The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study showed that to improve the degree of metabolic control in patients with type 1 diabetes mellitus (T1DM) using intensive treatment with any insulin therapy (subcutaneous multiple daily insulin injections [MDI]; continuous subcutaneous insulin infusion [CSII]), frequent daily measurements of capillary blood glucose are needed, and this information should be used for any changes required in treatment. Although glucometers have been constantly improved in recent years, so that they are increasingly faster and more accurate and need less blood, intermittent blood glucose measurements provide no information regarding the magnitude of fluctuations or the velocity or direction of changes occurring over time.
MiniMed (Northridge, CA) marketed in 1999 the first device for continuous glucose monitoring (CGM), the retrospective analysis Continuous Glucose Monitoring System, and later the Continuous Glucose Monitoring System Gold. Although these devices did not allow for real-time glucose measurements, the results could be retrospectively analyzed by professionals and be used to make changes in treatment. These Holter-like devices are known as retrospective continuous glucose monitoring systems intended for professional use. However, although these devices have become a standard working tool in endocrinology departments, there is no adequate scientific evidence showing that their intermittent use is associated with improved blood glucose control.
On the other hand, other devices able to continuously show glucose levels and to inform on trends, and which allow for programming alarms of different types, have been available for some years now. Such devices are called interactive or real-time CGM (RT-CGM) systems.
RT-CGM systems allow integration with CSII to form so-called integrated CSII-CGM systems (sensor-augmented pump [SAP] systems). This integration has for the first time made possible the design of equipment that automates functions based on information from RT-CGM. Examples of such equipment include systems that stop insulin infusion when blood glucose levels below a preset threshold are detected and, more recently, when a low preset value is predicted.
Contrary to that which occurs with retrospective information systems, since 2006 there has been an exponential increase in reports showing the efficacy of RT-CGM for improving the control of patients with T1DM. In summary, the use of these systems is associated with HbA1c decreases of approximately 0.3–0.6%, which are the greater the higher the baseline HbA1c, and the greater the frequency of use of the sensor, with a reduction (or no increase) in the frequency and severity of hypoglycemic episodes and a general improvement in quality of life perceived by the patients. In addition, although most studies compare RT-CGM to isolated CSII systems, it may be added that recent evidence is available of marked improvements in the metabolic control of patients on treatment with MDI in whom a device of this type is also used.
In observational studies, the integrated system that suspends insulin infusion when hypoglycemia is predicted has been shown to be clinically effective in preventing hypoglycemia and decreasing the frequency of both hypoglycemia and hyperglycemia. In addition, it has been shown to be effective in maintaining stable blood glucose levels after the automatic suspension of insulin infusion.
Improvements in the precision and reliability of these systems have affected the prospects for this technology. Thus, in 2016 the US Food and Drug Administration approved a device which was authorized to take decisions (including insulin dose adjustments) without requiring the results to be checked by capillary blood glucose measurements.
On the other hand, the use of this technology is seriously limited by its cost and by the fact that it is not currently reimbursed by the Spanish National Health System (SNS). Despite technical advances and a price reduction for CGM systems, these are only reimbursed in some neighboring countries.
The indications for the use of RT-CGM most commonly accepted in the different international clinical guidelines include recurrent or inadvertent hypoglycemia in patients with T1DM of all ages (special mention should be made of the specific recommendation of the British NICE regarding the use of the Paradigm VEO system in patients with disabling hypoglycemia), deficient glucose control despite optimized and duly administered insulin therapy, and pregestational control and pregnancy in women with T1DM. The financing of RT-CGM systems in the various countries varies widely. The signs, however, are diverse, and the situation is fluid. According to the most recent evidence, financing by a majority of the public health systems of developed countries may become more common as the situation becomes clearer.
The integration of MCG and CSII into SAP systems forms the basis for developing automated (closed-loop) insulin infusion systems with minimal or no patient intervention that will eventually result in an artificial pancreas.
Cost-effectiveness of continuous glucose monitoringLittle evidence is available regarding the clinical efficacy and, especially, the efficiency of retrospective CGM. The evidence concerning the efficiency of RT-CGM, while also limited, is greater. The studies conducted include cost-utility and cost-effectiveness analyses using models that simulate diabetes progression and the development of secondary complications based on the clinical characteristics of the cohort, the associated risk factors (mainly metabolic control variables), and different predefined time horizons. The models most commonly used for this purpose are the CORE Diabetes Model and the Markov model.
