relative frequencies. Means difference was analyzed using a Student's t test and, if there were more than two groups, using analysis of variance. A Chi-square test was used for differences in prevalence, and to calculate if there were gradients, in the event of more than two groups, the p-value of tendencies of this same test was used.
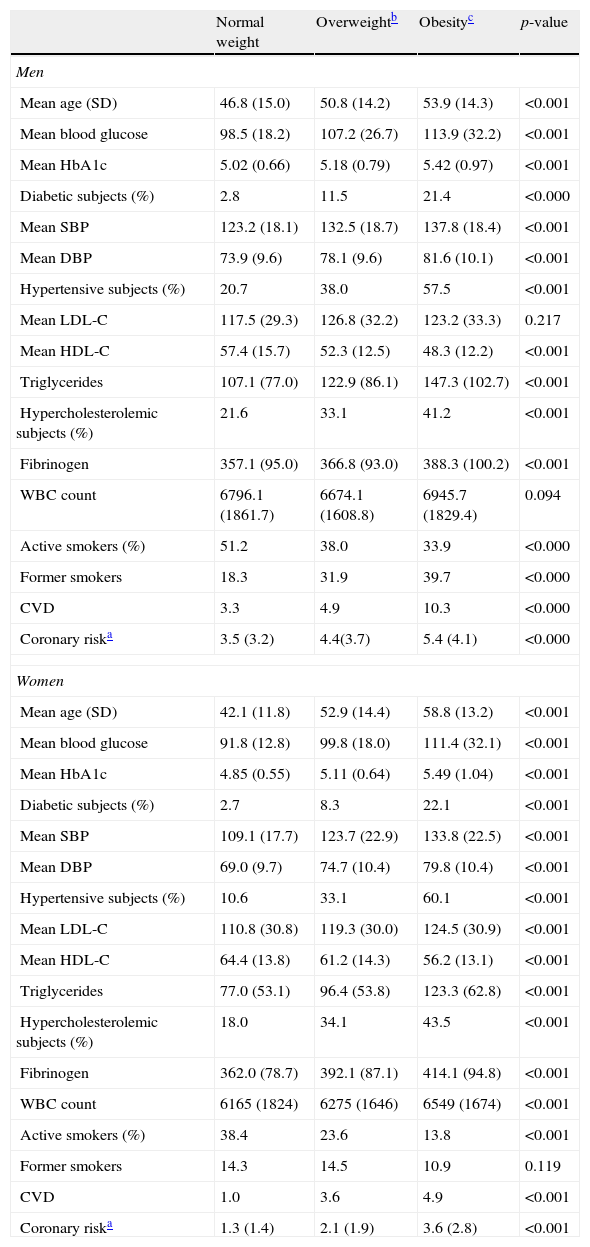
ResultsA total of 2853 of the 3521 subjects screened participated (participation rate, 80.5%). Mean sample age was 51.2 years (SD 14.7), and 46.5% of subjects were men. All other sociodemographic characteristics have previously been reported.10 Mean overall BMI was 28.6 (SD 5.4), 29.2 (SD 4.7) in men and 28.1 (SD 5.8) in women (p<0.001). Men had a greater prevalence of overweight (46.2%) and obesity (37.7%) as compared to women (33.2% and 32.6% respectively). Differences were statistically significant (p 0.001; p 0.01) (Fig. 1). As shown in Table 1, a gradient was seen in both sexes in the values of the different variables related to metabolic, hemodynamic, coagulation, and inflammatory aspects depending on BMI, and also in the prevalence of the different risk factors. Only LDL cholesterol and total WBC count in men showed no such association with BMI levels. Active smoking showed an inverse association in both sexes. A history of CVD and the estimation of mean risk of ischemic heart disease also increased with obesity.
