Elevated plasma lactate dehydrogenase (LDH) levels can be found in a great variety of conditions, including systemic infections or inflammation, muscle injury, hemolysis, thromboembolism, or malignancy. An uncommon and benign cause of such elevation is the presence of immune complexes called macroenzymes. A firm diagnosis of the underlying cause is therefore essential. However, the diagnosis is not always obvious, and other manifestations of the disorder need to be considered.
We report the case of a 50-year-old woman with no prior history of interest and diagnosed with primary hyperthyroidism (undetectable TSH, FT3 15.41pg/mL [normal range 2.5–3.9], FT4 39.9pg/mL [5.8–16.4]), for which antithyroid treatment was started (methimazole 20mg/day). The results of the complementary tests were consistent with Graves–Basedow disease (anti-TSH receptor antibodies [TRab] 23mIU/mL [0–1.5]; a significant increase in vascularization in both thyroid lobes as revealed by ultrasound). During follow-up (16 weeks after starting methimazole), the patient developed multiple joint pain in the hips and ankles, with LDH 1175μ/L (240–480), the remaining biochemical parameters and blood count values being within normal ranges. Her general condition was excellent, and the physical examination yielded no data of interest.
Since treatment with antithyroid drugs may trigger arthralgia and osteoarthritis,1 the patient was evaluated by Rheumatology, which ruled out disease. The subsequent biochemical controls showed persistent LDH elevation (>1000μ/L). The patient reported newly manifesting constipation. Colonoscopy and abdominal ultrasound were thus performed, with normal findings. Evaluation by Gynecology ruled out the presence of a gynecological neoplastic process. Likewise, since several nevi were found, dermatology discarded the presence of melanoma. A peripheral blood smear proved to be normal. Based on all the previous complementary tests, with no pathological findings, and in the presence of sustained high LDH levels, a positron emission tomography (PET) scan was performed and possible neoplastic disease discarded.
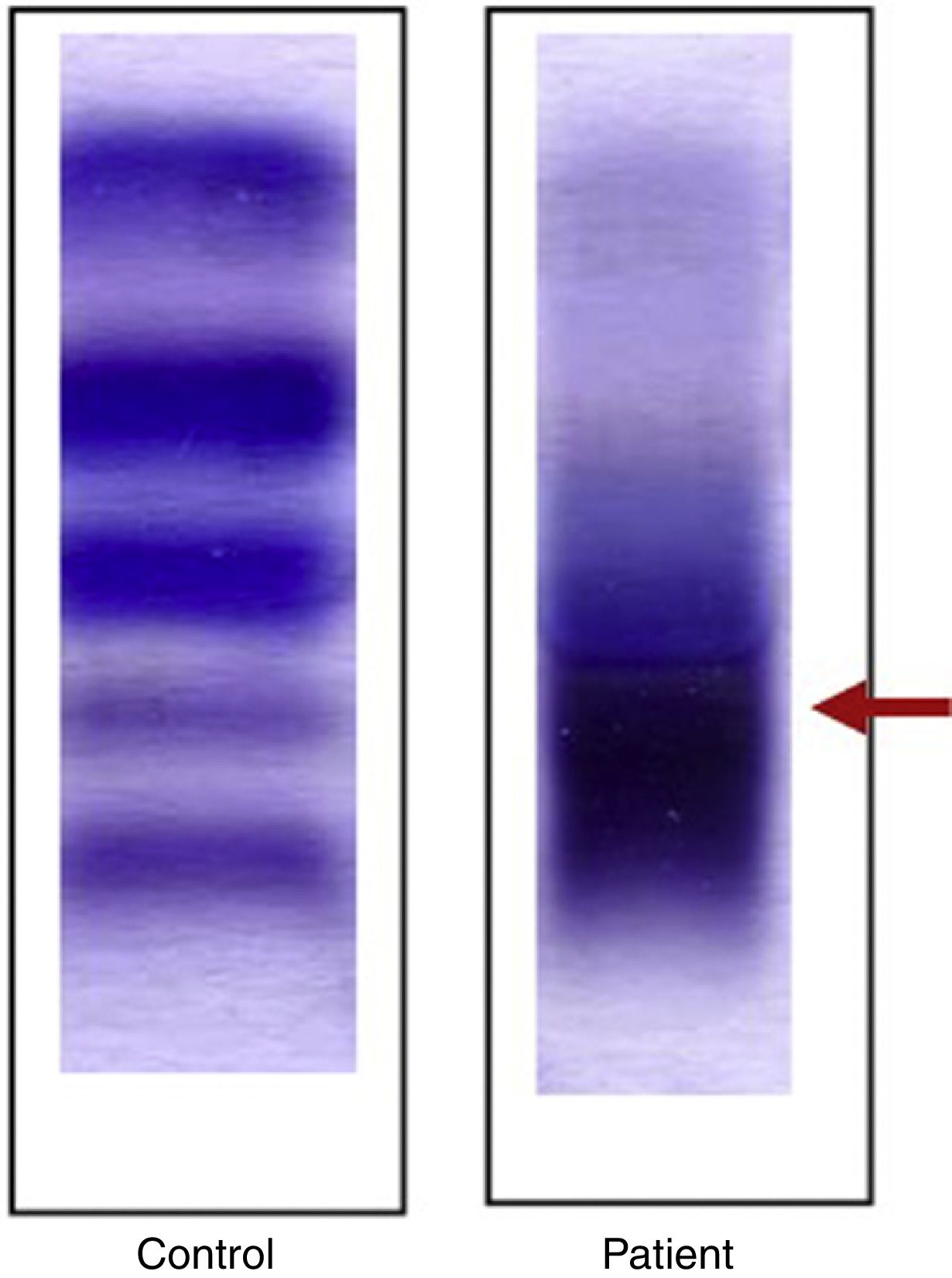
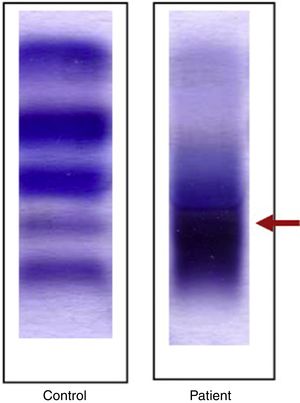
In the absence of a diagnosis, electrophoresis (Reference laboratory) was requested to assess the different LDH isoforms. The results showed the presence of high molecular weight isoforms suggesting circulating immune complexes bound to immunoglobulins (macro-LDH, Fig. 1).
One and a half years after the diagnosis, and 6 months after the discontinuation of antithyroid treatment, the Graves–Basedow disease is in remission (TSH 1.22μIU/mL, FT4 9.75pg/mL, TRab 0.9mIU/mL), with persistent markedly elevated LDH levels (>800μ/L).
