Hypoglycemia associated to insulin or other glucose-lowering agents is one of the most common causes of visits to the emergency department for adverse drug reactions. The study objective was to analyze the characteristics of patients with diabetes mellitus (DM) who attend a tertiary hospital emergency department for a hypoglycemic event.
Patients and methodsA 3-year retrospective analysis was conducted of patients with DM who attended the emergency department of Hospital Universitari de Bellvitge for a hypoglycemic event. An analysis was made of epidemiological and diabetes-related characteristics, prevalence of chronic diabetic complications and other comorbidities, the glucose-lowering treatment and the result of the hypoglycemic episode.
ResultsOf the 149 hypoglycemic events analyzed, 81.9% occurred in patients with type 2 DM. Mean age of patients with type 2 DM was 75.4 years. DM duration was longer than 10 years in 69.4% of patients. The prevalence rates of chronic kidney disease and cognitive decline were 38.5% and 19.7% respectively in patients with type 2 DM. Insulin with or without other concomitant glucose-lowering agents was associated to 78.7% of episodes in type 2 DM patients. The remaining 21.3% were associated to oral hypoglycemic agents, mainly glibenclamide. After the event, 13.4% of patients required hospital admission, and in 36.8% of these hypoglycemia was associated to use of glibenclamide.
ConclusionsA majority of hypoglycemic events occurred in elderly patients with type 2 DM, with a high prevalence of associated comorbidities and treated with insulin and sulfonylureas, particularly glibenclamide.
La hipoglucemia asociada a insulina u otros hipoglucemiantes es una de las principales causas de consulta a urgencias por efectos secundarios de medicamentos. El objetivo del estudio es analizar las características de los pacientes con diabetes mellitus (DM) que consultan a urgencias hospitalarias por un episodio de hipoglucemia.
Pacientes y métodosSe realizó un análisis retrospectivo de los pacientes con DM que fueron atendidos en el Servicio de Urgencias del Hospital Universitari de Bellvitge con el diagnóstico de hipoglucemia durante un periodo de 3 años. Se analizaron las características epidemiológicas, las relacionadas con la DM, sus complicaciones y otras comorbilidades, el tratamiento hipoglucemiante de base y el resultado del episodio de hipoglucemia.
ResultadosSe analizaron 149 episodios de hipoglucemia. El 81,9% de los casos eran pacientes con DM tipo 2. La edad media de los pacientes con DM tipo 2 fue de 75,4 años. La duración de la DM era superior a los 10 años en el 69,4% de los casos. La prevalencia de insuficiencia renal crónica y deterioro cognitivo fue del 38,5 y del 19,7%, respectivamente, en los pacientes con DM tipo 2. El 78,7% de los pacientes con DM tipo 2 estaban tratados con insulina con o sin otros hipoglucemiantes asociados. El 21,3% restante se trataban con agentes orales, principalmente glibenclamida. El 13,4% de los casos requirieron ingreso hospitalario y, en el 36,8% de ellos, la hipoglucemia estaba asociada al uso de glibenclamida.
ConclusionesLa mayoría de episodios de hipoglucemia se produjeron en pacientes con DM tipo 2 de edad avanzada, con elevada prevalencia de enfermedades asociadas y en tratamiento con insulina y sulfonilureas, especialmente glibenclamida.
Diabetes mellitus (DM) affects 14% of the population in Spain,1 and the main limitation of drug treatment for the disease is the risk of hypoglycemia, defined as a blood glucose concentration of <70mg/dl.2 Some studies have shown hypoglycemia associated with drug treatment of DM to be one of the leading causes of emergency room visits and of hospital admissions due to the side effects of drugs.3 The medications associated with hypoglycemia include insulin and classical insulin secretagogues (sulfonylureas and meglitinides). Hypoglycemia causes symptoms due to the activation of the autonomic nervous system (tremor, palpitations, diaphoresis) and manifestations derived from glucose deficiency in the central nervous system (confusion, behavioral changes, diminished consciousness, coma). Severe hypoglycemia is defined as an episode of hypoglycemia in which the patient needs assistance for its treatment.