Variables related to cardiovascular risk by BMI gradient.
| Normal weight | Overweightb | Obesityc | p-value | |
| Men | ||||
| Mean age (SD) | 46.8 (15.0) | 50.8 (14.2) | 53.9 (14.3) | <0.001 |
| Mean blood glucose | 98.5 (18.2) | 107.2 (26.7) | 113.9 (32.2) | <0.001 |
| Mean HbA1c | 5.02 (0.66) | 5.18 (0.79) | 5.42 (0.97) | <0.001 |
| Diabetic subjects (%) | 2.8 | 11.5 | 21.4 | <0.000 |
| Mean SBP | 123.2 (18.1) | 132.5 (18.7) | 137.8 (18.4) | <0.001 |
| Mean DBP | 73.9 (9.6) | 78.1 (9.6) | 81.6 (10.1) | <0.001 |
| Hypertensive subjects (%) | 20.7 | 38.0 | 57.5 | <0.001 |
| Mean LDL-C | 117.5 (29.3) | 126.8 (32.2) | 123.2 (33.3) | 0.217 |
| Mean HDL-C | 57.4 (15.7) | 52.3 (12.5) | 48.3 (12.2) | <0.001 |
| Triglycerides | 107.1 (77.0) | 122.9 (86.1) | 147.3 (102.7) | <0.001 |
| Hypercholesterolemic subjects (%) | 21.6 | 33.1 | 41.2 | <0.001 |
| Fibrinogen | 357.1 (95.0) | 366.8 (93.0) | 388.3 (100.2) | <0.001 |
| WBC count | 6796.1 (1861.7) | 6674.1 (1608.8) | 6945.7 (1829.4) | 0.094 |
| Active smokers (%) | 51.2 | 38.0 | 33.9 | <0.000 |
| Former smokers | 18.3 | 31.9 | 39.7 | <0.000 |
| CVD | 3.3 | 4.9 | 10.3 | <0.000 |
| Coronary riska | 3.5 (3.2) | 4.4(3.7) | 5.4 (4.1) | <0.000 |
| Women | ||||
| Mean age (SD) | 42.1 (11.8) | 52.9 (14.4) | 58.8 (13.2) | <0.001 |
| Mean blood glucose | 91.8 (12.8) | 99.8 (18.0) | 111.4 (32.1) | <0.001 |
| Mean HbA1c | 4.85 (0.55) | 5.11 (0.64) | 5.49 (1.04) | <0.001 |
| Diabetic subjects (%) | 2.7 | 8.3 | 22.1 | <0.001 |
| Mean SBP | 109.1 (17.7) | 123.7 (22.9) | 133.8 (22.5) | <0.001 |
| Mean DBP | 69.0 (9.7) | 74.7 (10.4) | 79.8 (10.4) | <0.001 |
| Hypertensive subjects (%) | 10.6 | 33.1 | 60.1 | <0.001 |
| Mean LDL-C | 110.8 (30.8) | 119.3 (30.0) | 124.5 (30.9) | <0.001 |
| Mean HDL-C | 64.4 (13.8) | 61.2 (14.3) | 56.2 (13.1) | <0.001 |
| Triglycerides | 77.0 (53.1) | 96.4 (53.8) | 123.3 (62.8) | <0.001 |
| Hypercholesterolemic subjects (%) | 18.0 | 34.1 | 43.5 | <0.001 |
| Fibrinogen | 362.0 (78.7) | 392.1 (87.1) | 414.1 (94.8) | <0.001 |
| WBC count | 6165 (1824) | 6275 (1646) | 6549 (1674) | <0.001 |
| Active smokers (%) | 38.4 | 23.6 | 13.8 | <0.001 |
| Former smokers | 14.3 | 14.5 | 10.9 | 0.119 |
| CVD | 1.0 | 3.6 | 4.9 | <0.001 |
| Coronary riska | 1.3 (1.4) | 2.1 (1.9) | 3.6 (2.8) | <0.001 |
CVD: prior cardiovascular disease; Active smokers: current smokers or subjects quitting smoking less than one year before; BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure.
