Multiple endocrine neoplasia (MEN) syndromes are characterized by the presence of tumors affecting two or more endocrine glands. Pituitary adenoma (PA) and pheochromocytoma/paraganglioma (Pheo/PGL) are common tumors in MEN type 1 and 2 respectively. The presence of both tumors in a patient is exceptional and was first reported by Iversen in 1952.1 Advances in genetics have suggested a possible common pathogenetic mechanism in which mutations of genes encoding the enzyme succinate dehydrogenase (SDH) could be involved.2,3 In 2015, Xekouki et al. confirmed the existence of this association called “the three P association” or 3PAs: pituitary adenoma with pheochromocytoma/paraganglioma).4 Three cases of this association, one of them partially described previously, are reported below.5
Case 1This was a 54-year-old male with no remarkable family history and with high blood pressure. Bilateral adrenal incidentalomas were diagnosed based on ultrasound examination for erectile dysfunction. Abdominal computed tomography (CT) showed a right adrenal mass 6cm in size and a 2cm nodule in the left adrenal gland. Urinary catecholamine levels were 3488nmol/d (normal range: 116–699), and metaiodobenzylguanidine (MIBG) scintigraphy showed bilateral uptake. There were also acromegalic features, the serum IGF-1 level was 46.4nmol/L (normal range: 8.1–32.8), and the serum GH level was not suppressed after an oral glucose tolerance test (OGTT). Pituitary magnetic resonance imaging (MRI) revealed a 7mm sellar lesion. Bilateral adrenalectomy and subsequent transsphenoidal surgery were performed, and a pathological study diagnosed pheochromocytoma and pituitary adenoma with immunohistochemistry positive for GH and prolactin respectively. A genetic study of RET, VHL, SDHB, and SDHD was negative.
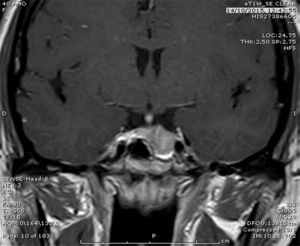
Case 2This was a 38-year-old female with a deletion affecting SDHB exon 1. The index case was her brother, who had undergone surgery for functioning para-aortic paraganglioma. She was initially assessed for menstrual changes and galactorrhea, and was diagnosed with macroprolactinoma (Fig. 1). Treatment was started with cabergoline 1mg/week, which resulted in symptom disappearance and the normalization of serum prolactin. The patient had no high blood pressure or adrenergic symptoms, and serum and urinary catecholamine levels were normal. Because of her family history and the presence of the same deletion as her brother, a CT scan of the neck, chest, and abdomen was performed, showing a right 11mm nodule in the right side of the neck and a hypervascular mass 35×20mm in size in the mediastinum. In OctreoScan®, the lesions expressed somatostatin receptors, which were consistent with paraganglioma. The mediastinal lesion was unresectable because it was too close to vascular structures. Because of the positive findings in scintigraphy and based on its efficacy in some cases,6 treatment was started with somatostatin analogs. The assessment of the therapeutic response is pending. The genetic tests performed on her mother and sister were positive.
Case 3This was a 56-year-old female with no remarkable family history, high blood pressure, and frequent hypertensive crises. The plasma norepinephrine level was 31,656pg/mL (normal range: <300) and the urinary norepinephrine level was 2336μg/d (normal range: <76). Abdominal CT and MRI revealed a 4cm mass in the right adrenal gland and a 1cm nodule in the left gland. MIBG scintigraphy showed right adrenal uptake. Bilateral adrenalectomy was performed at another hospital, and a pathological examination found a right pheochromocytoma and a normal left adrenal gland. The patient had phenotypic traits of acromegaly, a serum GH level of 17.9ng/mL (normal range: <5), a serum IGF-1 level of 839ng/mL (normal range: 94–483), and no serum GH suppression after OGTT. Pituitary MRI revealed a microadenoma, and transsphenoidal resection was therefore performed. Blood chemistry showed hypercalcemia (corrected calcium, 11.3mg/dL) and a serum parathormone level of 87ng/mL (normal range: <65) suggesting primary hyperparathyroidism. Neck ultrasound disclosed a right 16mm nodule and a left 6mm nodule consistent with parathyroid glands, and 99Tc-sestamibi scintigraphy was negative. As the patient was asymptomatic, with calcium levels less than 11.5mg/dL, and had no other criteria for surgery, watchful waiting was decided upon. A study of RET, MEN-1, and VHL showed no mutations.
Enzyme SDH is a protein complex of the mitochondrial membrane involved in the Krebs cycle. SDH consists of four subunits, SDHA, SDHB, SDHC, and SDHD. Changes in those genes inhibit the hydroxylation of hypoxia-inducible factor 1-alpha and cause an accumulation of succinate, which is related to a state of tissue pseudohypoxia and tumorigenesis.7 In addition to Pheo/PGL, SDH gene mutations have been identified in patients with Carney-Stratakis syndrome, renal carcinoma, or Cowden-like syndrome.8,9
In a review of all reported cases of PA and Pheo/PGL,2 mutations related to Pheo/PGL or PA were identified in 21 out of 72 patients. No genetic change could be shown in 23 patients, but there were elements suggesting a hereditary syndrome such as multiple Pheo/PGL, a family history of PA or Pheo/PGL, or an association with another endocrine disease. The remaining 28 patients were found to have no mutation or any other element suggesting hereditary disease. In the latter subgroup, a genetic study was available for only approximately half of the patients.2
Dénes et al.10 published in 2015 a genetic analysis of 39 patients with PA and Pheo/PGL. These authors detected 11 germinal mutations in five different genes: 5 SDHB, 1 SDHC, 1 SDHD, 2 VHL, and 2 MEN1. No mutation was found in 20 patients.
In patients with 3PAs and SDH mutations, PA is usually larger and locally aggressive or refractory to treatment. Most PAs secrete GH or prolactin or are non-functioning. Pheo/PGLs are often bilateral or multiple and have a trend to recurrence.4
The coexistence of bilateral pheochromocytoma and acromegaly suggests a pathogenic relationship between the tumors. An extension of the genetic study is currently ongoing to detect, among others, a MEN1 mutation or a large deletion in MAX, a gene recently involved in cases of Pheo/PGL, where no evidence exists of other known mutations. This could possibly explain the lack of an apparent family history.11 The second patient had a macroprolactinoma, which is uncommon in women of childbearing age and corresponds to the PA phenotype of patients with 3PAs. In case 3, the concurrence of three endocrine diseases suggests a relationship between them, and although they would be within the clinical spectrum of this new association, they could also correspond to MEN type 4. As regards the heterogeneity of the genetic study, it should be noted that the patients attended three different hospitals, and most tests, including the genetic study, were performed before the most recent findings regarding the 3PAs association were available.
In conclusion, the current evidence suggests that SDH mutations are related to pituitary tumorigenesis and a specific tumor phenotype. Patients with multiple Pheo/PGLs, an affected relative, or genetic SDH changes are predisposed to the development of pituitary tumors. In such cases, clinical, hormonal, and radiographic pituitary assessment is required. In the light of our current knowledge, a genetic study should first include the SDHB gene, and then all other subunits of succinate dehydrogenase, VHL, and MEN1. If the results of this study are negative, a test for MEN4 should be performed.
Please cite this article as: Guerrero Pérez F, Lisbona Gil A, Robledo M, Iglesias P, Villabona Artero C. Adenoma hipofisario asociado a feocromocitoma/paraganglioma: una nueva forma de neoplasia endocrina múltiple. Endocrinol Nutr. 2016;63:506–508.