Hypoparathyroidism (HP) is the most common complication of total thyroidectomy and can be an emergency.
ObjectivesTo describe the prevalence of HP after total thyroidectomy in children under 14 years of age, the variables related to its appearance and its clinical expression.
Patients and methodsRetrospective study at a children's hospital in the last 20 years. HP was defined by the need to supplement calcium after the intervention and was considered permanent if it could not be suspended within 12 months. Fisher’s statistical method of comparison of proportions.
ResultsThirty-nine children and adolescents (26 females) with an age range of 3.67–14.00 years. In 25 patients, the intervention was prophylactic and in 14 it was therapeutic; 14 suffered accidental excision of some parathyroid gland, but none more than two of them; 12 presented HP, of which 3 were permanent; 5 presented clinical symptoms; 1 of them was an emergency. The frequency of HP was 4/4 when 2 parathyroids were dissected, 2/10 when one was dissected, and 6/25 when none were dissected (p = 0.02). In the prophylactic interventions, it was 6/25 compared to 6/14 in the therapeutic ones (p = 0.29). The three cases of permanent HP were in children under 6 years of age, and it did not occur in any older children (p = 0.09).
ConclusionsHP is a common and sometimes serious complication in children after total thyroidectomy. It can occur, and even be permanent, even if the intervention is prophylactic and parathyroid glands remain in situ. Younger age could be a risk factor.
El hipoparatiroidismo (HP) es la complicación más frecuente de la tiroidectomía total y puede suponer una emergencia.
ObjetivosDescribir la prevalencia de HP tras tiroidectomía total en menores de 14 años, las variables relacionadas con su aparición y su expresión clínica.
Pacientes y métodosEstudio retrospectivo en un hospital infantil en los últimos 20 años. El HP se definió por la necesidad de suplementar calcio tras la intervención y se consideró permanente si no pudo suspenderse en 12 meses. Método estadístico de Fisher de comparación de proporciones.
ResultadosTreinta y nueve niños y adolescentes (26 mujeres) de un rango de edad de 3,67 a 14,00 años. En 25 pacientes la intervención fue profiláctica y en 14 terapéutica. Catorce sufrieron exéresis accidental de alguna glándula paratiroides, pero ninguno de más de dos de ellas. Doce presentaron HP, de los cuales 3 fueron permanentes, 5 presentaron sintomatología clínica y 1 de ellos supuso una emergencia. La frecuencia de HP fue de 4/4 cuando se disecaron 2 paratiroides, 2/10 cuando una y 6/25 cuando ninguna (p = 0,02). En la intervención profiláctica fue de 6/25 frente a 6/14 en la terapéutica (p = 0,29). Los tres casos de HP permanente fueron niños menores de 6 años, no ocurriendo el permanente en ningún niño mayor (p = 0,09).
ConclusionesEl HP es una complicación frecuente y en ocasiones grave en el niño tras la tiroidectomía total. Puede ocurrir, e incluso ser permanente, aunque la intervención sea profiláctica y queden glándulas paratiroides in situ. La menor edad podría ser un factor de riesgo.
Parathyroid hormone or parathormone (PTH) is one of the main regulators of plasma calcium levels. Its deficit, hypoparathyroidism (HP), can produce, among other acute and chronic manifestations, hypocalcaemia whose expression will be proportional to its severity and speed of onset. The manifestation of decreased plasma calcium is tetany, characterised by neuromuscular irritability, which produces mild symptoms (paresthaesias in the perioral region, hands and feet, muscle cramps), severe symptoms (carpopedal spasms, focal and generalised crises) or life-threatening emergencies (laryngospasm, arrhythmias and refractory heart failure).1
HP is the most common complication of total and near-total thyroidectomy in both adults and children. It is produced by the inadvertent removal of the parathyroid glands during surgery and, furthermore, since the parathyroid tissue requires very good irrigation, ischaemia and mechanical, thermal or electrical damage during surgical procedures can leave these glands totally non-functional even if they remain in situ. Most of the time, PH is temporary, with spontaneous recovery of parathyroid function in a few weeks or months, but sometimes it is permanent, either because all the glands have been sectioned, or because they have lost all their functionality despite retaining their position.1,2
The objectives of our study were to describe the prevalence of HP (whether temporary or permanent) in children under 14 years of age who underwent total thyroidectomy, the variables related to its appearance, and its clinical expression.