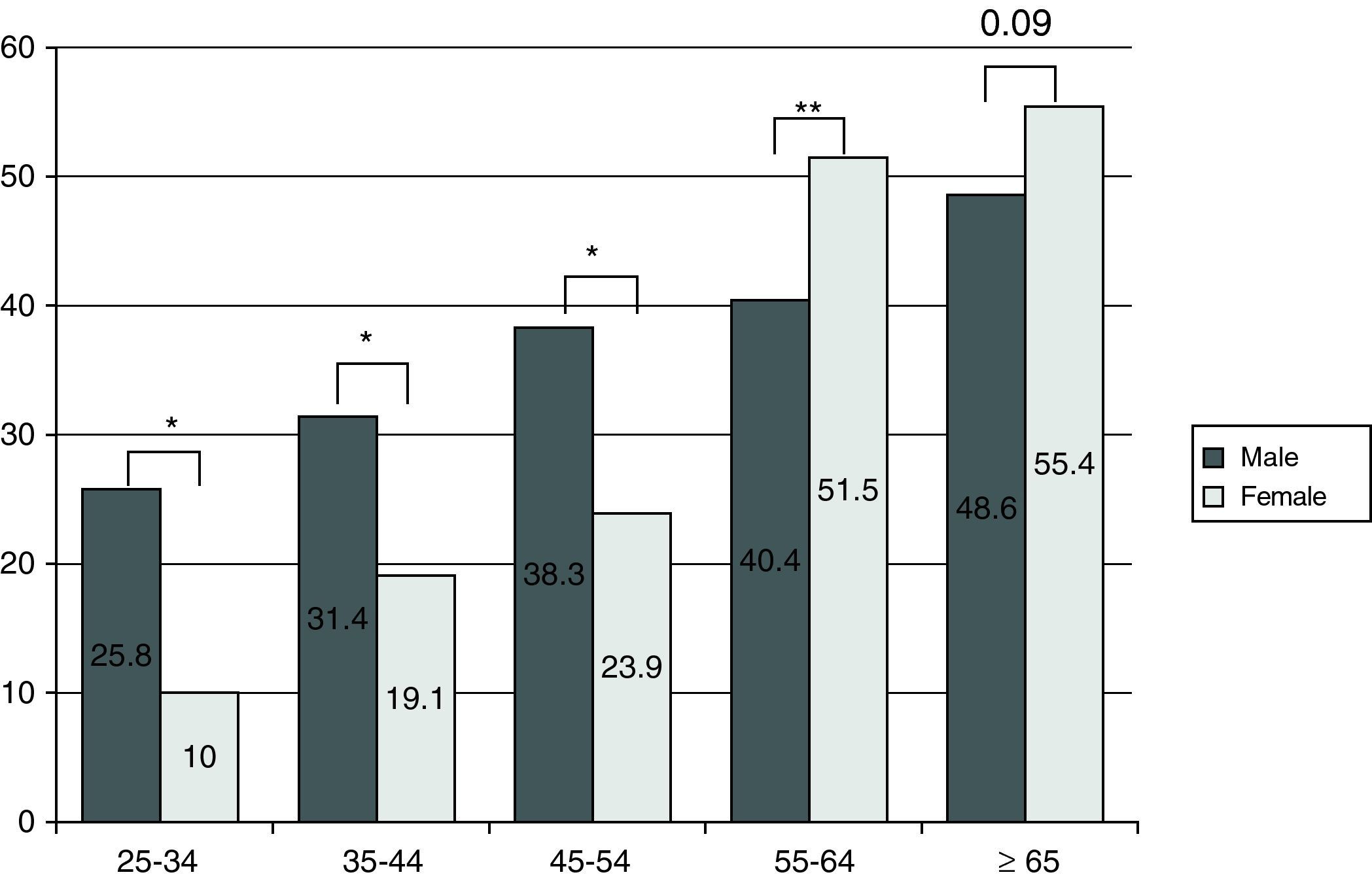
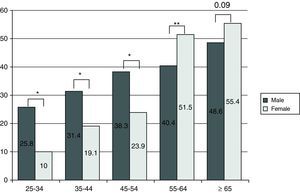
The prevalence of obesity increased with age in both sexes (p<0.001) and was higher in men until the age of 55 years, after which there was a higher prevalence in women. The highest prevalence was found in subjects over 65 years of age, who showed a joint prevalence higher than 50% (Fig. 2).
