Thyroid gland infection is a very uncommon condition, as the thyroid gland is extremely resistant to infection. This has been attributed to its high vascularization, lymphatic drainage, the presence of high iodine levels in tissue, the fact that hydrogen peroxide is generated inside the gland as a requirement for thyroid hormone synthesis, and its normal encapsulated location far from external structures (all of which have bactericidal effects).1
The most common etiological agents are microorganisms which are able to colonize oral mucosa and continue to the thyroid gland, especially Gram-positive bacteria such as streptococci and staphylococci, or anaerobic bacteria.2
Despite being unusual, it is a potentially curable disease with an excellent prognosis because of the current availability of antibiotics to cure it.3
A 57-year-old female patient attended the emergency room for pain and inflammation in the right subacromial region which worsened with arm motion and was associated with progressive dysphagia. She had no infectious signs, nor symptoms of hypothyroidism or hyperthyroidism. She reported no skin lesions. The condition had started one week before with fever up to 39°C, which subsided at two days. Her medical history was unremarkable.
A physical examination revealed a right cervical mass extending to the infraclavicular region which was tender, erythematous, and not indurated.
Supplemental tests showed 14,600 WBCs, with 87% neutrophils, and a C-reactive protein level of 43.8mg/dL. Serologic tests for HBV, HCV, HDV, and HIV were negative. Levels of all other parameters, including thyroid hormones, were clinically irrelevant.
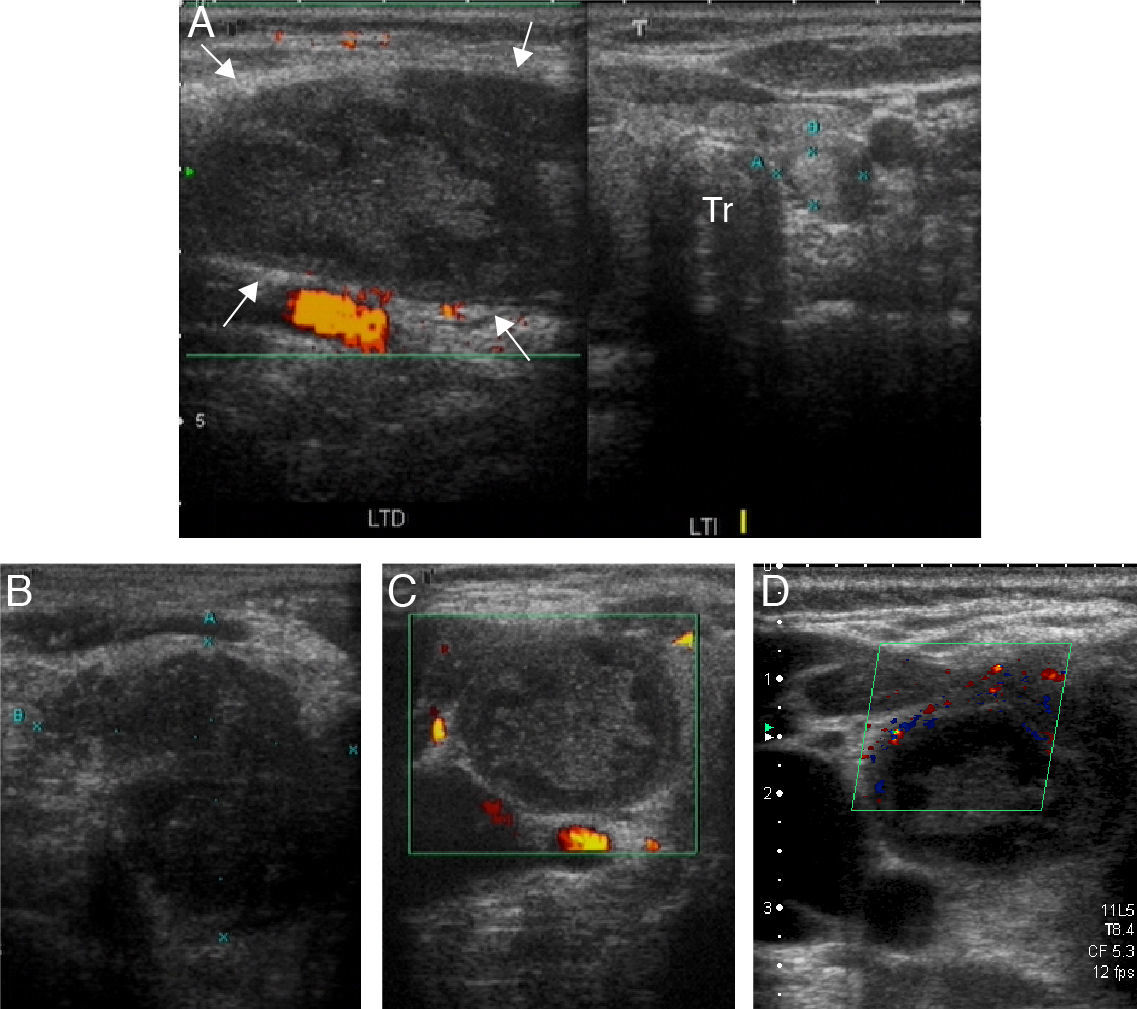
Chest X-rays showed right anterosuperior mediastinal widening, with an endothoracic growth component that displaced the trachea to the left of the midline. A neck ultrasound revealed a heterogeneous, hypoechoic enlargement of the right thyroid lobe with an endothoracic growth component and a hypoechogenic, avascular solid nodular lesion 5.0cm×3.5cm in size. There was also homogeneous infiltration of the right cervical musculoaponeurotic planes, with no adenopathies. The left thyroid lobe was of normal size, with a solid nodule Image 1.2cm×1.0cm in diameter in its lower pole (Fig. 1).
