There are several classifications based on thyroid ultrasound for selecting suspected malignant thyroid nodules. The Thyroid Imaging Reporting and Data System (TI-RADS) classification proposed by Horvath in 2009 includes 6 categories.
ObjetivesTo assess the sensitivity of the TI-RADS classification for diagnosing thyroid nodules.
MethodsA retrospective study of all patients who underwent thyroidectomy at our hospital (n=263) from September 2013 to December 2015. After thyroidectomy, histological results were correlated to the ultrasound findings reported.
ResultsOf the 263 study patients, 75 (28.5%) were diagnosed with thyroid cancer and 188 (71.5%) with benign disease. Correlation of histological results with preoperative ultrasound reports showed an initial sensitivity of 65%. After excluding 15 patients diagnosed with occult microcarcinoma, sensitivity increased to 81.6%. The ultrasound images from 11 false negatives cases were then reassessed by a radiologist who knew histological diagnosis and reclassified 10 of them as TI-RADS≥4. This procedure could have increased sensitivity up to 98.3%.
ConclusionsAlthough the sensitivity initially found in our study using the TI-RADS scale was relatively low, the value markedly improved when patients with occult microcarcinoma were excluded. Thus, use of the TI-RADS scale would allow for an adequate selection of patients amenable to fine needle aspiration of the nodule.
Existen distintas clasificaciones en ecografía tiroidea para la selección de nódulos tiroideos sospechosos de malignidad. La clasificación Thyroid Imaging Reporting and Data System (TI-RADS), descrita por Horvath en 2009, diferencia 6 categorías.
ObjetivosEvaluar la sensibilidad del método TI-RADS en el diagnóstico de patología nodular tiroidea.
Material y métodosEstudio observacional retrospectivo, que incluyó a todos los pacientes sometidos a tiroidectomía en nuestro centro (n=263), desde septiembre de 2013 a diciembre de 2015. Después de la tiroidectomía, los resultados histológicos se correlacionaron con los informes de las ecografías prequirúrgicas.
ResultadosDe los 263 pacientes incluidos en el estudio, tras la tiroidectomía 75 (28,5%) fueron diagnosticados de cáncer de tiroides y 188 (71.5%) de patología benigna. La correlación del resultado histológico con los informes de la ecografía prequirúrgica mostró una sensibilidad inicial del 65%. Tras excluir a 15 pacientes con diagnóstico de microcarcinoma oculto, la sensibilidad se incrementó hasta el 81,6%. Posteriormente, un radiólogo que conocía el diagnóstico histológico revisó las imágenes ecográficas de los 11 pacientes falsos negativos y reclasificó a 10 de ellos como TI-RADS≥4. Este procedimiento podría haber elevado la sensibilidad hasta un 98,3%.
ConclusiónAunque la sensibilidad de la escala TI-RADS obtenida inicialmente en nuestro estudio es relativamente baja, la exclusión de los pacientes con microcarcinoma oculto permite un notable incremento de su valor. De esta manera, la utilización de la escala TI-RADS permitiría una adecuada selección de pacientes subsidiarios de punción-aspiración con aguja fina.
