To assess in hospitalized patients the prevalence of hyperglycemia, degree of glycemic control, rate of hypoglycemia, and treatment used.
Patients and methodsA prospective, observational study.
ResultsHyperglycemia was found in 185 (26.7%) of 691 patients, of whom 85% had been diagnosed with diabetes and 15% had no diabetes. Preprandial mean blood glucose was 169mg/dL (95% CI 160–177). Control goals were achieved by 34.5% of patients (blood glucose ≤140mg/dL).
In 121 patients only sliding-scale regular insulin was used, while 64 patients received both basal and regular insulin. The mean daily insulin dose used was 19.5units. Oral antidiabetics were given to 11.4% of patients. Thirteen patients (7%) experienced hypoglycemia (<70mg/dL), none of them severe.
ConclusionsGlycemic control is not adequate in hospitalized patients, probably because of overuse of sliding scales and the low insulin doses used.
Conocer la prevalencia de hiperglucemia en pacientes ingresados, el grado de control glucémico, la tasa de hipoglucemias y el tratamiento utilizado.
Material y métodosEstudio observacional de corte transversal.
ResultadosDe 691 pacientes, 185 (26,7%) tenían hiperglucemia, 85% eran diabéticos conocidos y 15% no. La glucemia capilar media preprandial fue de 169mg/dl, (160-177, IC 95%). El 34,5% de los pacientes alcanzaron objetivos de control (glucemias ≤140mg/dL).
En 121 pacientes se utilizó solo insulina rápida (pauta móvil), en 64 se utilizó insulina basal e insulina rápida. La dosis media de insulina utilizada es de 19,5U/día. En el 11,4% se utilizaron antidiabéticos orales. Trece sujetos (7%) tuvieron hipoglucemia (< 70 mg/dL), ninguno sufrió hipoglucemia severa.
ConclusionesEl control glucémico de los pacientes ingresados no es bueno y esto se debe probablemente a la sobreutilización de pautas móviles y a las bajas dosis de insulina utilizadas.
Hyperglycemia in hospitalized patients has been associated with increased morbidity and mortality, mean stay and costs, both in known and unknown diabetics.1–4
In 2009 the latest consensus of the American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE)5 established glycemic control targets for noncritical inpatients: a preprandial blood glucose value less than 140mg/dL and a random blood glucose value less than 180mg/dL. These targets are less stringent than those proposed in the Spanish consensus document6 for the same type of patient: preprandial blood glucose levels<130mg/dl and postprandial blood glucose level<180–200mg/dL.
There are no published studies in our setting investigating the prevalence of hyperglycemia in noncritical hospitalized patients and its degree of control.
The aim of this study was to determine the prevalence of hyperglycemia in adult patients admitted to the medical and surgical wards of a teaching hospital as well as the prevalence of known diabetes, to determine the degree of glycemic control during hospitalization and routine metabolic control, the rate of hypoglycemia, and finally to investigate the insulin therapy regimens used during hospitalization.
Materials and methodsA cross-sectional observational study was carried out on March 9 and 18, 2010, reviewing the clinical records of all noncritical adult inpatients at the Hospital Universitario Príncipe de Asturias (HUPA). All adult patients admitted over 48h to one of the following departments were entered into the study: Internal Medicine, Cardiology, Gastroenterology, Pneumology, Neurology, Nephrology, General Surgery, Urology, Traumatology, ENT, Oncology, Rheumatology, and Endocrinology. Patients from the departments of Obstetrics and Gynecology, short stay unit, intensive care unit, psychiatric unit and pediatric unit were excluded.
The medical records of patients diagnosed with diabetes mellitus (DM) prior to admission with a baseline hyperglycemia≥127mg/dL on at least 2 occasions or random blood glucose>200mg/dL during hospitalization were reviewed and the capillary blood glucose records were analyzed; those performed during the 3 days prior to the study were being collected. Due to the small number of patients in whom postprandial glucose measurements were performed, only preprandial capillary glucose values were considered for the analysis.
