To access the prevalence of restless legs syndrome (RLS) in patients on chronic hemodialysis and to determine the risk factors for RLS.
Materials and methodsFifty subjects undergoing chronic maintenance hemodialysis were included in this study after seeking informed consent. RLS was diagnosed according to International Restless Legs Syndrome study group criteria. Demographic data, clinical history and laboratory values are collected using standard interviews.
ResultsRLS was reported in 14 of 50 hemodialysis patients (28%). Low hemoglobin, low serum ferritin levels and increased consumption of coffee in hemodialysis patients correlated significantly with onset of RLS. There was no difference in age, gender and duration of hemodialysis between RLS and non-RLS patients.
ConclusionRLS is prevalent in patients on chronic hemodialysis. Further studies are needed to confirm the possible risk factors for RLS.
Abordar la prevalencia del síndrome de las piernas inquietas (SPI) en pacientes sometidos a hemodiálisis crónica y determinar los factores de riesgo del síndrome.
Materiales y métodosEn el presente estudio, tras obtener el consentimiento informado, se incluyeron 50 pacientes sometidos a hemodiálisis de mantenimiento, crónica. El SPI se diagnosticó de acuerdo con los criterios definidos por el grupo International Restless Legs Syndrome Study. Utilizando entrevistas estándar se obtuvieron los datos demográficos, la historia clínica y los valores de laboratorio.
ResultadosSe documentó el síndrome en 14 de los 50 pacientes (28%) sometidos a hemodiálisis. En estos pacientes, unos valores bajos de hemoglobina, valores séricos bajos de ferritina y un mayor consumo de café se correlacionaron significativamente con el inicio del síndrome. No hubo diferencias significativas de edad, sexo y duración de la hemodiálisis entre pacientes con y sin SPI.
ConclusiónEn pacientes sometidos a hemodiálisis crónica el síndrome es prevalente. Se requieren más estudios para confirmar los posibles factores de riesgo de SPI.
RLS is a sensori-motor disorder defined as a disorder characterized by disagreeable leg sensations, usually prior to sleep onset, that cause an almost irresistible urge to move the legs.1 It may result from a decrease in dopaminergic modulation of intracortical excitability, with reduced supraspinal inhibition and increased spinal cord excitability.2
RLS is a common symptom in dialysis patients. The symptoms are deep paresthesias, creeping and crawling sensations or even pain in the calves and legs that occur exclusively when the legs are inactive, such as during hemodialysis.3 Although the tendency to move can be temporarily suppressed, it is ultimately irresistible; movement of the legs yields prompt relief. The results of clinical and electromyographic examinations in RLS are generally unremarkable. The purpose of present study is to evaluate the prevalence of RLS in patients with end stage renal disease (ESRD) on maintenance hemodialysis.
Materials and methodsThe present study was conducted on chronic hemodialysis population in a tertiary care hospital based dialysis unit. This is an observational study, conducted at Vaatsalya Hospital, Hassan, Karnataka State, India from January 2012 to December 2012. Hospital Research and Ethics Committee approved this study. Fifty stable adult ESRD patients undergoing maintenance hemodialysis were observed over 12 months. Patients suffering from any medical or neurological disorder that predisposes them to develop RLS, consuming any medicines that can induce RLS, and those unwilling to participate are excluded from this study.
RLS was diagnosed according to the criteria published by the International Restless Legs Syndrome study group.4 This criteria includes: urge to move legs, relief in the urge by movement, increment of urge during rest, and circadian variation with maximum symptom during evening or night. Only those cases that fulfilled the above criteria were diagnosed as having RLS.
All patients’ demographic data were recorded. Clinical history, drug history and family history of RLS were recorded. Biochemical investigations including complete hemogram, serum ferritin levels, serum calcium, serum phosphorus and blood urea levels were recorded. All events on dialysis and at home were noted.
Statistical analysisAnalysis was performed using SPSS software 17.0. The mean and standard deviation are reported for continuous variables and number and percentage are reported for categorical variables. Chi-square test was used to compare 2 variables and P value of <0.05 was considered as significant.
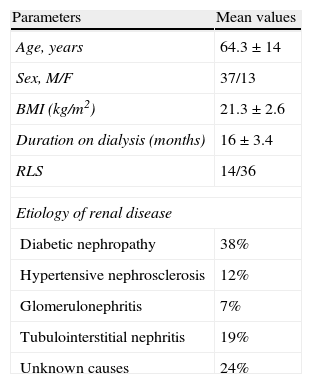
ResultsFifty patients who are on maintenance hemodialysis (MHD) were included in this study. Prevalence of RLS in this study was 28%. Mean age of the patients studied was 64.3±14 years. Mean duration on MHD was 15 months. Diabetes (38%) was the most common cause for ESRD. Their demographic data are shown in Table 1.