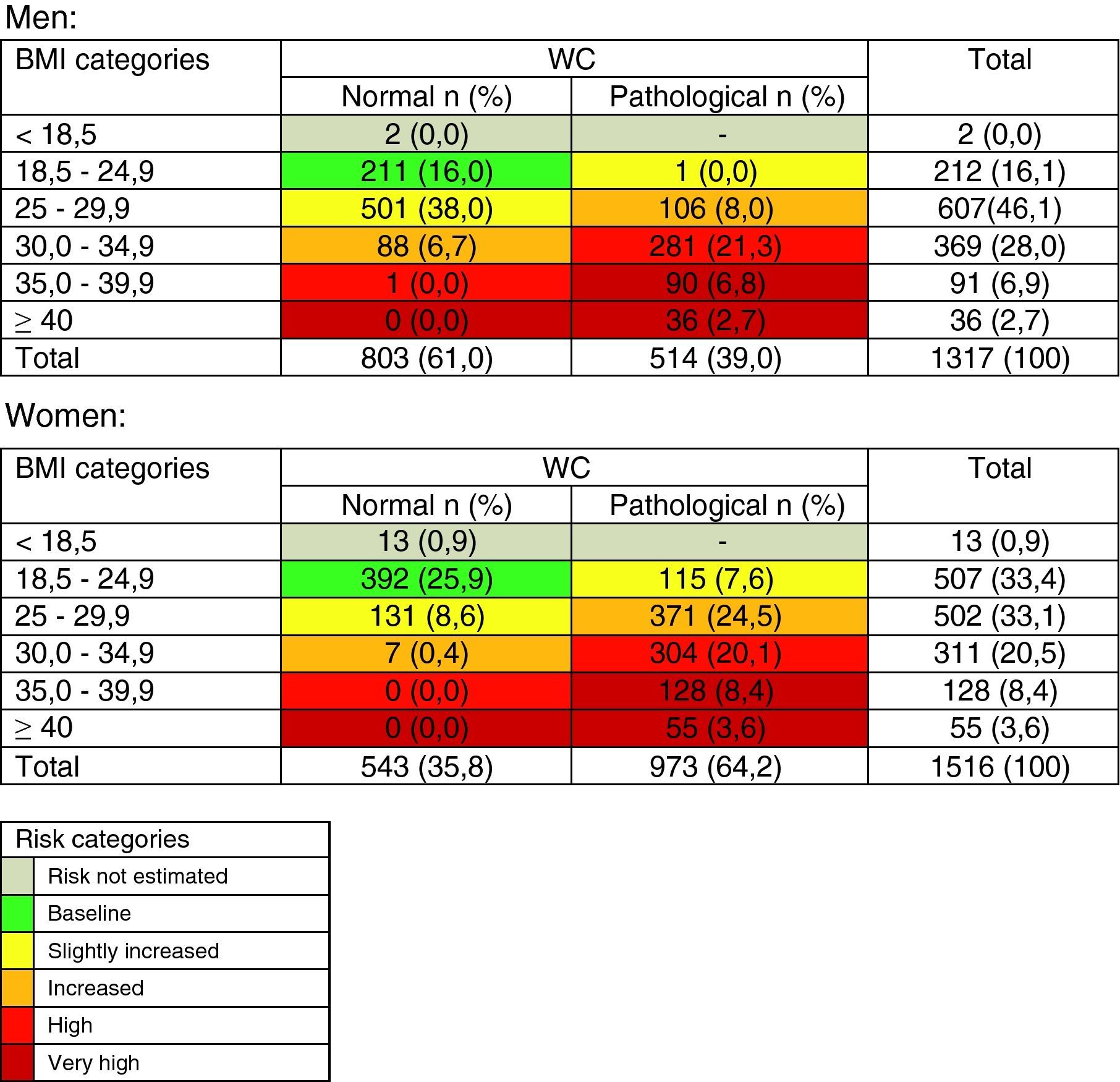
When the sample was categorized based on BMI and WC (Table 2), only 16.0% of men and 25.9% of women had desirable anthropometric measures, while the proportion of subjects exposed to a high and very high risk was higher than 30% in both sexes. A high-risk WC was found in 17.5% of men and 73.9% of women. Morbid obesity was found in 3.2% of the sample.
distribution of the sample by categories of risk of experiencing major cardiovascular complications based on BMI and WC.