The immediate and subsequent consequences of hypoglycemia are multiple: it affects patient quality of life, work activity and common daily activities such as driving, and in severe cases can lead to additional morbidity–mortality with neurological symptoms. Hypoglycemia may cause patients to reduce their adherence to treatment with the purpose of reducing the risk of such episodes, with the consequent worsening of metabolic control.4 Various studies have shown an association between severe hypoglycemia and cardiovascular disease.5 There are several mechanisms by which hypoglycemia may promote adverse cardiovascular events. Hypoglycemia can exert a proarrhythmic effect due to ST-segment and T-wave modifications, QT prolongation or ectopic beats.6 Activation of the sympathetic nervous system by hypoglycemia causes an increase in heart rate and myocardial contractility, and changes in vascular elasticity that can lead to cardiac overload, particularly in patients with previous cardiovascular disease. Catecholamines and other peptides released during hypoglycemia cause platelet activation and aggregation and endothelial dysfunction that in turn may favor atherosclerosis.7 Hypoglycemic episodes also result in increased direct and indirect economic costs associated with DM, especially if hospital admission proves necessary.8
Few studies in our setting have evaluated the characteristics of patients with hypoglycemia leading to emergency room visits, and none have been carried out in recent years.9 This is particularly relevant in the current scenario, characterized by the appearance of new drug classes and insulin analogs offering an improved safety profile in terms of hypoglycemia risk.
The objective of the present study was to analyze the characteristics, treatment and course of patients with DM seen due to hypoglycemia in the Emergency Department of our hospital.
Patients and methodsA retrospective observational study was conducted at Hospital Universitari de Bellvitge (Barcelona, Spain). We included patients seen in the emergency room of our center during 2012–2014 with a diagnosis of hypoglycemia. Patients not diagnosed with DM were excluded, as well as cases in which a capillary or plasma glucose level of <70mg/dl was not confirmed.
We analyzed patient age, the type of DM, the time from the onset of the disease, the degree of glycemic control, the presence of vascular and renal complications, as well as other relevant comorbidities (including cognitive impairment and alcohol abuse), recent hospitalization episodes, background glucose-lowering therapy, the treatment used to resolve the episode, and the care outcome. The data referring to each episode were compiled from the electronic emergency care reports. Information regarding the disease history was obtained from the electronic primary care history (Estació Clínica d’Atenció Primària [ECAP]). The degree of glycemic control was assessed based on the glycosylated hemoglobin (HbA1c) concentration in those cases where a measurement of this parameter in the previous three months was available. The time from the onset of DM was stratified by intervals (less than or more than 10 years), because in those patients diagnosed with DM before the introduction of the electronic case history system, the stated date of diagnosis of DM was the date on which the diagnosis was recorded in the electronic case history. Renal failure was defined as an estimated glomerular filtration rate (eGFR) of <60ml/min/1.73m2 in more than one measurement over at least three months.
The study was conducted in accordance with the recommendations of the Declaration of Helsinki (Fortaleza, 2013). As this was a retrospective analysis, patient informed consent was not considered necessary. The patient data were anonymized according to the provisions of the Organic Act 15/1999 on Personal Data Protection. The present article was reviewed for publication by the Clinical Research Ethics Committee of Hospital Universitari de Bellvitge.
Quantitative variables were reported as the mean and standard deviation (SD), while qualitative variables were reported as number and percentage. The comparative analysis of quantitative variables was performed using parametric tests (Student t-test) or nonparametric tests (Mann–Whitney U-test) in the absence of a normal data distribution. Qualitative variables were compared using the chi-squared test or nonparametric tests (Fisher's exact test) when the percentage of cells with an expected frequency of less than 5 was over 20%. Two-tailed tests were used for all variables, with a significance level of 5%.
ResultsDuring the study period, 184 emergency room visits with a diagnosis of hypoglycemia were recorded in 181 patients. Thirty-five of these cases were excluded because they involved patients with no diagnosis of DM, or because the emergency care report failed to confirm a capillary or plasma glucose level below 70mg/dl.
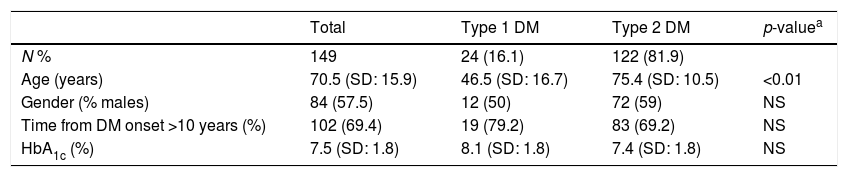
Table 1 shows the epidemiological and clinical characteristics of the patients. Of the 149 events included in the analysis, 122 (81.9%) occurred in patients with type 2 DM, 24 (16.1%) occurred in patients with type 1 DM, and 3 (2%) occurred in patients with other types of DM (post-transplant DM, diabetes secondary to pancreatic carcinoma, and DM secondary to mitochondrial disease). The mean patient age was 70.5 years (SD: 15.9). A total of 69.4% of the patients had been diagnosed with DM more than 10 years previously (the time from onset of the disease could not be established in two cases). A measurement of HbA1c obtained within the preceeding three months was available in 75 cases (50.3%), with a mean value of 7.5% (SD: 1.8).