Patients and methodsThis is a retrospective study of children who underwent total thyroidectomy in a children's hospital in the last 20 years. The interventions were performed by the same surgical team, which has been performing two or three a year. The variables of sex, age at the time of the surgery, diagnosis that indicated the thyroidectomy, number of parathyroid glands that appeared in the surgical specimen sent to anatomical pathology, whether the thyroidectomy was performed in one or two interventions (first one hemithyroidectomy and then the other), whether or not the lymph nodes in the neck were dissected, whether HP appeared, the time at which treatment with calcium was started and when it was discontinued, and the symptoms and signs attributed to HP were collected from the medical histories. Autotransplantation of parathyroid glands was not performed in any case.
According to the indication for thyroidectomy, two groups of patients were defined: therapeutic thyroidectomy, if they had thyroid disease, and prophylactic, if they did not have thyroid disease but were carriers of precursor genetic alterations of medullary thyroid carcinoma after a family genetic study.
HP was defined by the need to take calcium supplements and/or active metabolites of Vitamin D (hormone D) after the surgery and a distinction was made between temporary and permanent if those were able to be discontinued within 12 months or not. Diagnosis was reached in two ways, depending on whether or not an urgent biochemical determination of PTH was available. Currently, this hormone is determined 10 min after completing the thyroidectomy, a level below 15 pg/mL is diagnostic of HP, and treatment with calcium and hormone D supplements are started immediately to prevent hypocalcaemia, according to current international recommendations.2 Previously, when this analysis was not available, HP was diagnosed by the appearance of clinical or biochemical hypocalcaemia in the first five days postoperatively, with calcium levels being monitored every eight hours and symptoms closely watched for.
Quantitative variables are expressed with their mean, standard deviation and range, and qualitative variables with their proportion and percentage. Proportions were compared using Fisher's exact statistical method using the SPSS®programme.
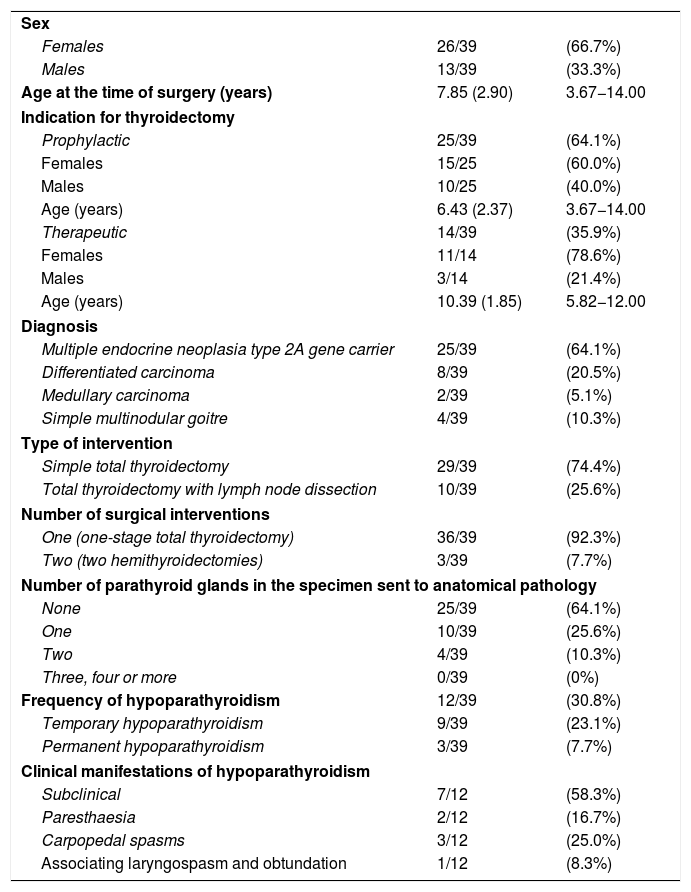
ResultsIn the last 20 years, 39 children and adolescents with an age range of 3.67–14.00 years have undergone total thyroidectomy at our centre. In 25 patients, the intervention was prophylactic, since they were healthy carriers of genetic mutations that predispose to multiple endocrine neoplasia type 2A. In the 10 cases with malignant disease, lymph node dissection was also performed. In three of these, two interventions were performed: first a hemithyroidectomy, whose histological analysis diagnosed differentiated carcinoma, and in a second surgical procedure, a total thyroidectomy and lymph node dissection of the central neck compartment were completed. Fourteen anatomical pathology specimens showed accidentally sectioned parathyroid glands, but in no case were more glands found. Twelve of those who underwent surgery presented HP, in three of them it was permanent and in nine, temporary. Table 1 shows the variables collected in our patients in more detail.