Neck ultrasound: (A) panoramic study of the thyroid gland, with image summation, showing gland enlargement at the expense of the right thyroid lobe (RTL), which has an altered echostructure with a hypoechoic nodular lesion which appears to infiltrate the cervical muscle planes (white arrows). An isoechoic nodule is also seen in the left thyroid lobe (LTL). Tr: trachea. (B–D) B-mode, power Doppler, and color Doppler. Detail of hypoechoic mass, approximately 50mm×37mm in size, with no internal vascularization but discrete peripheral vascularization.
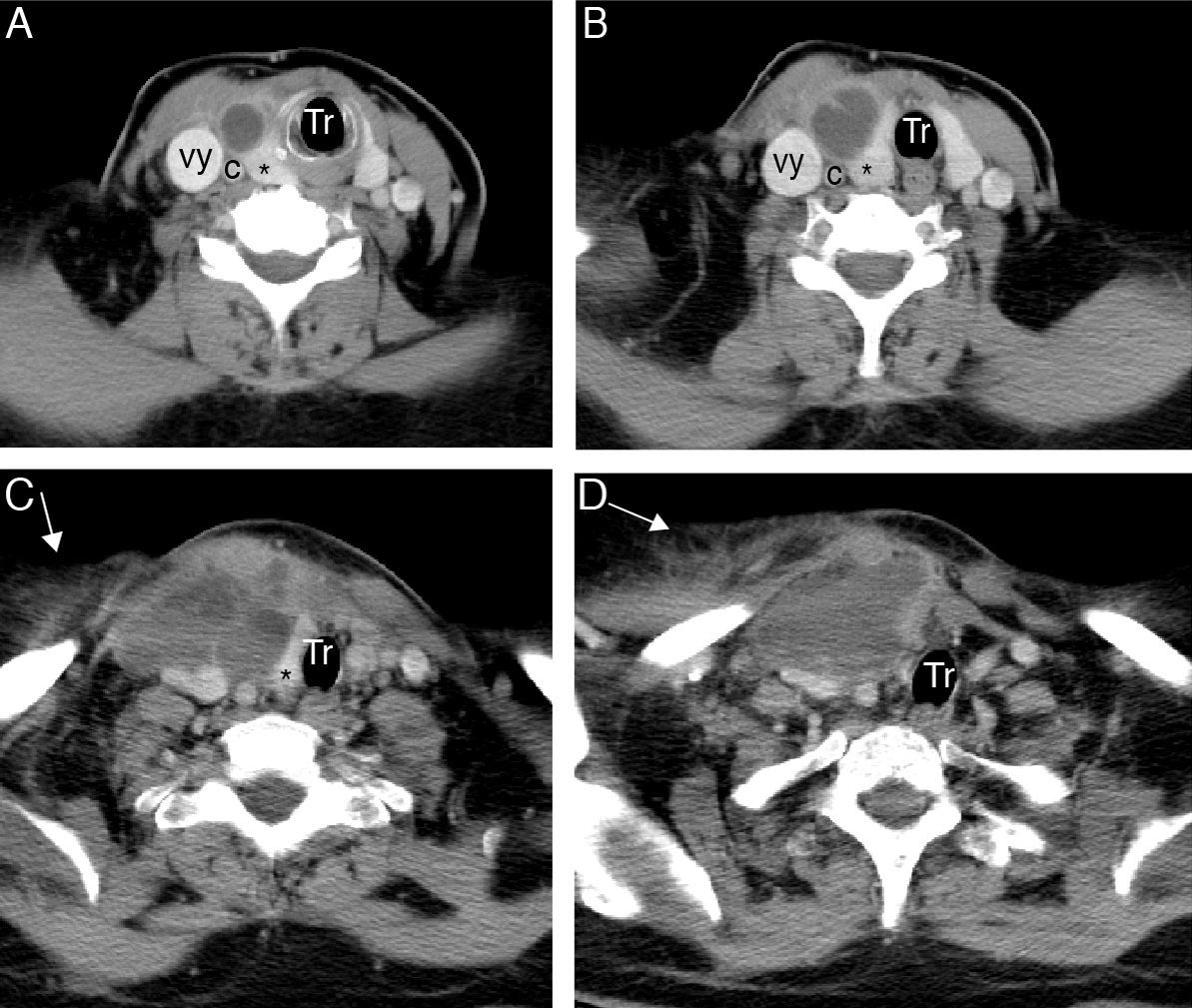
The patient was admitted to the endocrinology department. A CT scan of the neck showed findings consistent with a right cervical phlegmon-abscess extending to the anterior chest wall and mediastinum and dependent on the right thyroid lobe (Fig. 2).