Epidemiological characteristics of the studied patients.
| Total | Type 1 DM | Type 2 DM | p-valuea | |
|---|---|---|---|---|
| N % | 149 | 24 (16.1) | 122 (81.9) | |
| Age (years) | 70.5 (SD: 15.9) | 46.5 (SD: 16.7) | 75.4 (SD: 10.5) | <0.01 |
| Gender (% males) | 84 (57.5) | 12 (50) | 72 (59) | NS |
| Time from DM onset >10 years (%) | 102 (69.4) | 19 (79.2) | 83 (69.2) | NS |
| HbA1c (%) | 7.5 (SD: 1.8) | 8.1 (SD: 1.8) | 7.4 (SD: 1.8) | NS |
SD: standard deviation; DM: diabetes mellitus.
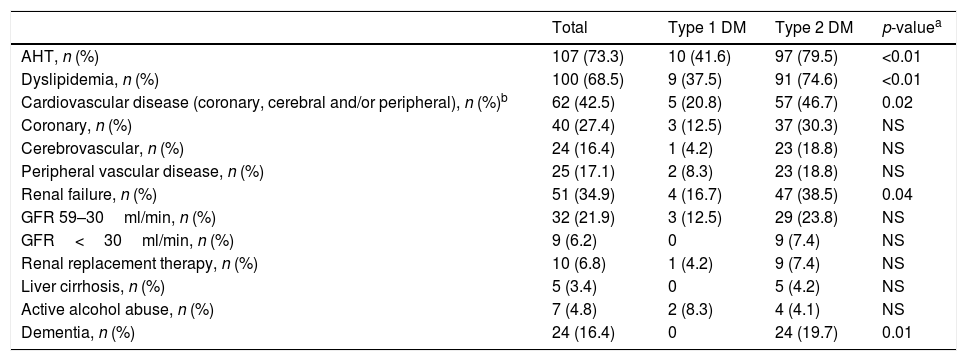
Patients with type 2 DM were older than those with type 1 DM (75.4 [SD: 10.5] vs. 46.5 [SD: 16.7] years; p<0.05), and had a lower HbA1c concentration, though the difference was not statistically significant (7.4% [SD: 1.8] vs. 8.1% [SD: 1.8) (p=0.08). Patients with type 2 DM had a greater prevalence of other cardiovascular risk factors, chronic complications and other comorbidities, except active alcohol abuse, though in some cases the differences were not statistically significant, probably because of the small number of cases involved (Table 2). Of note among the patients with type 2 DM was the prevalence of renal failure (38.5%) and cognitive impairment (19.7%), while the patients with type 1 DM showed a prevalence of alcohol abuse of 8.3%. A small percentage of patients (4.2% of those with type 2 DM) were diagnosed with liver cirrhosis. Nine percent of the patients with type 2 DM were institutionalized. A total of 12.7% of the patients had been admitted to hospital in the month before the emergency room visit (12 emergency medical admissions, 5 admissions for elective surgery, and two for emergency surgery). The difference in frequency of admission in the previous month between patients with type 2 and type 1 DM was not statistically significant (13.1% vs. 8.3%, respectively; p=0.7).
Associated disease conditions.
| Total | Type 1 DM | Type 2 DM | p-valuea | |
|---|---|---|---|---|
| AHT, n (%) | 107 (73.3) | 10 (41.6) | 97 (79.5) | <0.01 |
| Dyslipidemia, n (%) | 100 (68.5) | 9 (37.5) | 91 (74.6) | <0.01 |
| Cardiovascular disease (coronary, cerebral and/or peripheral), n (%)b | 62 (42.5) | 5 (20.8) | 57 (46.7) | 0.02 |
| Coronary, n (%) | 40 (27.4) | 3 (12.5) | 37 (30.3) | NS |
| Cerebrovascular, n (%) | 24 (16.4) | 1 (4.2) | 23 (18.8) | NS |
| Peripheral vascular disease, n (%) | 25 (17.1) | 2 (8.3) | 23 (18.8) | NS |
| Renal failure, n (%) | 51 (34.9) | 4 (16.7) | 47 (38.5) | 0.04 |
| GFR 59–30ml/min, n (%) | 32 (21.9) | 3 (12.5) | 29 (23.8) | NS |
| GFR<30ml/min, n (%) | 9 (6.2) | 0 | 9 (7.4) | NS |
| Renal replacement therapy, n (%) | 10 (6.8) | 1 (4.2) | 9 (7.4) | NS |
| Liver cirrhosis, n (%) | 5 (3.4) | 0 | 5 (4.2) | NS |
| Active alcohol abuse, n (%) | 7 (4.8) | 2 (8.3) | 4 (4.1) | NS |
| Dementia, n (%) | 24 (16.4) | 0 | 24 (19.7) | 0.01 |
DM: diabetes mellitus; GFR: glomerular filtration rate; AHT: arterial hypertension.