The increasing availability of thyroid ultrasound (TU) and access to cytological analysis of thyroid gland nodules (TNs) through TU-guided fine needle aspiration biopsy (FNAB) has markedly changed the diagnostic and therapeutic approach to patients with thyroid cancer (TC). Prior to the systemic use of TU-guided FNAB cytological studies, the malignancy rate of surgically resected TNs did not exceed 15%.1 In contrast, at present, with the systematic use of preoperative cytology, the resected TN malignancy rate exceeds 50%.1
Thyroid gland nodules in themselves are not a disease entity; rather, they are the physical expression of a broad range of thyroid disorders. The prevalence of TNs detected by palpation is between 4 and 8% among the general population, a figure that increases to 19–67% with the use of TU, and up to 50% in autopsy samples.2,3 The incidence of TC in patients with TNs ranges from 5 to 15%.4
Due to the considerable overlap between the ultrasound findings of benignity and malignity, FNAB is required for the adequate clinical management of TNs. However, the high prevalence of nodular thyroid disease precludes the use of FNAB in all TNs. Thyroid ultrasound plays a key role in this regard, since it allows for the morphological characterization of TNs, thereby facilitating adequate selection of those nodules amenable to FNAB cytological diagnosis.5
The Breast Imaging Reporting and Data System (BI-RADS) was developed by the American College of Radiology in order to standardize breast lesion assessment and reporting. Adequate measures for each risk group (monitoring, biopsy, surgery, etc.) were established based on this system. The Thyroid Imaging Reporting and Data System (TI-RADS), developed by different authors,5,6 plays a role analogous to that of the BI-RADS. The present study uses the TI-RADS classification of Horvath (2009),6 which assigns a thyroid pathology score of grades 1–5 (with grade 6 corresponding to histologically confirmed TCs). In this regard, a high probability of TC is considered from grade 4, and FNAB is advised in the case of TNs with TI-RADS grades 4 and 5.7
The aim of the present study was to establish histological correlations with TU using the TI-RADS for TNs. The reference technique was taken to be the histopathological study of the thyroidectomy piece.
Material and methodsA retrospective review was made of the ultrasound reports of all the patients at our center who had total or partial thyroidectomy due to nodular thyroid disease in the period between September 2013 and December 2015.
At our center, the indications of thyroidectomy in patients with TNs are based on a protocol based on the ATA guides (2009),7 and include: FNAB of nodules corresponding to grades iv, v and vi of the Bethesda classification8; single or multinodular goiter with compressive symptoms or thyroid gland hyperfunction; and esthetic reasons or the patient's personal decision. Consequently, all the patients with FNAB findings indicative of malignancy were operated upon.