Macroenzymes are complexes resulting from the binding of serum enzymes to a plasma protein such as circulating immunoglobulins (Igs), the most common being IgG. The macroenzymes most commonly reported in the literature are macro-creatine kinase (CK)2 and macro-amylase,3 with a reported macro-CK prevalence of 2% in hospitalized patients when systematic screening is performed.4 The diagnosis of macro-LDH is established by electrophoresis,5 which shows the presence of an abnormal high molecular weight band, with a half-life that increases as a result of decreased elimination through the kidneys. No association between autoimmune thyroid disease and macro-LDH has been established to date. However, some studies have suggested a possible relationship between these enzyme complexes and other autoimmune diseases such as rheumatoid arthritis or lupus erythematosus.6,7 The physiopathology of macroenzyme formation has not been established. It has been suggested that the release of LDH into plasma and its exposure to proteolytic activity may lead to conformational change in the enzyme, increasing its immunogenicity.8,9
On the other hand, the existence of these complexes has future repercussions for the patient, since enzyme determination cannot be used for diagnostic or for follow-up purposes, i.e., its clinical usefulness is lost.
Our review of the literature has yielded only one previous case of macro-LDH associated with Graves–Basedow disease.10 A lack of awareness of this relationship and the scant link between the two disorders caused us to perform multiple complementary tests. Greater initial diagnostic suspicion could have reduced the patient risks associated with invasive tests, as well as the uncertainty related to the lack of a definitive diagnosis.
Given the limited understanding of this disorder in the medical community,5 we believe that our clinical experience may encourage other specialists to include screening for macroproteins in patients with high enzyme or protein levels, in which no firm diagnosis is apparent and few clinical repercussions are observed. This could contribute to limiting the number of complementary tests performed and to optimizing the time to diagnosis.
In any case, further studies are needed to establish the mechanism whereby these complexes are formed and the risk factors involved, as well as their natural history.
Please cite this article as: Jiménez Varas I, Miren Azkutia A, Cuesta M. Elevación persistente de lactato deshidrogenasa de causa desconocida en enfermedad de Graves. Endocrinol Diabetes Nutr. 2018;65:374–375.