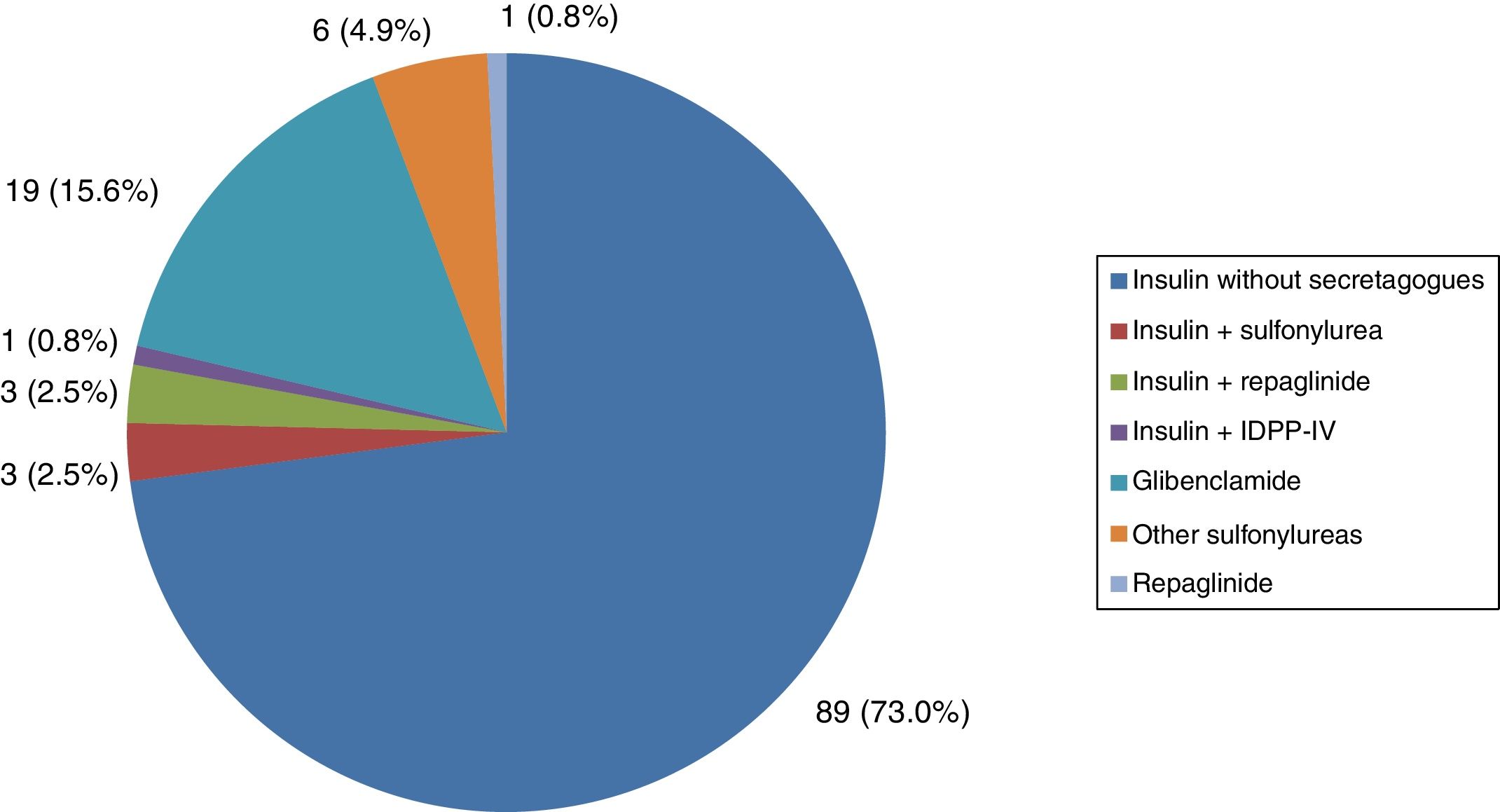
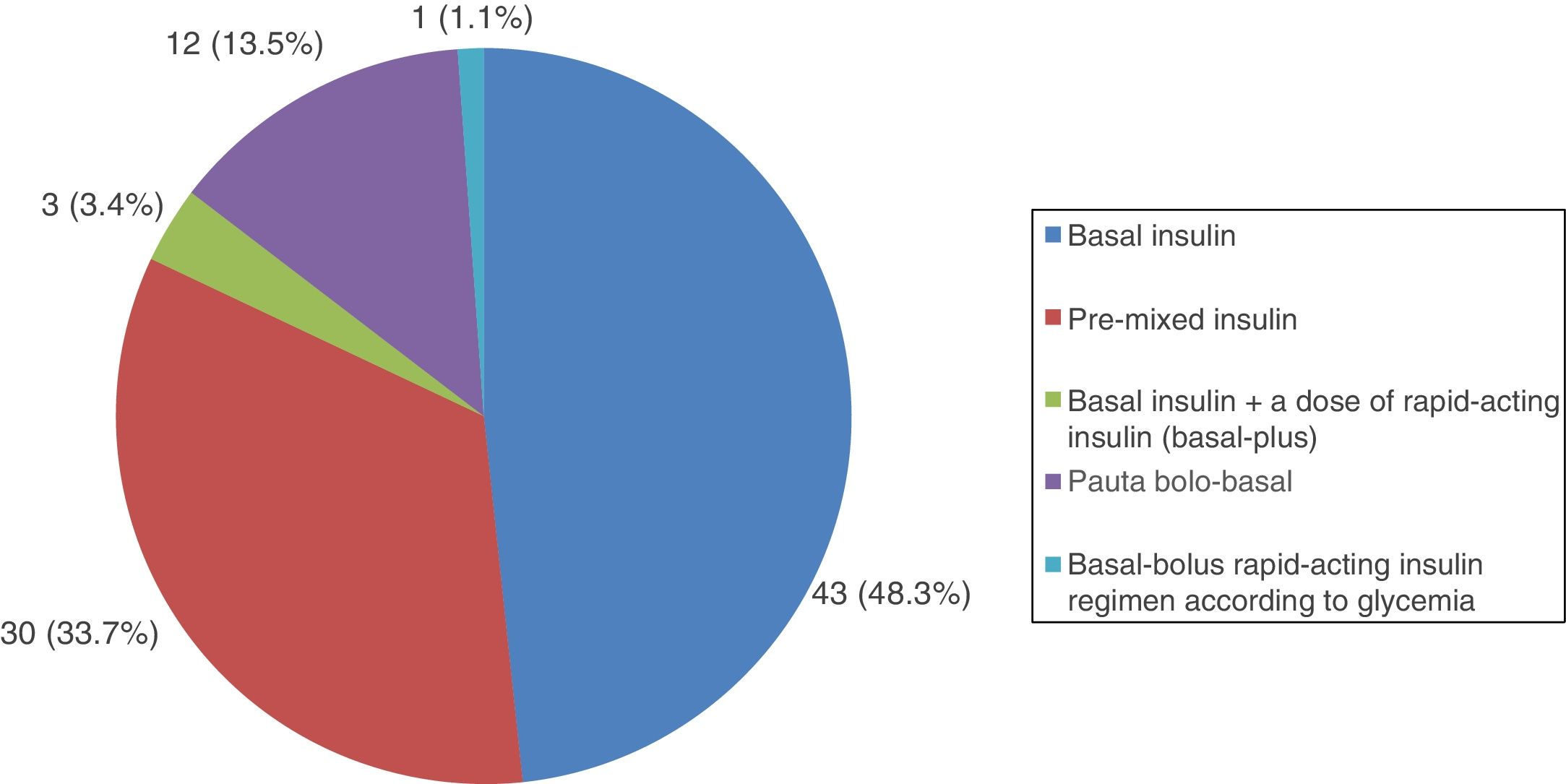
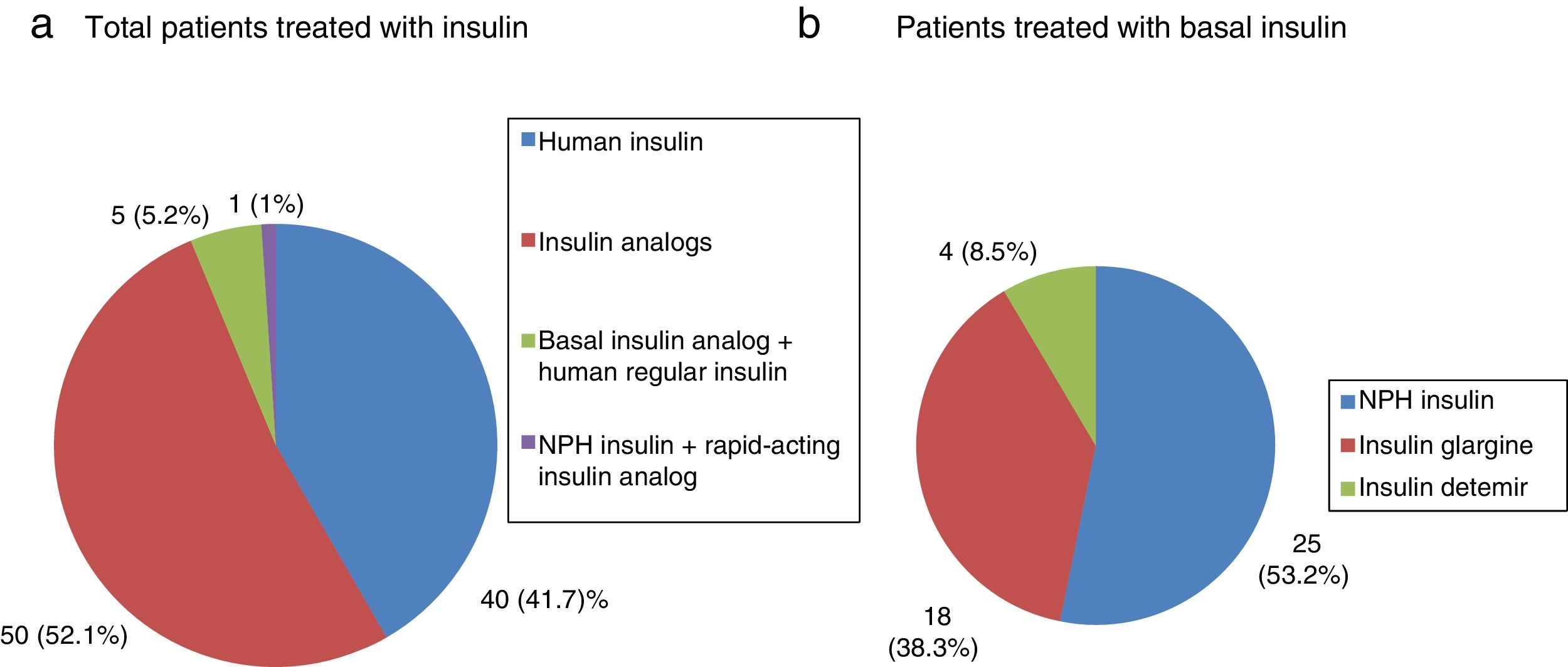
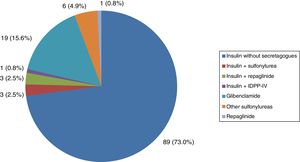
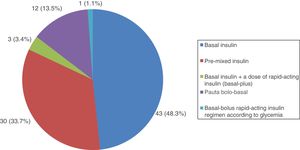
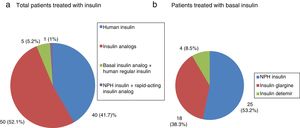
All patients with type 1 DM were treated with insulin, and the great majority (91.7%) followed a basal-bolus insulin regimen. In turn, 83.3% were receiving insulin analogs. Figs. 1–3 show the blood glucose-lowering therapies of the patients with type 2 DM. A high percentage (78.7%) of them were treated with insulin with or without other associated glucose-lowering drugs. Twenty-six patients with type 2 DM (21.3%) were treated with oral antidiabetic drugs alone. Of these 26 cases, 25 received sulfonylureas and one was treated with repaglinide. In 19 of the mentioned 25 cases (76%), the prescribed sulfonylurea was glibenclamide. Seven of the 47 patients with type 2 DM and renal failure (14.9%) were treated with sulfonylureas (glibenclamide in 5 cases and some other sulfonylurea in two patients). One of these 7 patients had stage IV renal failure (eGFR<30ml/min).