Prior to FNAB and/or surgery, all the patients underwent TU that was evaluated by various radiologists with different levels of experience in the use of the technique, though all were familiar with the TI-RADS.6 A Toshiba Aplio 500 Platinum ultrasound system was used, based on high grade Aplipure and Aplipure Plus technology (which captures the ultrasound beam electronically from different directions, reducing anisotropy artifacts) and speckle reduction (elimination of image noise), with a 14MHz PLT-1005 BT linear probe that uses differential harmonics, improving the definition of margins and tissue contrast resolution, with a decrease in acoustic shadows and noise. Although Doppler ultrasound was applied in most of the nodules as an available ultrasound tool, the absence of Doppler flow was not regarded as a criterion for the exclusion of TN malignancy. Axial images of both thyroid lobes were obtained, with quantification and measurement of all detected TNs. Systematic exploration was then made of the lateral neck lymph node chains, submaxillary glands and parotid glands. The following ultrasound characteristics were evaluated in each TN to obtain the corresponding TI-RADS grade:
- 1)
Ultrasound structure
- 2)
Echogenicity
- 3)
Morphology
- 4)
Anteroposterior/transverse diameter ratio
- 5)
Contours
- 6)
Presence/absence of a capsule
- 7)
Calcifications
- 8)
Hyperechogenic foci
- 9)
Vascularization
Nodule size was not included among the evaluated ultrasound characteristics, since it is not predictive of malignancy.9,10
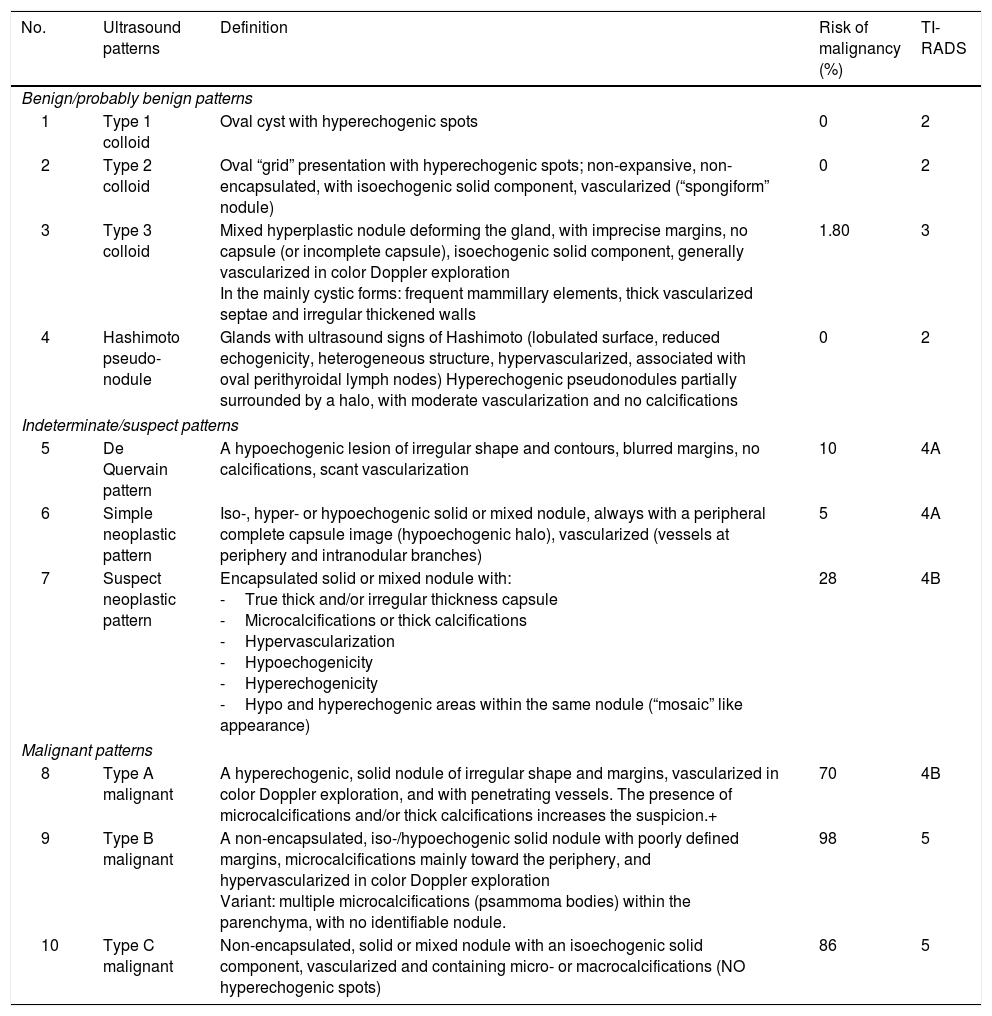
A TI-RADS score per patient was recorded, corresponding to the nodule of the highest TI-RADS grade. Table 1 shows the TI-RADS classification6 used in this study, and includes the management recommendations for each TI-RADS grade.
Horvath TI-RADS classification.6
| No. | Ultrasound patterns | Definition | Risk of malignancy (%) | TI-RADS |
|---|---|---|---|---|
| Benign/probably benign patterns | ||||
| 1 | Type 1 colloid | Oval cyst with hyperechogenic spots | 0 | 2 |
| 2 | Type 2 colloid | Oval “grid” presentation with hyperechogenic spots; non-expansive, non-encapsulated, with isoechogenic solid component, vascularized (“spongiform” nodule) | 0 | 2 |
| 3 | Type 3 colloid | Mixed hyperplastic nodule deforming the gland, with imprecise margins, no capsule (or incomplete capsule), isoechogenic solid component, generally vascularized in color Doppler exploration In the mainly cystic forms: frequent mammillary elements, thick vascularized septae and irregular thickened walls | 1.80 | 3 |
| 4 | Hashimoto pseudo-nodule | Glands with ultrasound signs of Hashimoto (lobulated surface, reduced echogenicity, heterogeneous structure, hypervascularized, associated with oval perithyroidal lymph nodes) Hyperechogenic pseudonodules partially surrounded by a halo, with moderate vascularization and no calcifications | 0 | 2 |
| Indeterminate/suspect patterns | ||||
| 5 | De Quervain pattern | A hypoechogenic lesion of irregular shape and contours, blurred margins, no calcifications, scant vascularization | 10 | 4A |
| 6 | Simple neoplastic pattern | Iso-, hyper- or hypoechogenic solid or mixed nodule, always with a peripheral complete capsule image (hypoechogenic halo), vascularized (vessels at periphery and intranodular branches) | 5 | 4A |