Axial CT images following intravenous administration of iodinated contrast. (A and B) Occupation of right cervical space by mass with cystic density and ill-defined contours, intimately related to the right thyroid lobe (*), and showing heterogeneous uptake of contrast medium, with peripheral enhancement. (C and D) Rarefaction of fat in cervical planes with extension of the process to the right pectoral region, where thickening of the greater pectoral muscle is seen (arrows). This mass displaces the trachea to the left, and right supra-aortic trunks posteriorly (c: right carotid artery; Tr: trachea; vy: right jugular vein).
In the emergency room, the thoracic surgery department performed surgical drainage, and oxacillin-susceptible Staphylococcus aureus was found in exudate culture. Two peripheral blood cultures were also positive for the same germ, and initial antibiotic therapy with vancomycin was therefore replaced by cloxacillin.
Abdominal CT and a bone scan were requested to find out the origin of the septic embolisms of the microorganisms, with negative results.
The patient is currently pending evaluation of the nodule in the left thyroid lobe, but is asymptomatic.
Thyroid gland infection is usually due to the direct extension of an infectious process occurring in an internal fistula of the piriform sinuses.4 These sinuses represent the course of migration of the last branchial arch from its embryonic origin in the fifth pharyngeal pouch. This type of fistula extends from the pharynx to the thyroid gland capsule and most often occurs on the left side. It is very frequently found in children with recurrent purulent thyroiditis.
Other routes through which the thyroid gland may become infected include the presence of a thyroglossal duct remnant, hematogenous dissemination,5 direct extension from an adjacent site, esophageal perforation, or fine needle thyroid puncture.6 Multinodular or adenomatous goiter is a common finding in the reported cases of adults with suppurative thyroiditis. In other adult series, approximately one fourth of patients were immunocompromised.7 Half of these were HIV-infected patients, in whom fungal infections are more common.
In our patient a blood-borne infectious site with no apparent origin was found after an extension study.
Virtually any bacterium may infect the thyroid gland,8 including pneumococci, Salmonella, Klebsiella, Bacteroides, Treponema pallidum, Pasteurella spp, and mycobacteria. Some organisms may cause chronic or insidious infection, particularly in patients with HIV disease. These include Mycobacterium tuberculosis, atypical mycobacteria, Aspergillus spp., Coccidioides immitis, Cryptococcus neoformans, Histoplasma capsulatum, Candida spp., Treponema pallidum, Echinococcus spp., and Pneumocystis carinii.
The dominant clinical symptom is pain in the thyroid gland region, with a subsequent increase in thyroid size and temperature. Our patient also reported dysphagia, but had no other symptoms such as hoarseness, sore throat, or dysphonia.9 Local lymphadenopathies were not found either. When faced with this presentation, a neoplastic condition must be ruled out. As occurred in our patient, thyroid infection most commonly occurs in autumn and winter, usually after upper respiratory tract infections.
Thyroid function tests showed no changes, as usually occurs in cases of pyogenic thyroiditis.
Thyroid gland ultrasound for fine needle aspiration is the initial imaging test of choice for diagnosis.
A CT scan may be of value for abscess site identification, but this is only required in exceptional cases.
Empirical treatment should be started with broad spectrum parenteral antibiotic therapy based on suspected diagnosis after radiodiagnosis.10 Surgical exploration should be performed in all patients in whom anatomical changes such as piriform sinus fistula or a thyroglossal duct remnant are found. Surgical drainage should be performed whenever imaging tests show the presence of intraglandular abscess or gas formation. If necrosis occurs or infection persists despite adequate antibiotic therapy, thyroid lobectomy will be required.3
Although 14 days of antibiotic therapy are sufficient to treat pyogenic thyroiditis, treatment prolongation up to four weeks is advised when bacteremia is found.
In conclusion, pyogenic thyroiditis is a very uncommon condition usually occurring in patients with thyroid diseases, piriform sinus fistula and, especially, with immunosuppression. Our patient did not meet any of these characteristics, which makes the case even more unusual.
Please cite this article as: Barbero Alonso S, et al. Presentación atípica de tiroiditis aguda supurada en paciente inmunocompetente. Endocrinol Nutr. 2013;60:211–3.