Neurohypophyseal germinomas are rare neoplasms, with slow growth and variable clinical presentation that occasionally complicate their diagnosis in the early stages of the disease. Although the determination of human chorionic gonadotropin (hCG) in serum and cerebrospinal fluid (CSF) may help, definitive diagnosis of these tumors is determined by the histopathological findings. We present two new cases of germinomas with special features that delayed their diagnosis for several years, and a review of the literature on this pathology.
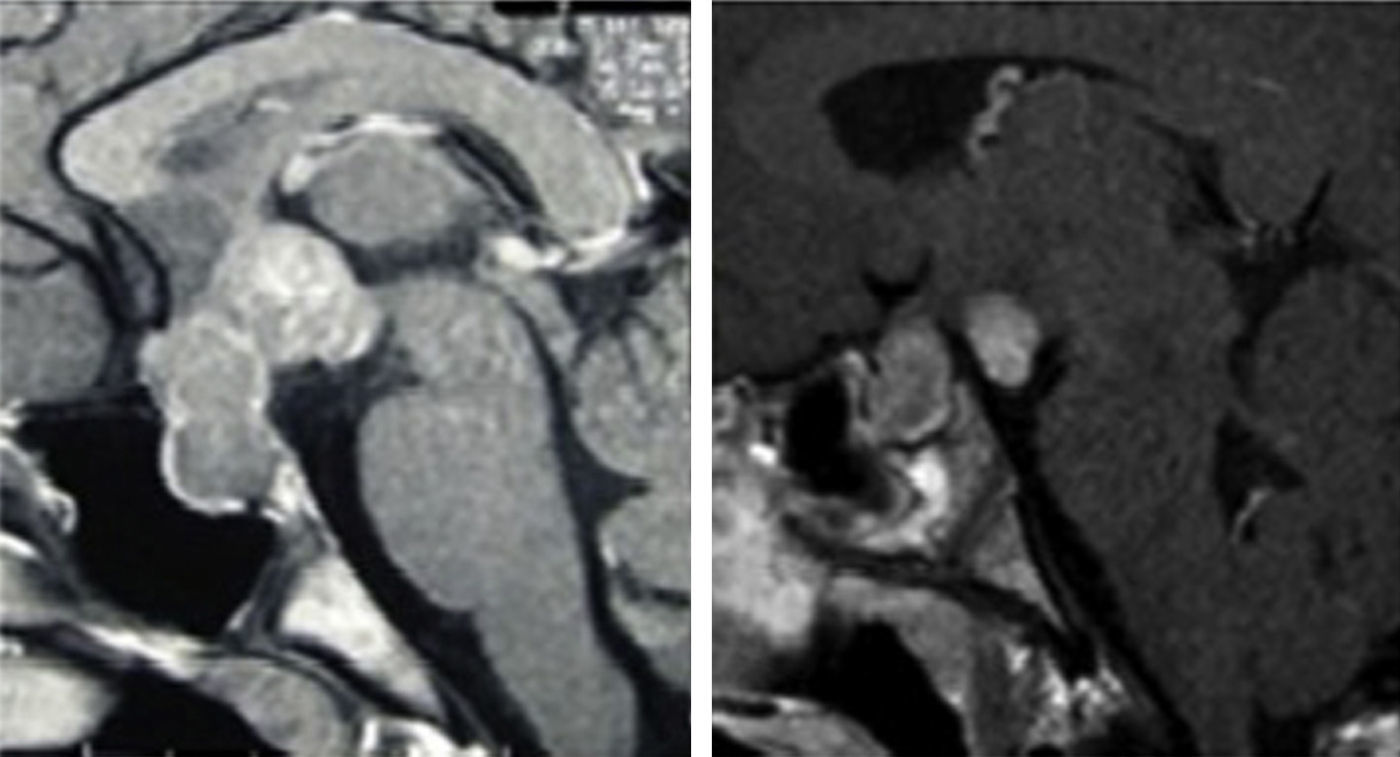
A 14-year-old boy was referred to our department because he presented growth arrest for the previous two years. Seven years before he had been evaluated for an incipient mammary button, and four years ago he had been diagnosed of primary polydipsia. Physical examination emphasized height and weight below the 3rd percentile, button left breast and testicular volume of 6mL. The endocrine study that we performed, revealed anterior panhypopituitarism with hyperprolactinemia: T4L 6.4pmol/L [normal values (nv), 10.3–25.7] TSH 2.44mU/L (nv, 0.38–4.84), baseline cortisol 190nmol/L (nv, 221–690), LH<0.1U/L (nv, 2–13.8), FSH 0.1U/L (nv, 2–13.8), testosterone 8.1nmol/L (nv, 10–35), PRL 28.4μg/L (nv, 4.6–21), GH 1.6μg/L (nv, 0–5), IGF-1 143μg/L (nv, 112–450), and a GH peak after clonidine stimulation test of 1.3μg/L (60min). Given the presence of inappropriate undetectable LH concentrations for the testosterone levels, serum hCG was evaluated, yielding a concentration of 10.9mIU/mL. Brain MRI identified a hypothalamic-hypophyseal mass (Fig. 1). The CSF showed an hCG concentration of 32.6mIU/mL, with a CSF/serum hCG ratio of 2.9. A transsphenoidal biopsy of the lesion was obtained, with confirmation of the diagnosis of neurohypophyseal germinoma.