Variables of our patients.
| Sex | ||
| Females | 26/39 | (66.7%) |
| Males | 13/39 | (33.3%) |
| Age at the time of surgery (years) | 7.85 (2.90) | 3.67−14.00 |
| Indication for thyroidectomy | ||
| Prophylactic | 25/39 | (64.1%) |
| Females | 15/25 | (60.0%) |
| Males | 10/25 | (40.0%) |
| Age (years) | 6.43 (2.37) | 3.67−14.00 |
| Therapeutic | 14/39 | (35.9%) |
| Females | 11/14 | (78.6%) |
| Males | 3/14 | (21.4%) |
| Age (years) | 10.39 (1.85) | 5.82−12.00 |
| Diagnosis | ||
| Multiple endocrine neoplasia type 2A gene carrier | 25/39 | (64.1%) |
| Differentiated carcinoma | 8/39 | (20.5%) |
| Medullary carcinoma | 2/39 | (5.1%) |
| Simple multinodular goitre | 4/39 | (10.3%) |
| Type of intervention | ||
| Simple total thyroidectomy | 29/39 | (74.4%) |
| Total thyroidectomy with lymph node dissection | 10/39 | (25.6%) |
| Number of surgical interventions | ||
| One (one-stage total thyroidectomy) | 36/39 | (92.3%) |
| Two (two hemithyroidectomies) | 3/39 | (7.7%) |
| Number of parathyroid glands in the specimen sent to anatomical pathology | ||
| None | 25/39 | (64.1%) |
| One | 10/39 | (25.6%) |
| Two | 4/39 | (10.3%) |
| Three, four or more | 0/39 | (0%) |
| Frequency of hypoparathyroidism | 12/39 | (30.8%) |
| Temporary hypoparathyroidism | 9/39 | (23.1%) |
| Permanent hypoparathyroidism | 3/39 | (7.7%) |
| Clinical manifestations of hypoparathyroidism | ||
| Subclinical | 7/12 | (58.3%) |
| Paresthaesia | 2/12 | (16.7%) |
| Carpopedal spasms | 3/12 | (25.0%) |
| Associating laryngospasm and obtundation | 1/12 | (8.3%) |
Quantitative variables are expressed with their mean, (standard deviation) and range, and qualitative variables with their proportion and percentage.
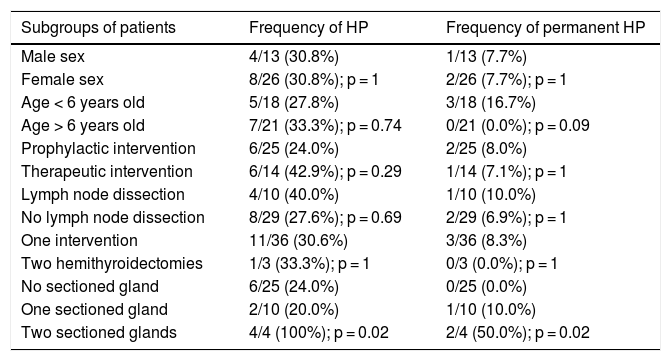
HP was significantly more common in cases in which two parathyroid glands were accidentally dissected. However, having glands remaining in situ does not guarantee that they are functional, since none of our children with permanent HP had lost all of their parathyroid tissue. Both those patients who underwent prophylactic surgery and those patients who underwent therapeutic surgery were affected by HP, even if the thyroidectomy was performed in a single surgical procedure and even if lymph node dissection was not performed. The prevalence of permanent HP was higher in the group under six years of age, although this difference did not reach statistical significance. The three cases of permanent HP occurred in the youngest girl operated on for carcinoma, at five years old, and in the only two relatives with multiple endocrine neoplasia who underwent surgery before the age of four. Table 2 shows the frequencies of HP in the different subgroups of patients.