BMI: body mass index.
Pathological WC: >102cm in men and >88cm in women.
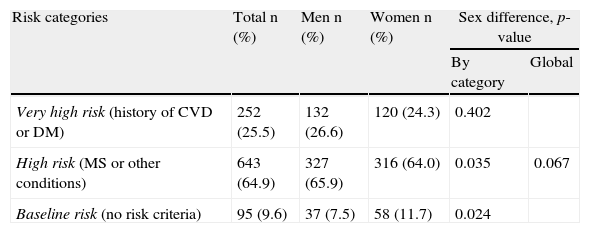
The risk assessed by the association of obesity with certain conditions and comorbidities was considered high and very high in approximately 90% of obese subjects (Table 3).
Distribution of obese subjects based on the assessment of absolute risk of cardiovascular morbidity and mortality proposed by SEEDO.
| Risk categories | Total n (%) | Men n (%) | Women n (%) | Sex difference, p-value | |
| By category | Global | ||||
| Very high risk (history of CVD or DM) | 252 (25.5) | 132 (26.6) | 120 (24.3) | 0.402 | |
| High risk (MS or other conditions) | 643 (64.9) | 327 (65.9) | 316 (64.0) | 0.035 | 0.067 |
| Baseline risk (no risk criteria) | 95 (9.6) | 37 (7.5) | 58 (11.7) | 0.024 | |
DM: diabetes mellitus on drug treatment or basal blood glucose ≥126mg/dL; CVD: history of ischemic heart disease, stroke, arterial revascularization, or lower limb amputation for ischemia; MS: metabolic syndrome.
Other conditions: at least two of the following: family history of early cardiovascular mortality, age less than 65 years in women or 55 years in men, active smoking or quitted smoking less than one year before, BP ≥130/85mmHg, LDL ≥130g/dL, HDL <40mg/dL in men and <50mg/dL in women, TG ≥150mg/dL, impaired basal blood glucose ≥100mg/dL, age ≥45 years in men or ≥55 years or menopause in women.
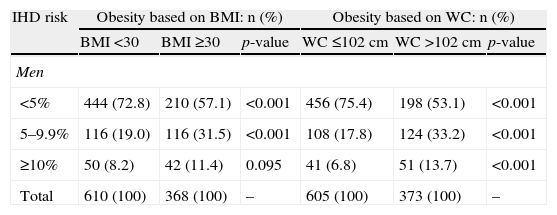
Both obesity and pathological WC were associated with the highest estimated risk of ischemic heart disease in both sexes (Table 4). The prevalence ratio of intermediate and high risk was greater for subjects with pathological WC as compared to obese subjects in both sexes also, although a greater increase was seen in women. In women, obesity was associated with a four- and eight-fold greater prevalence of moderate and high risk as compared to non-obese women, while pathological WC multiplied by 10 the prevalence of intermediate risk and concentrated all high-risk cases (Table 4).
Sex prevalence of ischemic heart disease in the different risk categories by BMI and WC.
| IHD risk | Obesity based on BMI: n (%) | Obesity based on WC: n (%) | ||||
| BMI <30 | BMI ≥30 | p-value | WC ≤102cm | WC >102cm | p-value | |
| Men | ||||||
| <5% | 444 (72.8) | 210 (57.1) | <0.001 | 456 (75.4) | 198 (53.1) | <0.001 |
| 5–9.9% | 116 (19.0) | 116 (31.5) | <0.001 | 108 (17.8) | 124 (33.2) | <0.001 |
| ≥10% | 50 (8.2) | 42 (11.4) | 0.095 | 41 (6.8) | 51 (13.7) | <0.001 |
| Total | 610 (100) | 368 (100) | – | 605 (100) | 373 (100) | – |
| BMI <30 | BMI ≥30 | p-value | WC ≤88cm | WC >88cm | p-value | |
| Women | ||||||
| <5% | 698 (95.1) | 300 (76.1) | <0.001 | 374 (98.7) | 624 (83.3) | <0.001 |
| 5–9.9% | 32 (4.4) | 77 (19.5) | <0.001 | 5 (1.3) | 104 (13.9) | <0.001 |
| ≥10% | 4 (0.5) | 17 (4.0) | <0.001 | 0 (0) | 21 (2.8) | <0.001 |
| Total | 734 (100) | 394 (100) | – | 379 (100) | 749 (100) | – |
IHD: ischemic heart disease; BMI: body mass index; WC: waist circumference.