In 73.2% of the cases the presenting symptoms of hypoglycemia corresponded to neuroglycopenia. A hypoglycemia triggering factor was cited in 67 of the 149 cases analyzed (45%). The most common factors were decreased food intake (64.2%) and the intensification of insulin therapy (28.3%). Less common triggering factors were increased insulin secretagogue dosage (4.5%), the start of insulin therapy (4.5%), errors in patient antidiabetic treatment administration (3.3%), physical activity (2.4%), and an abusive intake of toxic substances (1.5%). In 9 of the 67 cases there was more than one triggering factor.
Eighty-four patients (56.4%) required medical transport to reach the emergency room. The treatment of the hypoglycemic episode was specified in 144 of the 149 cases. In 42 cases (29.2%) treatment was limited to oral carbohydrates. In the remaining 70.8% of the cases, parenteral treatment was administered (intravenous glucose and/or glucagon).
The mean duration of stay in the emergency room was 7.9h (SD: 5.4). Most patients (86.6%) were discharged home from the emergency room. Of the 20 patients requiring admission, 95% had type 2 DM. Of these, 42.1% were treated with oral antidiabetics alone, without insulin, and the majority (87.5%) received glibenclamide. The mean duration of hospital admission was 1.8 days (SD: 1.2).
DiscussionOur study shows that most hypoglycemic episodes seen in the emergency room of our center occurred in elderly type 2 DM patients with, a high prevalence of associated disease conditions, such as renal failure or cognitive impairment. In addition, they were mainly receiving insulin or sulfonylureas, particularly glibenclamide.
The individual risk of hypoglycemia is greater in patients with type 1 DM.10 However, type 2 DM accounts for 90% of all cases of diabetes; as a result, at the population level most hypoglycemic episodes occur in patients with type 2 DM. In addition, patients with type 1 DM are more accustomed to hypoglycemia, and therefore probably consult less often for this reason.
In our study, over 60% of the patients had suffered DM for more than 10 years, and the mean age of the patients with type 2 DM was 75.4 years. The prospective trial of the UK Hypoglycemia Study Group showed the frequency of hypoglycemia to be increased in patients with type 2 DM treated with insulin for more than 5 years, and similar to that in patients with recently diagnosed type 1 DM.11 Other studies have shown the incidence of severe hypoglycemia in patients with type 2 DM to increase with age and the duration of DM.12 It has been reported that the counter-regulatory hormonal response to hypoglycemia is activated at lower blood glucose levels in individuals over 65 years of age.13 In addition, type 2 DM is characterized by a gradual loss of pancreatic beta-cell function. This loss of beta-cell function is associated with a deficient counter-regulatory response to hypoglycemia, particularly as regards the glucagon secretion response of the pancreatic alpha-cells.14 These factors could contribute to an increased risk of hypoglycemia in older patients with more advanced DM.
A total of 34.9% of the global patients in our study and 38.5% of the patients in the type 2 DM subgroup had renal failure. Different studies have shown that chronic kidney disease increases the risk of severe hypoglycemia.15 The kidneys are involved in glucose homeostasis, contributing to neoglycogenesis and reabsorbing filtered glucose. In addition, many hypoglycemic drugs and/or their metabolites are excreted through the kidneys. Renal failure can alter these mechanisms, thereby favoring hypoglycemic events.16
Dementia was diagnosed in 19.7% of our patients with type 2 DM. There is evidence of an association between DM and dementia.17 A number of factors may contribute to an increased risk of dementia in patients with DM (vascular complications, the direct effect of hyperglycemia upon the central nervous system, insulin resistance). Hypoglycemia is one of the potential factors capable of influencing the relationship between DM and dementia. Hypoglycemic episodes can cause neuronal damage,18 which may be particularly relevant in elderly patients with limited neuronal plasticity. Hypoglycemia has also been associated with alterations in endothelial function and coagulation mechanisms that could promote brain ischemia.19 Prospective clinical studies have identified an epidemiological association between severe hypoglycemia and dementia.20 However, the relationship between dementia and hypoglycemia may be bidirectional, since patients with poorer cognitive function are more susceptible to hypoglycemia due to problems in recognizing the symptoms of hypoglycemia, identifying situations predisposing to hypoglycemia, and in adopting measures to correct the problem. The causal relationship therefore remains controversial.