Insulin regimens were recorded, as well as the mean daily dose, if they continued to receive treatment with oral antidiabetics, with corticosteroids, and if they were given enteral or parenteral nutrition. The number of subjects with recorded hypoglycemia in the previous 3 days was recorded, hypoglycemia being considered as a capillary glucose level<70mg/dL. The laboratory test database of Health Area 3 of Madrid, which is centralized in the HUPA Laboratory, was reviewed from six months before admission or during hospitalization, and HbA1c measurements of patients were collected. HbA1c was determined by high-performance liquid chromatography and the reference normal range was 4.27–6.07%.
For the analysis, two groups were considered, according to the degree of control: good control (GC) if mean preprandial capillary blood glucose≤140mg/dL and poor control (PC) if blood glucose>140mg/dL according to the criteria of both the ADA and the AACE.5 Treatments were classified as including some basal insulin (NPH, glargine or detemir) and also rapid insulins, the B+R group, vs those treated exclusively with rapid-acting insulins or sliding scale regimens, the R group.
The data were collected and processed using the Excel database (Microsoft Office 2003) and analyzed using the SPSS version 15.0 statistical package. Qualitative variables were expressed in absolute and relative frequencies, n (%), and quantitative variables as mean (SD) and 95% confidence interval (95% CI).
To analyze the characteristics of glycemic control, possible differences were sought between the GC and PC groups. The Chi-square test was used to study the associations between qualitative variables, and the Mann–Whitney test to study the associations between quantitative variables, since numerical variables did not follow a normal distribution. In those variables showing significant differences, p<0.05, the OR (95% CI) of having PC vs GC was calculated. Multivariate logistic regression was performed to weigh the influence of these variables on the degree of glycemic control.
As this was an observational study, informed consent was not requested from the patients. All data were treated anonymously and confidentially.
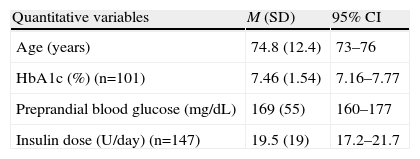
ResultsDuring the 2 days on which the observational study was conducted, 691 patients were admitted to the wards selected for the study, 185 of whom (26.7%) had hyperglycemia during admission. Of these, 147 (85%) of patients had a previous diagnosis of diabetes and 28 (15%) were not known diabetics. Table 1 shows the overall results of the subjects included in the study.
Overall results of study subjects (n=185).
| Quantitative variables | M (SD) | 95% CI |
| Age (years) | 74.8 (12.4) | 73–76 |
| HbA1c (%) (n=101) | 7.46 (1.54) | 7.16–7.77 |
| Preprandial blood glucose (mg/dL) | 169 (55) | 160–177 |
| Insulin dose (U/day) (n=147) | 19.5 (19) | 17.2–21.7 |
| n | % | |
| Qualitative variables | ||
| Sex (male) | 109 | 59 |
| Previous known diabetes | 157 | 85 |
| Corticosteroid use | 14 | 7.6 |
| Treatment regimen | ||
| Basal+rapid (B+R group) | 64 | 35 |
| Only rapid (R group) | 121 | 65 |
| Required insulin | 147 | 79.5 |
| Use of oral antidiabetics | 21 | 11.4 |
| Degree of glycemic control | ||
| Good control (preprandial capillary blood glucose≤140 mg/dL) | 64 | 34.5 |
| Poor control (preprandial capillary blood glucose>140 mg/dL) | 121 | 65.5 |
| Preprandial capillary blood glucose>200 mg/dL | 41 | 22 |
| Patients with hypoglycemia (capillary blood glucose<70 mg/dL) | 13 | 7 |
Quantitative variables are expressed as mean (M) and standard deviation (SD) and 95% confidence interval (95% CI). Qualitative variables are expressed as absolute frequency (n) and relative frequency (%).
Only the results of preprandial blood glucose levels are shown since few subjects underwent postprandial blood glucose measurements, the most common practice being to measure three preprandial capillary blood glucose levels daily.
Mean capillary blood glucose on the 3 days was 169mg/dL (95% CI 160–177), with only 64 subjects (34.5%) belonging to the GC group with preprandial capillary blood glucose≤140mg/dL.
The insulin regimen most used to manage patients was the sliding scale regimen or only rapid insulins (R), 121 subjects (65%), compared to the basal and rapid insulin regimen (B+R) used by 64 subjects (34.5%). The mean insulin dose used was 19.5U/day.