| 7 | Suspect neoplastic pattern | Encapsulated solid or mixed nodule with: -True thick and/or irregular thickness capsule -Microcalcifications or thick calcifications -Hypervascularization -Hypoechogenicity -Hyperechogenicity -Hypo and hyperechogenic areas within the same nodule (“mosaic” like appearance) | 28 | 4B |
| Malignant patterns | ||||
| 8 | Type A malignant | A hyperechogenic, solid nodule of irregular shape and margins, vascularized in color Doppler exploration, and with penetrating vessels. The presence of microcalcifications and/or thick calcifications increases the suspicion.+ | 70 | 4B |
| 9 | Type B malignant | A non-encapsulated, iso-/hypoechogenic solid nodule with poorly defined margins, microcalcifications mainly toward the periphery, and hypervascularized in color Doppler exploration Variant: multiple microcalcifications (psammoma bodies) within the parenchyma, with no identifiable nodule. | 98 | 5 |
| 10 | Type C malignant | Non-encapsulated, solid or mixed nodule with an isoechogenic solid component, vascularized and containing micro- or macrocalcifications (NO hyperechogenic spots) | 86 | 5 |
The surgical pieces were examined by two pathologists who specialized in thyroid gland disease and with over 10 years of experience. The fresh thyroidectomy specimens were sent to the Department of Pathology along with clinical information on the patient. The pieces were stained and sections were obtained every 1cm, parallel to the sagittal plane, followed by fixation in formalin solution for 24–48h. Each nodule was identified and analyzed individually. We recorded the morphology, size, color and consistency of each nodule, as well as the presence of a capsule, calcifications, and the location of the nodule within the gland. A microscopic study was subsequently made of all the identified nodules, and a report was produced with the histopathological diagnosis, according to the classification of the World Health Organization (WHO).11
Once the results were obtained, and in order to secure maximum sensitivity with the TI-RADS in our series, a single radiologist with over 9 years of experience in TU and interventional procedures, and who was aware of the histological diagnosis of the TNs, re-evaluated the TU images of the patients with TC and presurgery TI-RADS<4. Consequently, there was no masking of the final diagnosis.
The data were entered in an MS Excel 2013 spreadsheet, including demographic variables, ultrasound signs, TI-RADS grade and histological results. These qualitative variables were described with their percentage distribution. Filters were used to classify the patients with positive results (TI-RADS≥4 at ultrasound) as true positive cases with malignant histological findings or false positive cases with benign histological findings. The patients with negative results (TI-RADS<4) were, in turn, classified as true negative cases with negative histological findings or false negative cases with malignant histological findings. The validity of the diagnostic test was subsequently analyzed with calculation of the sensitivity.