The economic benefits to be derived from the prevention of hypoglycemia, which is potentially one of the main clinical benefits of CGM, was a primary objective in a recent economic study of the integrated system with suspension for hypoglycemia.
Economic evaluation of interactive continuous glucose monitoring (RT-CGM)Economic evaluation of RT-CGM has been addressed in several studies conducted in the United States. Huang et al. reported a cost-utility study comparing CGM and capillary glucose self-monitoring (CGSM) in T1DM on intensive therapy. The study included a cohort with HbA1c≥7% in adults aged >25 years and another cohort with HbA1c<7.0% including patients of all ages. Using a Markov model, the incremental cost-effectiveness ratio (ICER) per life year gained (QALY) was $ 98,679/QALY (€ 71,500/QALY, approx.) for the cohort with HbA1c>7%, and $ 78,943/QALY (€ 57,205/QALY) for the cohort with HbA1c<7%. Assuming a threshold of $ 100,000/QALY, accepted for other therapies in diabetes, CGM may be considered cost-effective.
McQueen et al. used a Markov model on a population cohort with adult T1DM and found a more favorable ICER of $ 45,033/QALY (€ 32,500/QALY approx.) for the use of CGM versus CGSM. The authors suggest that for patients with T1DM on intensive therapy and HbA1c>8%, CGM is a cost-effective alternative to CGSM.
Economic evaluation of SAP therapyRoze et al. conducted an economic evaluation analysis in T1DM on SAP therapy as compared to CSII and CGSM. Using the CORE Diabetes Model, and taking into consideration the improvement in metabolic control under SAP found in meta-analyses, the authors predicted a lower complication rate, with a mean delay of 1.15 years in the development of complications, and a longer life expectation (mean increase, 1.03 years). In the economic analysis, this resulted in an ICER of 367,571 Swedish krona/QALY (€ 39,000/QALY, approx.), favorable to the purchase of therapy in the Swedish system (500,000 SEK/€ 55,000). It was concluded, therefore, that SAP therapy was cost-effective as compared to CSII therapy alone.
Economic evaluation of SAP with a low-glucose suspend functionIn Australia, Ly et al. reported an economic evaluation analysis of low glucose suspend (LGS) systems in patients with T1DM. The economic evaluation was based on the result of the only clinical trial comparing SAP with LGS function to CSII alone in pediatric patients with T1DM and adults with evidence of unaware hypoglycemia. The primary objective of the analysis was ICER for severe hypoglycemia prevented, which was A$ 17,602 (€ 11,500, approx.) and A$14,289 (€ 9300, approx.) for the whole group and for the subgroup aged less than 12 years respectively. Based on these results, the authors concluded that SAP-LGS therapy is a cost-effective alternative to CSII therapy in patients with T1DM and unaware hypoglycemia, because the cost increase associated with this technology is partly compensated for by a reduction in the incidence of severe hypoglycemia and, consequently, of the use of resources to treat it.
In the British health care environment, and also using a CORE model, the use of SAP with LGS function has been proposed as a cost-effective option as compared to CSII.
In Spain, the Department of Health of the Canary Islands prepared, at the request of the Spanish Ministry of Health, a report evaluating RT-CGM systems. Based on the methodology and the specific scenarios analyzed, the report concluded that RT-CGM systems are not an adequate cost-effective alternative for glucose monitoring in patients with diabetes from the perspective of the Spanish national health system. This continued to be maintained following the analysis of subgroups of patients with T1DM and T2DM. However, these results contrast with those found in other contexts analyzed where this technology was found to be cost-effective (US, Sweden) and with data reported by the Agència d’Informació, Avaluació i Qualitat en Salut in Catalonia in 2010. Finally, with regard to the negative results of this recent study of the Agency for Healthcare Technologies, it should be noted that the cost-effective analysis was not conducted on the types of patients for which this therapy would probably be indicated. In any case, it is surprising that the results in the Spanish national health system are so negative, since most evaluations published (with similar characteristics and environment) report that RT-CGM systems are efficient.
Positioning of SED-SEEPWorking methodsThis document was prepared and approved by the Working Group on Technologies Applied to Diabetes (GTAD) of the Spanish Society of Diabetes (SED), and endorsed by the Spanish Society of Pediatric Endocrinology (SEEP) and the Group on Consensus and Clinical Guidelines and the SED itself before publication.
Members of the GTAD of SED are healthcare professionals involved in the technological management of diabetes and are representative of those involved in the treatment of patients with T1DM, and specifically in the application of the advanced technologies which are the object of this consensus, such as diabetes educators, nurses, and pediatric and adult endocrinologists.