Only a small proportion of subjects, 21 (11.4%), were treated with oral antidiabetics (12 metformin and 9 secretagogues), combined or not with insulin therapy.
Thirteen subjects (7%) had mild hypoglycemia; none had severe hypoglycemia.
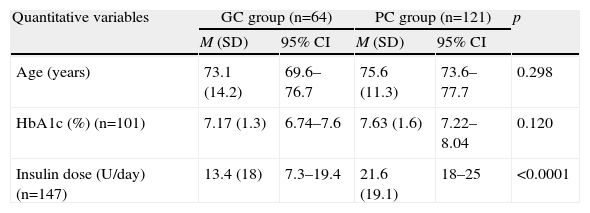
Analysis of the study variables (Table 2) according to the degree of glycemic control showed differences between the two groups, GC and PC, in the use of insulin, the insulin regimen used and insulin dose. Thus, poor glycemic control during admission was associated with an OR of 1.57 (95% CI 1.26–1.95) for use of insulin, 2.07 (95% CI 1.22–3.51) for the B+R vs R regimen, and 2.26 (95% CI 1.26–4.04) for insulin dose (calculated from >15U/day vs <15U/day). No differences were found in the other variables or in the presence of DM prior to admission. The multivariate logistic regression analysis only showed statistical significance for the insulin dose used and not for the insulin regimen, with an OR of 3.06 (95% CI 1.45–6.44) for the use of ≥15U/day vs <15U/day.
Analysis of the results between groups: good control (GC) vs poor control (CM) of study subjects (n=185).
| Quantitative variables | GC group (n=64) | PC group (n=121) | p | ||
| M (SD) | 95% CI | M (SD) | 95% CI | ||
| Age (years) | 73.1 (14.2) | 69.6–76.7 | 75.6 (11.3) | 73.6–77.7 | 0.298 |
| HbA1c (%) (n=101) | 7.17 (1.3) | 6.74–7.6 | 7.63 (1.6) | 7.22–8.04 | 0.120 |
| Insulin dose (U/day) (n=147) | 13.4 (18) | 7.3–19.4 | 21.6 (19.1) | 18–25 | <0.0001 |
| Qualitative variables | n | % | n | % | p |
| Sex (male) | 40 | 62.5 | 69 | 57 | 0.472 |
| Previous DM | 54 | 84.4 | 103 | 85.1 | 0.892 |
| Corticosteroid use | 4 | 6.3 | 10 | 8.3 | 0.622 |
| Treatment regimen | |||||
| Basal+rapid (B+R group) | 13 | 20.3 | 51 | 42.1 | 0.003 |
| Rapid (R group) | 51 | 79.7 | 70 | 57.9 | |
| Required insulin | 37 | 57.8 | 110 | 91 | <0.0001 |
| Use of oral antidiabetics | 9 | 14.1 | 12 | 9.9 | 0.398 |
| Patients with hypoglycemia (capillary blood glucose<70mg/dL) | 5 | 7.8 | 8 | 6.6 | 0.761 |
Quantitative variables are expressed as mean (M) and standard deviation (SD) and 95% confidence intervals (95% CI) and qualitative variables as absolute frequency (n) and relative frequency (%).
Likewise, there were no differences in the rate of hypoglycemia between the two control groups.
Interconsultation was only requested with the Department of Endocrinology of the hospital in 15% of the patients with hyperglycemia.
DiscussionIn this study, the prevalence of hyperglycemia in hospitalized patients was somewhat lower than that previously reported (38% and 31%) in two hospitals of similar characteristics to ours in the US1,7 probably because of the lower prevalence of type 2 diabetes in our setting.
The degree of blood glucose control was not good, as 66% patients of patients were above treatment targets on the 3 days prior to the study: almost a quarter (22%) of patients had mean blood glucose levels over 200mg/dL, a percentage a little lower than in the study of Knecht et al.8 and Wexler et al.,9 both performed in a patient sample similar to our own.
The sliding scale regimen was the most commonly used regimen in the hospital despite its use5,6,10 not being recommended since it does not cover basal insulin needs, promotes episodes of hyperglycemia and hypoglycemia, and has shown poorer control in patients receiving it as the sole regimen.