Frequency of hypoparathyroidism in different subgroups of patients.
| Subgroups of patients | Frequency of HP | Frequency of permanent HP |
|---|---|---|
| Male sex | 4/13 (30.8%) | 1/13 (7.7%) |
| Female sex | 8/26 (30.8%); p = 1 | 2/26 (7.7%); p = 1 |
| Age < 6 years old | 5/18 (27.8%) | 3/18 (16.7%) |
| Age > 6 years old | 7/21 (33.3%); p = 0.74 | 0/21 (0.0%); p = 0.09 |
| Prophylactic intervention | 6/25 (24.0%) | 2/25 (8.0%) |
| Therapeutic intervention | 6/14 (42.9%); p = 0.29 | 1/14 (7.1%); p = 1 |
| Lymph node dissection | 4/10 (40.0%) | 1/10 (10.0%) |
| No lymph node dissection | 8/29 (27.6%); p = 0.69 | 2/29 (6.9%); p = 1 |
| One intervention | 11/36 (30.6%) | 3/36 (8.3%) |
| Two hemithyroidectomies | 1/3 (33.3%); p = 1 | 0/3 (0.0%); p = 1 |
| No sectioned gland | 6/25 (24.0%) | 0/25 (0.0%) |
| One sectioned gland | 2/10 (20.0%) | 1/10 (10.0%) |
| Two sectioned glands | 4/4 (100%); p = 0.02 | 2/4 (50.0%); p = 0.02 |
HP: hypoparathyroidism.
The proportions were compared using Fisher's exact method.
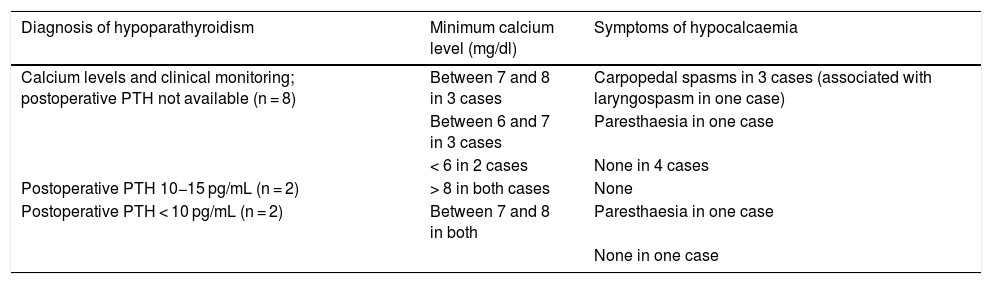
HP was diagnosed by post-operative PTH levels less than 15 pg/mL in four cases, of the eight for which this determination was available. Despite the early treatment established in the first six hours postoperatively, one of them presented with hypocalcaemia of 7.3 mg/dl with mild symptoms (isolated and self-limited paresthaesias) at 24 h’ evolution.
Table 3 shows a summary of the clinical and biochemical characteristics of HP according to its form of diagnosis. The range of HP duration in temporary cases was 9–81 days (median 40 days). In total, HP was symptomatic in five children. Four of the patients manifested it between 24 and 48 h postoperatively, being hospitalised. The fifth patient was discharged from hospital 48 h after surgery, asymptomatic and with normal and stable calcium levels, but attending the emergency department 96 h after surgery, with spasms.
Hypoparathyroidism: form of diagnosis and clinical manifestations.
| Diagnosis of hypoparathyroidism | Minimum calcium level (mg/dl) | Symptoms of hypocalcaemia |
|---|---|---|
| Calcium levels and clinical monitoring; postoperative PTH not available (n = 8) | Between 7 and 8 in 3 cases | Carpopedal spasms in 3 cases (associated with laryngospasm in one case) |
| Between 6 and 7 in 3 cases | Paresthaesia in one case | |
| < 6 in 2 cases | None in 4 cases | |
| Postoperative PTH 10−15 pg/mL (n = 2) | > 8 in both cases | None |
| Postoperative PTH < 10 pg/mL (n = 2) | Between 7 and 8 in both | Paresthaesia in one case |
| None in one case |
PTH: parathyroid hormone.
The patient who had a serious evolution was a child under four years of age who, after suffering post-surgical hypocalcaemia, had treatment withdrawn until it was suspended, attempting to use the hypocalcaemia as a stimulus to hypertrophy the parathyroid tissue that had remained in situ, as in the anatomical pathology specimen only two glands were identified. Months after discontinuation of treatment, since he had developed a clinical tolerance to low calcium levels, he suddenly suffered generalised tetany, laryngospasm and decreased level of consciousness, with a calcium level of 4.9 mg/dl, which was a life-threatening emergency. Iatrogenic morbidity derived from the administration of intravenous calcium salts was added to the morbidity of the condition, as he suffered from a very painful calcium phlebitis of the entire venous tree through which they were provided, and later calcinosis cutis when the calcium crystals emerged through the skin.