Hypophyseal MRI findings, Sagittal acquisitions, TI-sequencing after gadolinium contrast injection. Case 1. Hypothalamic-hypophyseal lesion affecting both cavernous sinuses, compression of the optic chiasm and deformation of the third ventricle. Case 2. Thickening of the hypophyseal stalk and enhanced uptake nodule in the tuber cincrcum, measuring 7mm in size.
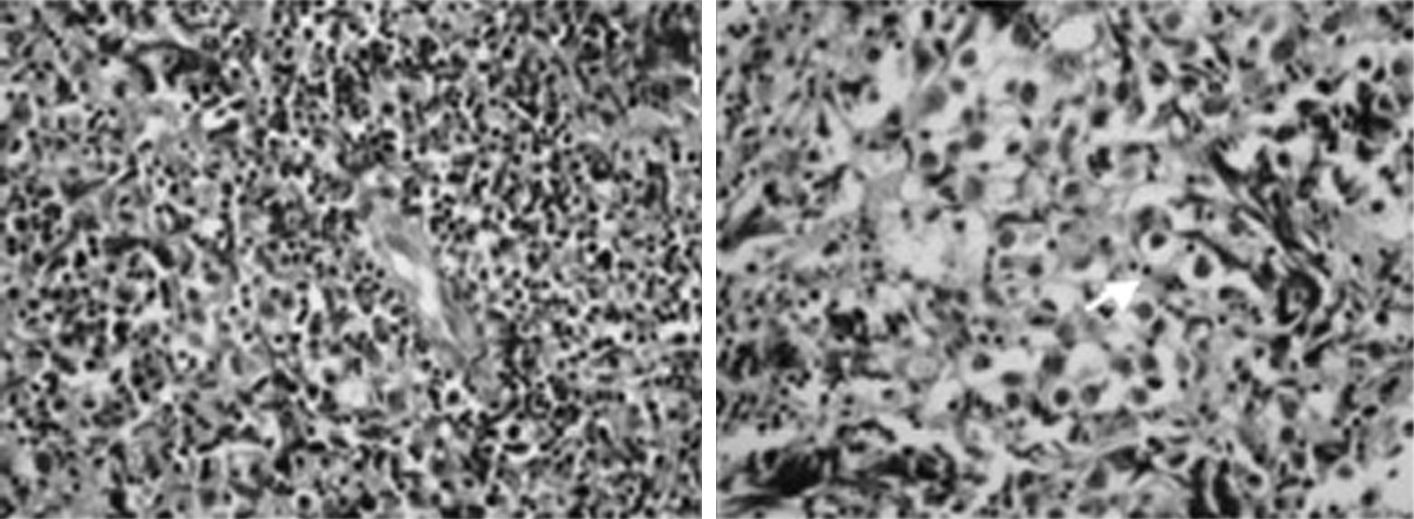
A 10-year-old boy presented with polyuria–polydipsia regarded as corresponding to primary polydipsia. Arrested growth was established after one year of follow-up, and the patient was referred to other hospital where somatotropic deficiency was detected (GH peak after clonidine stimulation test of 3.6μg/L at 60min), along with central diabetes insipidus (dehydration test suspended after 4h due to hypernatremia (155mmol/L) and 3% body weight loss). The brain MRI findings proved normal. Treatment was started with GH and inhalatory desmopressin. After 16 months the patient developed central hypothyroidism and replacement therapy was started. A new pituitary MRI revealed then a thickening of the hypophyseal stalk associated to a 7-mm nodule with enhanced contrast uptake in the hypothalamic tuber cinereum (Fig. 1). GH treatment was suspended. Transsphenoidal biopsy of the sellar component reported lymphocytic hypophysitis. GH treatment was resumed, with the introduction of corticoid therapy for four weeks and a new pituitary MRI was performed showing a progressive enlargement of the hypothalamic lesion and thickening of the hypophyseal stalk. GH treatment and corticoid therapy were suspended and serum hCG was measured proving low but detectable levels: 2mIU/mL. So a second biopsy was performed which again confirmed the diagnosis of lymphocytic hypophysitis (Fig. 2). At this point the patient was referred to our department. We measured hCG levels in serum and CSF with the following results: 7.1 and 23mIU/mL, respectively, so we asked our pathologist to review the pituitary biopsy performed in the referral center. The adenohypophyseal tissue showed a dense mononuclear inflammatory infiltrate with the occasional presence of small granulomas composed of epitheloid histiocytes compatible with lymphocytic hypophysitis. However, of note was the presence of large cells with a vesicular nucleus, a macronucleolus and clear cytoplasm, forming small nests delimited by lymphocytes (Fig. 2). The immunohistochemical study proved positive for c-Kit and placental lactogen, and negative for CD30, thus confirming the biochemical diagnosis of germinoma.