Alcohol reduces neoglycogenesis and favors hypoglycemia. Furthermore, some studies have shown that alcohol aggravates the alterations of cognitive functions induced by hypoglycemia.21 These factors may explain why alcohol abuse is a relatively common associated factor in patients with type 1 DM, i.e., young patients with few associated disease conditions.
Some studies have shown hypoglycemia associated with drug treatment for DM to be one of the most common side effects in elderly patients after hospital discharge.22 In our study, 12.7% of the patients had been admitted in the month before the emergency room visit.
A total of 78.7% of the patients with type 2 DM were treated with insulin. The remaining 21.3% were treated with sulfonylureas or meglitinides (glibenclamide in the great majority of cases). Within the sulfonylureas, glibenclamide is associated with an increased risk of hypoglycemia. The clinical guides therefore advise the use of other second-generation sulfonylureas (glimepiride, gliclazide and glipizide),23 especially in patients with renal failure.24 Five of the 20 patients treated with glibenclamide in our study had renal failure. This situation is not exceptional in our setting. A recent study analyzed the prevalence of chronic kidney disease and the associated characteristics in patients over 65 years of age with type 2 DM in Spain. The study showed that although the use of sulfonylureas decreased as kidney function worsened, 10.5% of the patients treated with sulfonylureas had a GFR<45ml/min, a situation in which sulfonylurea use is not recommended. The same study found that 36.4% of the patients treated with glibenclamide had renal failure, despite the formal contraindication of glibenclamide use in this situation.25
Hypoglycemic events imply increased costs associated with DM.26 In this regard, 56.4% of the patients used medical transport to reach the emergency room, and the mean time spent in the emergency room was 7.9h. In turn, 13.4% of the patients required hospital admission, with a mean duration of stay of 1.8 days. The patients with type 2 DM treated with oral antidiabetics alone represented 21.3% of the global study cohort. However, in the case of the patients admitted to hospital, those treated with oral antidiabetics alone represented 42.1% of the cases, and of these, the great majority (87.5%) received glibenclamide. This situation is probably secondary to the long-acting effects of some sulfonylureas and/or their active metabolites.27
Our study has a number of limitations. In effect, this was a retrospective study with a limited number of cases, conducted at a single center, and in which the clinical information was compiled from the emergency care reports and the electronic case history. No recent HbA1c measurement was available in all cases for the analysis of glycemic control. Moreover, we only considered cases of hypoglycemia seen in the emergency room, i.e., not all episodes of hypoglycemia associated with DM treatment were represented, only the most severe cases. Furthermore, we only included cases with a documented capillary or plasma glucose concentration of <70mg/dl. This means that some excluded cases may also have been hypoglycemic episodes in which blood glucose was not recorded, or in which treatment was started in the presence of consistent symptoms despite the lack of prior confirmation of low blood glucose. In any case, our results are in agreement with those of prospective, multicenter studies in other countries that have evaluated the characteristics of patients seen in emergency departments due to hypoglycemia.28 A study conducted in the United States has validated a tool that classifies the risk of suffering hypoglycemia requiring an emergency room visit or hospital admission in patients with type 2 DM (low, intermediate or high risk).29 This tool uses 6 clinical variables including age, the use of insulin and/or sulfonylureas, and the degree of kidney function, all of which were relevant variables in our study.
In conclusion, most of the hypoglycemic episodes seen in the emergency room of our center occurred in elderly patients with type 2 DM and a high prevalence of other comorbidities, particularly renal failure and cognitive impairment, and who were treated with insulin and/or sulfonylureas (particularly glibenclamide). The individualization of DM treatment should take into account risk factors for hypoglycemia such as patient age, renal function and cognitive performance. If sulfonylurea therapy is indicated, glibenclamide should be avoided. In recent years, new glucose-lowering drugs (DPP-IV inhibitors, GLP-1 receptor agonists, SGLT2 inhibitors) and new insulin analogs (degludec, glargine U300) have become available, with benefits over other therapeutic options in relation to hypoglycemia risk.30–32 The limitations facing these new drugs are their greater cost and the fact that they have been introduced relatively recently. Nevertheless, they should be considered as a treatment alternative when avoiding hypoglycemia is an important issue.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Caballero-Corchuelo J, Guerrero-Pérez F, García-Sancho de la Jordana P, Pérez-Maraver M. Análisis de las características de los pacientes con diabetes mellitus que consultan por hipoglucemia en el servicio de urgencias de un hospital terciario. Endocrinol Diabetes Nutr. 2019;66:19–25.