IHD risk: some sign of ischemic heart disease in the following 10 years according to the Framingham function calibrated for Spain for the population aged 35–74 years with no prior history of cardiovascular disease.
This study shows that obesity and overweight may affect 74.1% of the general population from a healthcare area in the region of Extremadura. If subjects with a pathological WC are added, 78.2% would be at risk based on anthropometric measures only. A higher prevalence of obesity was found in the male population, in contrast to what has traditionally been reported.
The risk of CVD was increased for a vast majority of obese subjects when the methods proposed by the SEEDO were used. The specific risk of ischemic heart disease was higher in women. This high prevalence of obesity with its resultant increase in associated cardiovascular risk may be making this modifiable risk factor the one with the greatest impact on the population, as has already been shown,16 although the figures depend on the origin and methods of each study.17
Overweight, obesity, and cardiovascular risk factorsObesity has been related to an increased prevalence of traditional cardiovascular risk factors in different populations.18,19 In this case, a gradient was also found in both the variables associated with risk and with the prevalence of diabetes and high blood pressure for intermediate stages such as overweight. LDL cholesterol showed no such increase in men, but the characteristic dyslipidemic profile in this population, defined by low HDL cholesterol and elevated triglyceride levels, was seen in both sexes. These metabolic changes appear to be mediated by an underlying insulin resistance and a low-grade chronic inflammatory status. An attempt was made to explore this inflammatory pathway by measuring WBC counts,20 since other mediators that have been related to this situation, such as interleukin-6 or tumor necrosis factor α, were not available.21 In our case, the WBC count gradient was only significant in women. However, another marker dependent on inflammatory activity, in addition to coagulant, such as fibrinogen22 did show this increase with BMI in both sexes. The only risk factor inversely related to BMI was active smoking, mainly because of the presence of a large group of elderly women who had never smoked (data not shown).
Prevalence by ageAge is a variable highly related to obesity, which in our survey increased throughout the age range studied, although its prevalence decreased after 70 years (data not shown). The prevalence rates found in this survey were markedly higher than those reported by the DORICA study,2 conducted more than one decade ago. As an example, the prevalence of obesity in the youngest decade was three times higher in men and two times higher in women. The incidence of obesity was also different depending on sex in our study, as a greater prevalence was found in men until 55 years of age, in contrast to the greater prevalence in women reported in the above study. Finally, the population older than 65 years showed a 20% increase in prevalence as compared to prior studies.23 These differences may only result from the characteristics of the studied area, but it cannot be ruled out that they reflect changes in the epidemiology of the disease.
Obesity, pathological WC, and cardiovascular riskWhile no agreement exists as to which is the best obesity measure related to cardiovascular risk,24 abdominal obesity appears to be better than BMI in this regard,25 although the use of both measures may improve risk estimation.6,9 The use of this classification system showed a very low proportion of subjects, particularly men, with desirable anthropometric measures, so demonstrating an expansion of obesity in its different forms in this sex. A high prevalence of pathological WC was found in women with overweight, a significant finding because overweight may be more sensitive than BMI for risk detection. This was demonstrated when the risk of ischemic heart disease was estimated, for which higher prevalence ratios of intermediate and high risk were seen with WC as compared to BMI. Moreover, higher prevalence ratios of moderate and high risk associated with both variables were also found in women as compared to men. Thus, 70% of women with moderate risk and 81% of those with high-very high risk were obese, as compared to 50% of men at both risk levels. Thus, virtually all cases with moderate and high-very high risk occurred in women with a high WC. This may occur because the risk in men depends to a greater extent on smoking, which is less prevalent in women, and/or because all other traditional risk factors associated with obesity are more prevalent in women, as shown in Table 1.