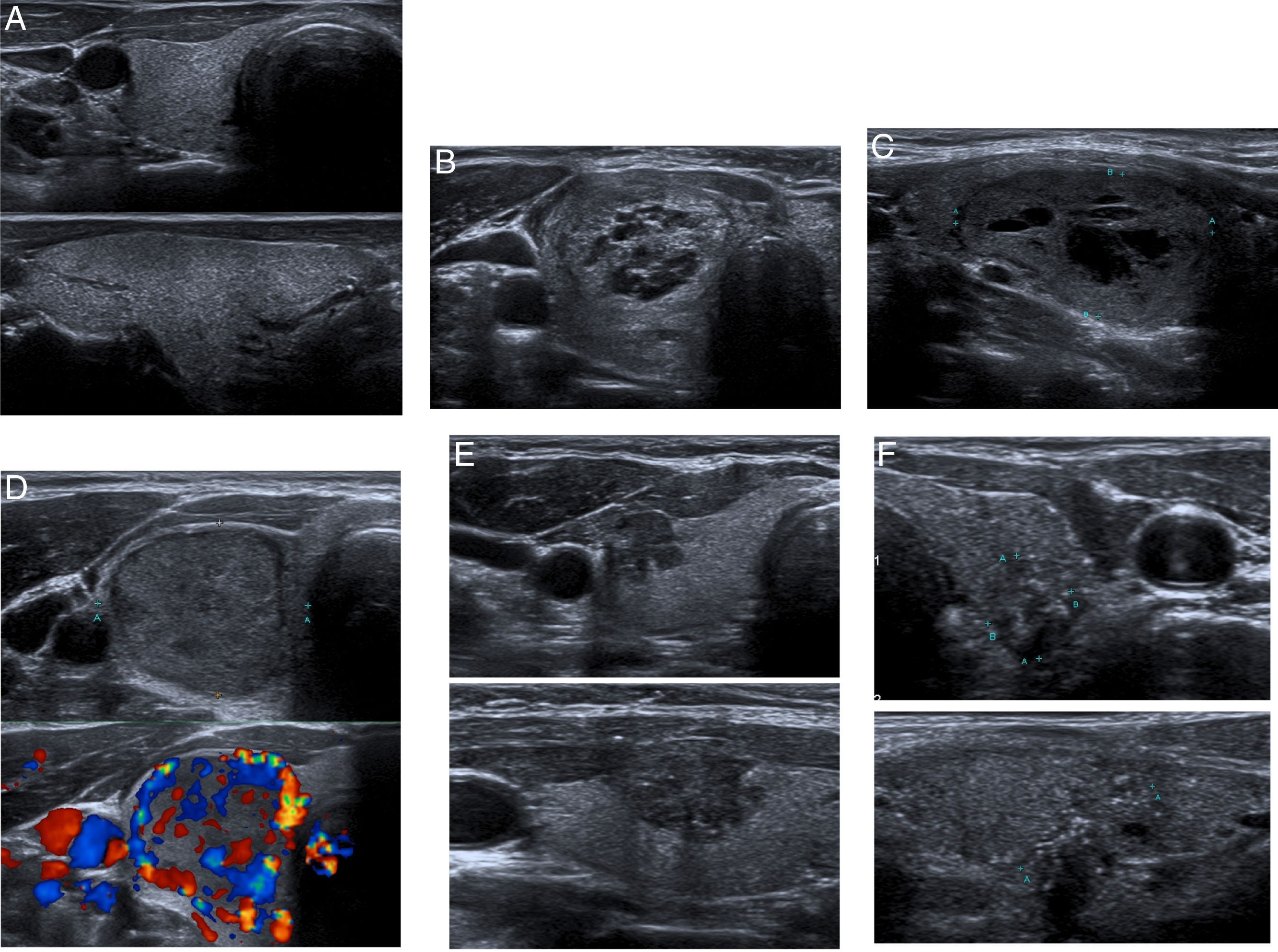
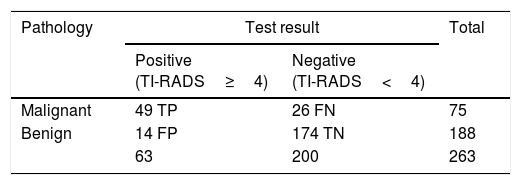
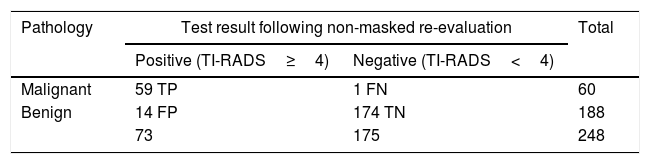
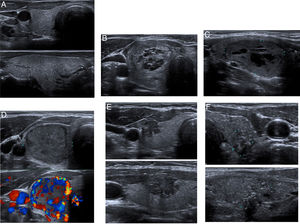
ResultsA total of 263 patients were included in the study. The histological results revealed 188 benign lesions and 75 malignant lesions. We grouped TI-RADS grades 1, 2 and 3 as “negative test” and grades 4 and 5 as “positive test”. Therefore, the lesions with benign histopathological findings and classified as TI-RADS<4 represented true negative cases, and those with malignant histopathological findings and classified as TI-RADS≥4 represented true positive cases. Accordingly, of the 75 patients with TC, 49 (65.3%) were reported as TI-RADS≥4 (true positive cases) and 26 (34.7%) as TI-RADS<4 (false negative cases). Of the 188 patients with benign thyroid gland disease, the presurgery TI-RADS grade was <4 in 174 patients (true negative cases=92.5%) versus ≥4 in 14 patients (false positive cases=7.5%) (Table 2). Fig. 1 shows the ultrasound images of several nodules included in the study, which constitute examples of the different TI-RADS grades.