Patient characteristics.
| Parameters | Mean values |
| Age, years | 64.3±14 |
| Sex, M/F | 37/13 |
| BMI (kg/m2) | 21.3±2.6 |
| Duration on dialysis (months) | 16±3.4 |
| RLS | 14/36 |
| Etiology of renal disease | |
| Diabetic nephropathy | 38% |
| Hypertensive nephrosclerosis | 12% |
| Glomerulonephritis | 7% |
| Tubulointerstitial nephritis | 19% |
| Unknown causes | 24% |
M: males; F: females; BMI: body mass index; RLS: restless legs syndrome.
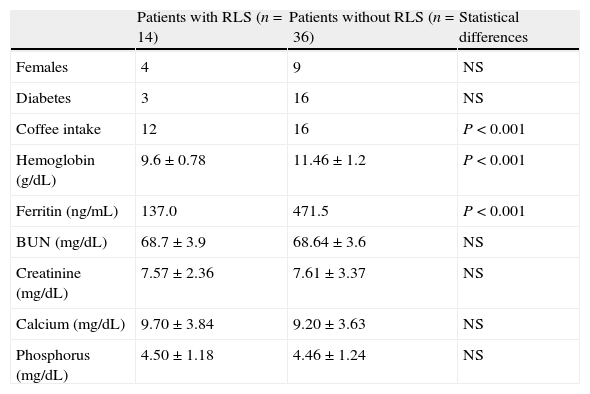
There was no difference between the genders with regard to prevalence of RLS. Statistically significant correlations were found between RLS and low hemoglobin level, low serum ferritin level and high coffee intake. There was no significant difference with respect to age, duration of dialysis and levels of serum creatinine, BUN (blood urea nitrogen), serum calcium and serum phosphorus levels among subjects with and without RLS (Table 2).
Biochemical data and their statistical significance in patients with and without RLS.
| Patients with RLS (n=14) | Patients without RLS (n=36) | Statistical differences | |
| Females | 4 | 9 | NS |
| Diabetes | 3 | 16 | NS |
| Coffee intake | 12 | 16 | P<0.001 |
| Hemoglobin (g/dL) | 9.6±0.78 | 11.46±1.2 | P<0.001 |
| Ferritin (ng/mL) | 137.0 | 471.5 | P<0.001 |
| BUN (mg/dL) | 68.7±3.9 | 68.64±3.6 | NS |
| Creatinine (mg/dL) | 7.57±2.36 | 7.61±3.37 | NS |
| Calcium (mg/dL) | 9.70±3.84 | 9.20±3.63 | NS |
| Phosphorus (mg/dL) | 4.50±1.18 | 4.46±1.24 | NS |
BUN: blood urea nitrogen; NS: not significant.
This study found that the prevalence of RLS among hemodialysis patients is 28%. This prevalence is much higher when compared to RLS in general population in Asian community (0.9–8.9%).5 Prevalence of RLS in our study is higher than earlier study conducted among dialysis patients in India.6 Such differences between these studies could be due to variations in the susceptibilities to develop RLS among study population, different dialysis strategies used as well as the diagnostic criteria applied in the studies.
Most research on the disease mechanism of restless legs syndrome is being focused on the iron system.7 The most commonly associated medical condition is iron deficiency, which accounts for 20% of all cases of RLS.8 In our study significant number of patients with RLS had lower hemoglobin levels as well as lower serum ferritin levels. In a study conducted by Al-Jahdali et al., significant patients with RLS had positive correlation with regular coffee intake.9 Statistically significant association was found between RLS and regular coffee intake in our study. However, Gigli et al. failed to show any association between coffee intake and RLS.10
RLS often persists after initiation of dialysis but may improve after transplantation. RLS has been linked to abnormalities in calcium and phosphorus metabolism.11 Folate deficiency, vascular insufficiency, sleep apnea, uremia and diabetes have also been implicated to cause RLS. Recent studies have failed to confirm these findings.12 Our study also failed to confirm the association of RLS with serum calcium, phosphorus, urea and creatinine levels. RLS has strong female predisposition in earlier studies.13 However, in our study we did not find any difference between genders.
There are several limitations to our study.
- 1.
The sample size is small and hence, results are difficult to be generalized to whole ESRD community; there are no specific tests for RLS.
- 2.
Data obtained were through interview and neurological examination. However, recall bias cannot be excluded in this study.
- 3.
Influence of certain medications such as antiemetic's (antidopaminergic), antihistamines and antidepressants cannot be ruled out, as many of our patients during the study period are on some of these medications.
Our study suggests that RLS occurs in a significant portion of chronically dialyzed patients. Our study also suggests that RLS was significantly associated with high caffeine intake and with iron deficiency anemia. As a consequence of RLS, most patients have insomnia, and some suffer from anxiety or mild depression and have a poor quality of life. Considering the importance of RLS in overall patient quality of life, the percentage of patients in each unit who experience RLS should be tracked as a quality assurance initiative.
Conflict of interestThe authors have no conflict of interest to declare.