Histological specimen of transsphenoidal biopsy of case 2. Adenohypophyseal tissue showed a dense mononuclear inflammatory infiltrate (left image) with the occasional presence of small granulomas composed of epitheloid histiocytes compatible with lymphocytic hypophysitis. Of note was the presence of large cells with a vesicular nucleus, a macronucleolus and clear cytoplasm, forming small nests delimited by lymphocytes (right image).
Intracranial germ cell tumors represent less than 1% of all intracranial neoplasms, but in children constitute up to 6.5% of such lesions.1 These tumors include germinoma, embryonal cell carcinomas, and teratomas. After the pineal gland, the suprasellar region represents the second most common site of involvement. They are more common in the second decade of life, with a peak incidence between 10 and 14years of age. The lesions originating in the pineal gland are more prevalent in males, while no gender difference in distribution is seen in the lesions appearing in the suprasellar region.2
Among the suprasellar germ cell tumors, the most common lesions are germinomas, followed by teratomas and pinealomas of an ectopic or metastatic nature.2 Neurohypophyseal germinomas may be pure or contain syncytiotrophoblastic giant cells which secrete hCG. Measurement of hCG is an important adjunct method in the diagnostic of germ cell tumors. At high concentrations hCG can be detected in serum, but when the serum hCG levels are low, evaluation of the hormone in CSF may be of help in establishing the diagnosis, since this parameter is more sensitive as an indicator of tumor presence and even can precede to abnormalities on imagen techniques.3–5
The suprasellar germinomas often generate endocrine alterations. Over 90% of patients show clinical evidence of hypopituitarism that can manifest as gonadal dysfunction, secondary hypothyroidism and less frequently, alterations of the corticotropic axis. Children may present lack of sexual development and growth alterations as in our two patients. Neurohypophyseal and stalk dysfunction can manifest as hyperprolactinemia (symptomatic or otherwise), or as diabetes insipidus. The latter is observed in about 80% of all cases and may constitute an early finding. As an antecedent, our two cases were initially diagnosed with “primary polydipsia”. Other potential symptoms are vision disturbances, including field defects or optic atrophy, hypothalamic manifestations, hydrocephalus, or symptoms of intracranial hypertension.3
In the MRI studies, thickening of the hypophyseal stalk is the most common finding, together with the loss of neurohypophyseal hyperintensity in T1-weighted sequences, in which the lesion appears isointense or slightly hypointense with respect to the normal hypophysis. After gadolinium contrast injection, uptake is less pronounced than in the normal hypophysis.5
The imaging findings are not specific and the differential diagnosis fundamentally must be established with tuberoinfundibular lymphocytic hypophysitis.6 Since this disorder is infrequent in childhood, histological findings compatible with a lymphocytic inflammatory process can represent the first sign of a host reaction to occult germinoma, as illustrated in our second patient. This would justify the determination of hCG in CSF in all prepubertal patients with a presumed or histological diagnosis of lymphocytic hypophysitis, as well as the immunohistochemical study of the histological specimen with the determination of placental lactogen, c-Kit and CD30.7
As regards the treatment of intracranial germinomas, combined chemotherapy–radiotherapy has been the standard approach. However in non disseminated intracranial germinomas, the irradiation of the whole ventricular system without chemotherapy could be sufficient, as recent articles have shown that focal radiotherapy plus chemotherapy were associated with inferior control of these tumors, and a higher incidence of chemotherapy related toxicities.8-10
The prognosis of these tumors is dependent upon the histology, but also upon the size of the tumor and the extent of the disease at the time of diagnosis. An early diagnosis is key to treat such tumors before the hypothalamic-hypophyseal damage proves irreversible or adjacent structures suffer compression or metastatic disease became apparent.