Initial results. Number of patients with positive or negative testing according to a TI-RADS grade of over or under 4.
| Pathology | Test result | Total | |
|---|---|---|---|
| Positive (TI-RADS≥4) | Negative (TI-RADS<4) | ||
| Malignant | 49 TP | 26 FN | 75 |
| Benign | 14 FP | 174 TN | 188 |
| 63 | 200 | 263 | |
FN: false negative; FP: false positive; TN: true negative; TP: true positive.
Examples of TI-RADS grades. A. Axial (top) and longitudinal images (bottom) of a normal thyroid gland. No thyroid nodules are seen. TI-RADS 1. B. Oval mixed nodule exhibiting a “spongiform” appearance, with an isoechogenic solid component. TI-RADS 2. Type 2 colloid pattern. C. Oval mixed hyperplastic nodule, partially encapsulated, and exhibiting a slightly hypoechogenic main solid component. TI-RADS 3. Type 3 colloid pattern. D. Axial acquisitions in B mode (top) and color Doppler (bottom). An encapsulated, hypoechogenic, discretely heterogeneous and hypervascularized solid nodule. TI-RADS 4B. Suspect neoplastic pattern. E. Axial (top) and longitudinal images (bottom). A non-encapsulated, hypoechogenic solid nodule with poorly defined margins, and with a number of peripheral microcalcifications. TI-RADS 5. Type B malignant pattern. F. Axial (top) and longitudinal images (bottom). Multiple disperse microcalcifications within the parenchyma, with no identifiable nodule. TI-RADS 5. Type B malignant pattern.
The initial sensitivity of TU was 65%.
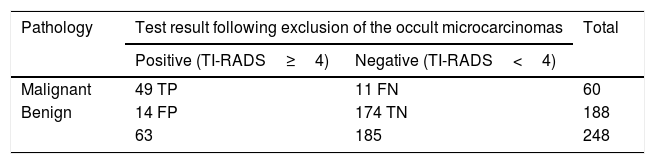
Following re-evaluation of the TU images of the 26 patients with TC and presurgery TI-RADS<4 (FN), 15 cases (58%) were identified as incidental microcarcinomas measuring <1cm, occult within the multinodular goiter, and 11 (42%) were identified as carcinomas measuring ≥1cm in size. Following a review of the ultrasound images, the 15 microcarcinomas maintained TI-RADS<4, since they were undetectable because of their small size and/or the concomitant findings of multinodular goiter or chronic thyroiditis, these being circumstances that mask the presence of TNs. For this reason the 15 microcarcinomas were excluded from the analysis, causing sensitivity to increase to 81.6% (Table 3).
Results following exclusion of the occult microcarcinomas. Number of patients with positive or negative testing according to a TI-RADS grade of over or under 4.
| Pathology | Test result following exclusion of the occult microcarcinomas | Total | |
|---|---|---|---|
| Positive (TI-RADS≥4) | Negative (TI-RADS<4) | ||
| Malignant | 49 TP | 11 FN | 60 |
| Benign | 14 FP | 174 TN | 188 |
| 63 | 185 | 248 | |
FN: false negative; FP: false positive; TN: true negative; TP: true positive.
Of the 11 carcinomas representing false negative cases (4 TI-RADS grade 2 and 7 TI-RADS grade 3), the TI-RADS grade was reclassified as ≥4 in 10 of the 11 patients (91%). These 10 patients were added to the initial 49 cases, causing sensitivity to increase to 98.3%.