The comorbidity of obesity with established CVD or diabetes markedly increases cardiovascular risk. Twenty-five percent of obese subjects in this study were in this situation while an additional 65% were at an increasing risk of having metabolic syndrome or other determining factors. As a result, only approximately 10% of obese subjects had none of these risk increasing clinical conditions.
The difference seen between the prevalence of low risk in obese subjects estimated by the Framingham function adapted for Spain (66.9%) and by the SEEDO classification system (9.6%) may be due to:
- •
The estimated risk: the risk of ischemic heart disease using the Framingham function, the total cardiovascular risk using the SEEDO classification system.
- •
The populations assessed: only subjects with no history of CVD aged 35–74 years are assessed with the Framingham function.
- •
The low basal risk of ischemic heart disease in Spain.
- •
The calculation method: using a risk function, calibrated and validated for our country, which estimates the 10-year probability of ischemic heart disease based on traditional risk factors with the Framingham equation and by the association with multiple risk situations shown in the literature using the SEEDO classification system.
All of this makes both estimations difficult to compare, but because of the magnitude of the difference we think it may be due to the high number of risk conditions used in the SEEDO recommendations, which, to our knowledge, have still to be validated.
Difficulties for interventionIn view of the results reported, it may be wondered what intervention measures should be taken and whether individualized care, as proposed by SEEDO, is feasible.9 The main problems we face from the healthcare viewpoint include firstly, the poor motivation of the affected subjects, who are not always aware of the risk of the disease. Primary care healthcare professionals, responsible for initial detection and management, are not always well trained in conducting motivational interviews or in guiding dietary or physical exercise programs. On the other hand, effective and safe drugs for the treatment of the disease are currently lacking. Finally, social and economic determinants do not always favor, and may even prevent, the necessary changes in dietary habits or leisure time physical exercise.26 The solution to this serious public health problem may be far off because of the difficulties listed. This may make it difficult to achieve the optimal control of risk factors, which is far from being achieved,27 and so result in a delay in the reduction of cardiovascular disease in the coming decades.
Therefore, we believe that a comprehensive national plan should be devised, with the collaboration of institutions already created for this purpose,28 in order to address this problem and to design an intervention strategy which will propose the most cost-effective measures. Recommendations should not be simplistic, because many factors which affect individual behavior are beyond the control of the subjects, themselves.29
Study strengths and limitationsThe association found between obesity and all other risk factors cannot be put down to chance because of the cross-sectional design of the study, although plenty of evidence for this association has been reported.18,19 The prevalence rates reported were found in a representative sample from the population of a rural healthcare area in Badajoz. Random sampling and high response rate support the validity of the results. However, these results cannot be extended to the rest of the region or to the whole country, although they were similar to those reported in other regions with cardiovascular mortality figures similar to Extremadura.3 The proportion of subjects considered to have diabetes (23.8%), high blood pressure (26.2%), or hypercholesterolemia (28.5%), was based on the measurement of the parameters defining these conditions on a single day. They had no history of nor were receiving treatment for such diseases, and numbers may therefore be lower. Estimates of risk increase associated with obesity proposed by SEEDO are based on different studies and populations, and risk increase may, therefore, not be of such a magnitude.
ConclusionsWe think that obesity is a highly prevalent risk factor in our environment that already affects, to a greater or lesser extent, the majority of the general population. Obesity is almost consistently associated with an increased risk of CVD, particularly in women. We think that both BMI and WC should be used for better risk assessment. The increasing importance of obesity requires the conducting of cohort studies to measure the extent of this risk. Consideration should also be given to the development and implementation of a comprehensive plan for the prevention and treatment of obesity in order to decrease its eventual consequences for public health in our country.
Funding2004–2007 National Scientific Research Plan (PI 071218), grants to emergent groups (EMER 07/046), grants for research intensification (INT 07/289, 09/030) from I.S. Carlos III, scholarship from the Plan Integral Enfermedades Cardiovasculares de Extremadura. Fundesalud. Extremadura regional government.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Félix-Redondo FJ, et al. Prevalencia de obesidad y riesgo cardiovascular asociado en la población general de un área de salud de Extremadura. Estudio Hermex. Endocrinol Nutr. 2012;59:160–8.