In preparing this document, a comprehensive analysis was made of the currently available scientific evidence on continuous glucose monitoring in both children and adults. A systematic search was made in Medline of the available evidence published before 26 January 2017 using the term “continuous glucose monitoring”. The clinical guidelines on this subject issued by other scientific societies and the indications approved in the healthcare systems of countries similar to ours were also evaluated.
As stated in the document, the increasing evidence generated in this field will probably make this statement obsolete in the medium term. Finally, it should be noted that clinical indications for the flash system have not been included in this consensus document because it is not regarded as an RT-CGM system. It was also taken into consideration that adequate evidence as to the impact of this technology on clinical efficacy and safety is not yet available, and that its viability as an alternative to capillary glucose measurements and its efficiency also needs to be assessed.
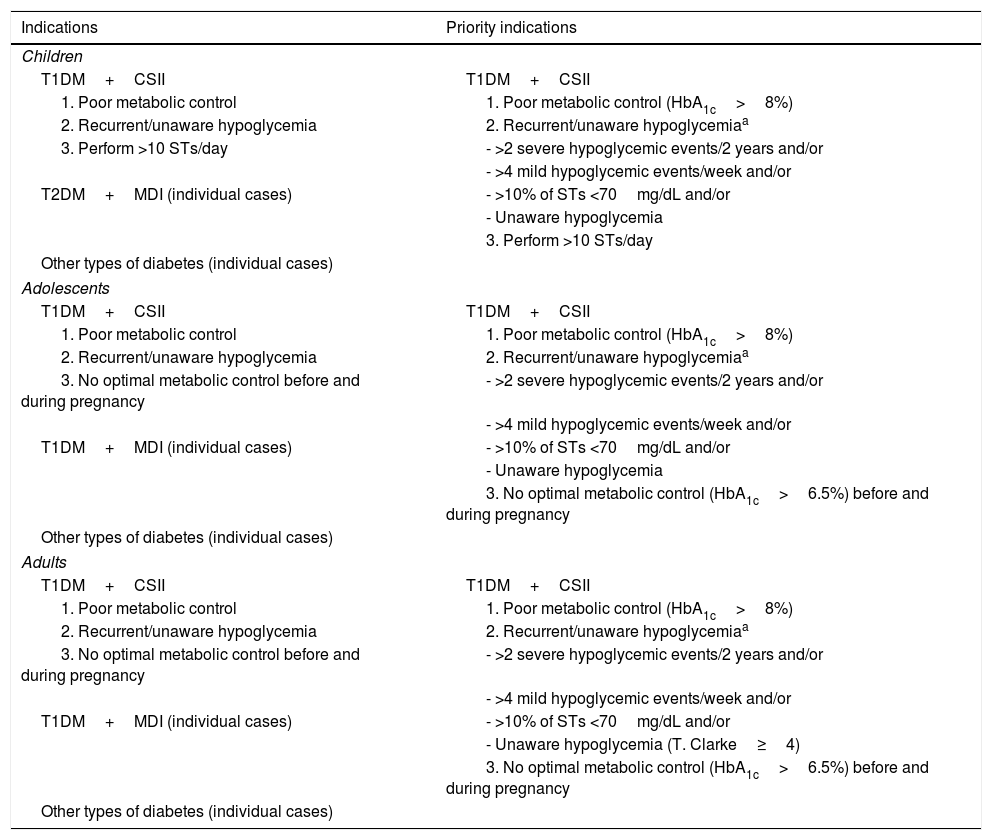
Based on the foregoing and after analyzing the current scientific evidence, the GTAD proposes indications for the clinical use of CGM. Table 1 describes the most widely accepted clinical indications for the use of RT-CGM and the priority clinical indications that, according to the GTAD, should first be assessed when considering the public reimbursement of these systems. Given that current resources are limited, we have described the conditions in which the system is most needed and the growing scientific evidence in support of its use.