Tables 3 and 4 respectively show the histopathological results and TI-RADS grades before and after re-evaluation of the ultrasound images of the TNs.
Results after retrospective re-evaluation of the ultrasound images corresponding to the false negative cases (not masked with respect to the histological findings). Number of patients with positive or negative testing according to a TI-RADS grade of over or under 4.
| Pathology | Test result following non-masked re-evaluation | Total | |
|---|---|---|---|
| Positive (TI-RADS≥4) | Negative (TI-RADS<4) | ||
| Malignant | 59 TP | 1 FN | 60 |
| Benign | 14 FP | 174 TN | 188 |
| 73 | 175 | 248 | |
FN: false negative; FP: false positive; TN: true negative; TP: true positive.
Our study reveals sensitivity values in detecting malignant disease in TNs that are lower than those found in the literature, where all studies report values of over 85%.5,12 However, if we had excluded the 15 cases of occult papillary microcarcinoma (lesions not visible at TU and therefore not amenable to correlation with the histological findings, which was the primary objective of our study), sensitivity would have increased to 81.6%. The presence in our series of 10 TNs with a histological diagnosis of microcarcinoma, which following re-evaluation were reclassified as sonographically suspect of malignancy (TI-RADS≥4), could have further boosted sensitivity to 98.3%. However, awareness of the final diagnosis on the part of the radiologist, as well as the absence of masking procedures, reduced the validity of this ultrasound re-evaluation of the TNs.
A similar study carried out in Spain, albeit comparing the TI-RADS classification with the FNAB findings instead of the histological results, obtained similar results, particularly in the high suspicion category (TI-RADS≥4), where percentage malignancy was 86% (30/35) versus 77% (49/63) in our study.13
With regard to the false negative cases, it should be noted that 15 of the TNs with TC corresponded to microcarcinomas that were not identified due to the concomitant findings of multinodular goiter or chronic thyroiditis. These circumstances complicate the identification and characterization of TNs according to the TI-RADS criteria, a diagnostic limitation also found in other TN ultrasound classifications.14 It should also be mentioned that in our study we assigned a TI-RADS grade per patient, corresponding to the nodule of the highest TI-RADS grade. As a result it would not have been possible to establish a correlation between a non-visualized nodule and the histopathological results of the thyroidectomy piece. Since the main objective of our study was to correlate TU to the histological findings of TNs, we excluded the mentioned 15 microcarcinomas, thereby increasing significantly the sensitivity obtained.
Our study has several limitations. Firstly, this is a retrospective study, which implies selection bias, since many benign TNs are not subjected to thyroidectomy. This circumstance precluded the calculation of other parameters such as specificity and predictive values. Another limitation was the participation of different radiologists with different levels of experience in evaluating thyroid gland disease. This implies possible inter-observer variability (not quantified in our study) and the heterogeneity of the results obtained.
Finally, we have not been able to compare our results with those of other groups using ultrasound classifications different from the TI-RADS, such as those proposed by the guides of the American Thyroid Association14 or the British Thyroid Association.10 To the best of our knowledge, no publications in Spain have used these latter classifications.
In conclusion, our study showed the initial sensitivity of the employed TI-RADS classification to be low, and, therefore, as not allowing for the optimum screening of patients with TNs who could benefit from FNAB, thereby avoiding unnecessary procedures. However, after excluding the occult microcarcinomas, the sensitivity of this tool increased significantly and proved similar to that reported in other studies where the TI-RADS was effectively found to be useful in screening for patients amenable to FNAB. In any case, it must be emphasized that, independently of the sensitivity of the different scales, the use of some of the instruments proposed by the international scientific bodies would appear to be absolutely necessary.
Financial supportNone.
Conflicts of interestNone.
Please cite this article as: García-Moncó Fernández C, Serrano-Moreno C, Donnay-Candil S, Carrero-Alvaro J. Estudio de correlación de los resultados histológicos con los hallazgos ecográficos en nódulos tiroideos. Clasificación TI-RADS. Endocrinol Diabetes Nutr. 2018;65:206–212.