DiscussionOur work highlights the importance (both due to its frequency and its potential severity) of post-thyroidectomy HP in paediatric patients and presents its peculiarities in children and adolescents, since most of the published literature on this subject is from adult patients.
Post-surgical HP is quite common. Its prevalence is highly variable according to the authors. In adults it occurs in between 20 and 60% of interventions, while it is permanent between 0 and 12% of the time.2,3 The main factor that determines this wide variability is the experience of the surgical team: the higher the volume of interventions, the lower the number of any of its complications. Regarding some examples, we can see how an Italian centre logging 933 interventions publishes quite low rates, of 20% and 2% of temporary and permanent HP, respectively4, while in multicentre studies with a lower volume of patients per centre, such as the Spanish national registry of 1,792 patients operated on in 20 hospitals, it rises to 48.3% for temporary HP and 14.5% for permanent.5
Published paediatric series also confirm these differences. When it comes to a single centre with a high volume, the prevalences range between 12 and 37% of temporary HP and between 0.6 and 4% of permanent,6–10 while in multicentre studies they amount to between 23 and 49% temporary and between 7 and 21% permanent,11–15 figures that are comparable to those of our centre, where the volume of thyroidectomies in the paediatric age is low.
In addition to the experience of the surgeon, other classically described risk factors for damage to the parathyroid tissue during surgery are the extent of the thyroidectomy (whether it is bilateral), lymph node dissection of the central neck compartment (which is why HP is more common in malignant thyroid disease), enlarged thyroid or thyroid with substernal extension, Graves' disease and re-intervention. On the contrary, in a prophylactic thyroidectomy of a healthy thyroid, the risk decreases.2,5–7,11,12,15,16 The series of paediatric patients, although providing less evidence, also corroborate these same factors reported in adults, along with an additional one, age under five years, since it is more difficult to identify the parathyroid glands in these very young children.6,16 We have verified this fact, but we have not achieved statistical significance as we have a very limited sample.
Since clinical practice guidelines17 recommend thyroidectomy in most relatives with multiple endocrine neoplasia before the age of five years, we cannot delay the age of surgery in these children to reduce the risk of HP. The challenge is to minimise the damage to the parathyroid tissue at these difficult ages, and for this there are two lines of research. The first tries to improve the visualisation of the parathyroid glands to preserve their irrigation and the second proposes the autotransplantation of those that suffer from ischaemia or accidental section.2 Visualisation could be improved by incorporating intraoperative ultrasound18 and optical techniques, such as autofluorescence, indocyanine green, methylene blue fluorescence, or 5-aminolevulinic acid,19 all of which are currently underutilised.
Regarding autotransplantation, at the moment there is no consensus on its performance, and according to a recently published systematic review of the literature, its benefits have not yet been demonstrated.20 A Chinese group proposes to classify the parathyroid glands into groups at risk of being damaged according to their relationship with the thyroid gland and the thymus and decide whether to keep them in situ (those with low risk of damage) or autotransplant them (those with high risk). With this decision they manage to significantly lower the incidence of permanent HP from 4.5 to 0.4%.21
The urgent determination of PTH after surgery has been agreed upon at the national and international level22,2 as the fastest way to predict HP and to prevent hypocalcaemia by starting treatment early, in the first few hours postoperatively. As this hormone has a very short half-life (three to five minutes), its determination is valid 10 min after thyroidectomy, while it is generally necessary to wait 12–24 h for calcium levels to drop. In our patients, although there are still too few cases to be able to analyse them (eight cases), it appears to us that the use of postoperative PTH is reducing the frequency of clinical and biochemical hypocalcaemia, especially in severe forms. The inconvenience, undoubtedly minor, would be an increase in the frequency of HP (4/8 cases) when using the threshold of 15 pg/mL of PTH proposed by the consensus.2 With such a conservative figure, we could be overdiagnosing and overtreating, although this is undoubtedly better than exposing children to the risk of severe hypocalcaemia.
ConclusionsWe can conclude that HP is a common and sometimes serious complication in children and adolescents undergoing total thyroidectomy. It can occur, and even be permanent, even if the surgery is prophylactic, parathyroid glands remain in situ and none of the classically described risk factors are present. Younger age could be another independent risk factor.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-García E, Gómez-Gila AL, Romero-Lluch AR, Conde-Sánchez M, Domínguez-Pascual I, Fernández Pineda I, et al. Hipoparatiroidismo postiroidectomía: experiencia de 20 años en un hospital infantil. Endocrinol Diabetes Nutr. 2022;69:92–97.