Most widely accepted indications for RT-CGM systems in Spain.
| Indications | Priority indications |
|---|---|
| Children | |
| T1DM+CSII | T1DM+CSII |
| 1. Poor metabolic control | 1. Poor metabolic control (HbA1c>8%) |
| 2. Recurrent/unaware hypoglycemia | 2. Recurrent/unaware hypoglycemiaa |
| 3. Perform >10 STs/day | - >2 severe hypoglycemic events/2 years and/or |
| - >4 mild hypoglycemic events/week and/or | |
| T2DM+MDI (individual cases) | - >10% of STs <70mg/dL and/or |
| - Unaware hypoglycemia | |
| 3. Perform >10 STs/day | |
| Other types of diabetes (individual cases) | |
| Adolescents | |
| T1DM+CSII | T1DM+CSII |
| 1. Poor metabolic control | 1. Poor metabolic control (HbA1c>8%) |
| 2. Recurrent/unaware hypoglycemia | 2. Recurrent/unaware hypoglycemiaa |
| 3. No optimal metabolic control before and during pregnancy | - >2 severe hypoglycemic events/2 years and/or |
| - >4 mild hypoglycemic events/week and/or | |
| T1DM+MDI (individual cases) | - >10% of STs <70mg/dL and/or |
| - Unaware hypoglycemia | |
| 3. No optimal metabolic control (HbA1c>6.5%) before and during pregnancy | |
| Other types of diabetes (individual cases) | |
| Adults | |
| T1DM+CSII | T1DM+CSII |
| 1. Poor metabolic control | 1. Poor metabolic control (HbA1c>8%) |
| 2. Recurrent/unaware hypoglycemia | 2. Recurrent/unaware hypoglycemiaa |
| 3. No optimal metabolic control before and during pregnancy | - >2 severe hypoglycemic events/2 years and/or |
| - >4 mild hypoglycemic events/week and/or | |
| T1DM+MDI (individual cases) | - >10% of STs <70mg/dL and/or |
| - Unaware hypoglycemia (T. Clarke≥4) | |
| 3. No optimal metabolic control (HbA1c>6.5%) before and during pregnancy | |
| Other types of diabetes (individual cases) | |
ST: capillary glucose self-testing; T1DM: type 1 diabetes mellitus; CSII: continuous subcutaneous insulin infusion (pump systems).
The combination of CSII and RT-CGM (SAP therapy) together with the low glucose suspend/predictive low-glucose suspend functions has been shown to decrease the proportion of values <70mg/dL in CGM. The GTAD recommends that priority consideration should be given to these devices in cases where RT-CGM is indicated due to recurrent/unaware hypoglycemia. However, there is no strong evidence comparing this function to the SAP system without this facility.
Adherence to the established recommendations (discussed in the main document) and the achievement of individual goals, including the degree of patient satisfaction, should be reassessed at six months of treatment start and at the regular intervals deemed appropriate by the medical team (annually).
The GTAD and, on its behalf, the signatories of this document, have received at some time funding from the main companies working in diabetes-related technology (Medtronic, Roche, DEXCOM, Abbott, etc.).
Eva Aguilera Hurtado, Francisco Javier Ampudia-Blasco, Víctor Manuel Andía Melero, Ramiro Antuña de Alaiz, Raquel Barrio Castellanos, Pilar Isabel Beato Víbora, Águeda Caballero Figueroa, Ana Isabel Chico Ballesteros, Gonzalo Díaz Soto, Marta Elena Domínguez López, Mercedes Galindo Rubio, Beatriz García Cuartero, José Manuel García López, Marga Giménez Álvarez, Cintia González Blanco, María José Goñi Iriarte, Gracia María Lou Francés, Pilar Martín Vaquero, María Asunción Martínez Brocca, Juan Fco. Merino Torres, Jesús Moreno Fernández, María José Picón César, Mercedes Rigla Cros, María Soledad Ruiz de Adana Navas, María Yolanda Salgado Frutos, Higinio Salgado Pacheco, Inmaculada Simón Muela, Estíbaliz Ugarte Abasolo, Maite Valverde Torreguitart, Federico Vázquez San Miguel, Mercè Vidal Flor, Carmen Yoldi Vergara.
SED-SEED Positioning Document on CGM in Spain. February 2017. Available at: http://www.sediabetes.org/modulgex/workspace/publico/modulos/web/docs/apartados/388/210217_033809_2296268171.pdf
Annex 1. Available at: http://www.sediabetes.org/modulgex/workspace/publico/modulos/web/docs/apartados/388/210217_033809_5618861048.pdf
Annex 2. Available at: http://www.sediabetes.org/modulgex/workspace/publico/modulos/web/docs/apartados/388/210217_033809_8081258813.pdf
Please cite this article as: Giménez M, Díaz-Soto G, Andía V, Ruíz de Adana MS, García-Cuartero B, Rigla M, et al. Documento de consenso SED-SEEP sobre el uso de la monitorización continua de la glucosa en España. Endocrinol Diabetes Nutr. 2018;65:24–28.
The members of the Group on Technologies Applied to Diabetes of the SED and of the SEEP are listed in Appendix A.