While only one clinical trial11 conducted in 130 hospitalized patients has shown better glycemic control in patients with basal-bolus insulin therapy (using insulin glargine and glulisine) vs a sliding scale regimen, the recent consensus of the ADA5 and of several Spanish scientific societies6 proposes basal-bolus therapy as the optimum insulinization regimen for noncritical hospitalized patients.
Only in 64 (35%) of the patients were some type of basal insulin and rapid insulin used, suggesting that the recommendations given in this consensus have not been disseminated sufficiently among the different hospital departments.
The fact that mean preprandial blood glucose was higher in the group of patients with a more rapid basal regimen than in patients with only the sliding scale regimen probably indicates that basal insulin was only added to patients with poorer glycemic control or who had had more intensive regimens prior to admission and were patients with more difficult previous control. However, the multivariate regression analysis showed that only the insulin dose used was associated with an increased risk of poor control and that the type of regimen explains to a lesser extent the degree of control observed.
As this was an observational study, the association detected between the basal-bolus regimen and poorer control must not be interpreted as a cause–effect relationship, but rather as a result of the need for more intensive treatment for patients with higher blood glucose levels, a hypothesis supported by the fact that only the insulin dose in the multivariate study reached statistical significance, with more insulin being used in those who were worse controlled.
Another limitation of the study is that its cross sectional design prevented us from knowing the course of blood glucose in patients in whom basal insulin was added.
The mean insulin dose per day was very low (19.5U/day). This may be one of the underlying causes of poor glycemic control. In other observational studies, mean insulin doses were also low.7 The dose was low due to the use of only sliding scale regimens and the low doses used in the insulin dose titration algorithms.
The mean doses used in the only clinical trial11 comparing basal-bolus regimen vs sliding scale regimen in hospitalized patients were much higher in patients with basal-bolus therapy (43U/day) than in patients with sliding scale regimen only (12.5U/day).
We think that both facts, excessive use of the sliding scale regimen and the low insulin doses used, contributed to the high proportion of patients with poor glycemic control in this study.
The confirmed hypoglycemia rate was 7%, a difficult finding to compare with other observational studies due to the paucity of published data and the possibility that it was underestimated owing to the observational design of this study.
The analysis of our data did not find significant differences in the rate of hypoglycemia according to the insulin regimen used. In two clinical trials in inpatients, no significant differences were found in the hypoglycemia rate between basal-bolus therapy and a sliding scale regimen11 or between basal-bolus therapy and premixed insulin.12
The use of oral antidiabetics during hospitalization has also not been recommended in recent consensuses5,6 because of their lack of flexibility, slow onset of action and potential adverse effects, which may be greater in hospitalized patients. This recommendation is also not sufficiently known because 11.4% of patients continued receiving treatment with oral antidiabetics during admission.
Although HbA1c determination was only available in 101 patients (55%), the mean value of 7.6% suggests that metabolic control may have been adequate given the mean patient age (74 years) and presumably high associated comorbidity.13
The degree of control was very similar to that previously reported by a group of diabetic patients over 36 years of age (HbA1c 7.6±1.4%) in our health area,14 and to that reported in another area of similar characteristics.15
Having a recent HbA1c value for known diabetics is useful and it should be measured in all patients on admission,6,13 since achieving a lower blood glucose level during admission in patients with generally good metabolic control and reconsidering treatment at discharge of patients with previous poor control have been proposed as objectives.
In known nondiabetic patients with hyperglycemia on admission, HbA1c may help classify patients16: HbA1c greater than 6.5% probably indicates previously undiagnosed diabetes; in this case starting treatment on discharge would be indicated. If HbA1c is less than 6.5%, it is probably a case of stress hyperglycemia that will be resolved with the clinical improvement of the patient.
The low number of interconsultation requests to Endocrinology in our hospital (15%) probably reflects the low importance attributed to optimum control of blood glucose levels during admission.
In summary, in this study we found that glycemic control in noncritical patients admitted to this hospital was not good, as nearly 2/3 of patients were outside the treatment targets. This was probably contributed to by overutilization of sliding scale regimens and the low insulin doses used. We recommend a more effective dissemination of the latest consensuses on the management of hyperglycemia during hospitalization among the clinicians involved, along with the removal of any barriers that may prevent their implementation.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please, cite this article as: Botella M, et al. Control glucémico en pacientes hospitalizados no críticos. Endocrinol Nutr. 2011;58:536–40.