The paramount importance of vascular access (VA) within the complex world of haemodialysis has always been underscored, as well as the need to have the collaboration of an expert vascular surgeon in this type of intervention to be able to achieve long-lasting and efficient VAs with the least possible complications. However, another group of health practitioners involved in this topic, the group comprised of the nursing team of the haemodialysis room and of the Nephrology Service, is often, possibly involuntarily, left in a second plane, undervaluing their medical care. In my opinion, this is a tremendous mistake, as I consider that the role of haemodialysis nursing is essential, due to their close relationship with the patients, as they experience the day-to-day renal replacement therapy with them, and they act as a link between the patient and the nephrologists and vascular surgeons that attend to them.
I have not acquired this concept, which situates haemodialysis nursing as an essential ally of the vascular surgeon, from one day to the next, rather it is something that I have assumed and reinforced throughout the years that I have been engaged in carrying out VAs for dialysis. As an example of this, at the ADER1 meeting that was held in Barcelona in 2003, I already mentioned that:“If in doubt, dialysis patients must firstly ask Nursing, then the Nephrologist, and finally the Vascular Surgeon”.
Later, at the National Congress of Angiology and Vascular Surgery that was held in Cadiz in 20072, one of the round tables addressed VA for dialysis. As a participant and speaker on the table, and in the section on monitoring VA, I indicated that the role of dialysis nursing is essential during the late postoperative period, as they can evaluate a series of aspects of the VA by means of physical examination: “Maturation and inspection of the VA: it is useful to detect an oedema of the limb, the appearance of collateral circulation, aneurysms in the venous section. They can also control the intensity of the thrill, and characteristics of the access murmur”.
Later on, the paper on “New Contributions to the Consensus on Vascular Accesses of the Spanish Society of Dialysis and Transplant” presented at the III Course on Vascular Accesses for Dialysis held in Bilbao in 20083, stated that Guideline no. 5 of the Consensus says: “Dialysis nursing must evaluate VA before each dialysis. The role of Nursing in the dialysis room, in all aspects related to VA, is vital”.
These opinions could represent a purely personal viewpoint and therefore, of relative value. However, there are other authors that coincide with this same idea. This same opinion is expressed in different articles by D. Waterhouse, from the Renal Unit of the Hospital Royal Infirmary in Manchester4, F. Murphy, School of Nursing Trinity College in Dublin5, CJ Richard and J. Engebretson from the Woman¿s University of Houston, Texas6, and D. Carlton from the Renal Unit of St. Mary's Hospital in London7. They all confirm my idea that dialysis nursing is an essential and basic ally for vascular surgeons engaged in the construction and maintenance of the VA.Nursing and Dialysis
There are two facets in connection with dialysis where nursing care is basic: the pre-dialysis consultation and the dialysis room
1Pre-dialysis consultationNowadays, in all Nephrology Services that have a dialysis unit, there is a pre-dialysis consultation carried out by nurses, where patients are informed about all aspects related to their renal disease. Thus, as the patient considers the nursing staff to be more accessible than the nephrologist, the information offered initially by the specialist physician is completed and increased. After verifying the patient's cultural level, their degree of understanding and acceptance of the disease, and the habits and social support involved, they are informed of all that related to terminal chronic renal insufficiency, they are offered different therapeutic possibilities, such as transplant and peritoneal dialysis, and haemodialysis, and the replacement renal therapies are explained to them in detail. This is a way of collaborating in the patient's final decision, as they are informed of the advantages and disadvantages of both dialysis systems, so they have as much information as possible to be able to choose between them. If haemodialysis is the method chosen, the nursing service then prepares the visit to the vascular surgeon, when the type of VA and the implantation place will de decided upon. Patients will also be informed of the characteristics of the surgical intervention.
2Dialysis RoomThere are two situations that the nursing staff must supervise within the dialysis room, after starting the replacement renal therapy:
- -
Control of the immediate post-operative period after carrying out the VA, if the patient has started dialysis with a temporary catheter due to worsening of the chronic renal insufficiency without having constructed the definite VA.
- -
Monitoring of the functionalism and detection of possible complications that the VA may present during its use.
Within the immediate post-operative period, the nursing staff assess the aspect of the surgical wound, watch over the appearance of possible early complications, such as infection of the access, distal ischemia, or thrombosis, confirm its correct functioning and that the maturation is suitably progressing, removing the skin suture at the right time. They can also begin to inform the patient about the peculiarities of the use of the VA when the time comes to start their punctures.
Once the patient has started the replacement renal therapy with dialysis, the nursing staff will inspect the VA during each session, to monitor its function and be able to detect any possible complications that may arise with time, and be able to correct them before they lead to losing the access.
The control of the VA may be:
- -
Physical: by inspecting the access, it is possible to detect oedemas and increase the collateral circulation in the limb, both of which suggest a proximal venous lesion, hardened areas in the cutaneous decubitus venous routes in the puncture area, the appearance of aneurysmatic areas, etc. By palpation, we can objectify any possible alterations and changes in the VA thrill, normal difficulties in puncture, and extension of the post-puncture haemostasia time, all of which point towards problems in the VA, leading to the need to carry out additional examinations to diagnose the type of lesion and the treatment required.
- -
Instrumental: this consists in the daily verification of the functionalism parameters of the VA that are measured in the dialysers. The nursing staff performs a strict control of the flow that the access offers, to detect possible reductions during several dialyses, which would point towards a probable stenosis. They also control possible increases in blood pressure, also confirmed throughout several dialysis sessions, and that are suggestive of the existence of a proximal venous lesion.
As I have mentioned above, both VA surveillance modalities have a priority objective, and that is to detect the appearance of possible complications in the VA, and be able to correct them before they cause any definite loss. There are different types of complications.
- -
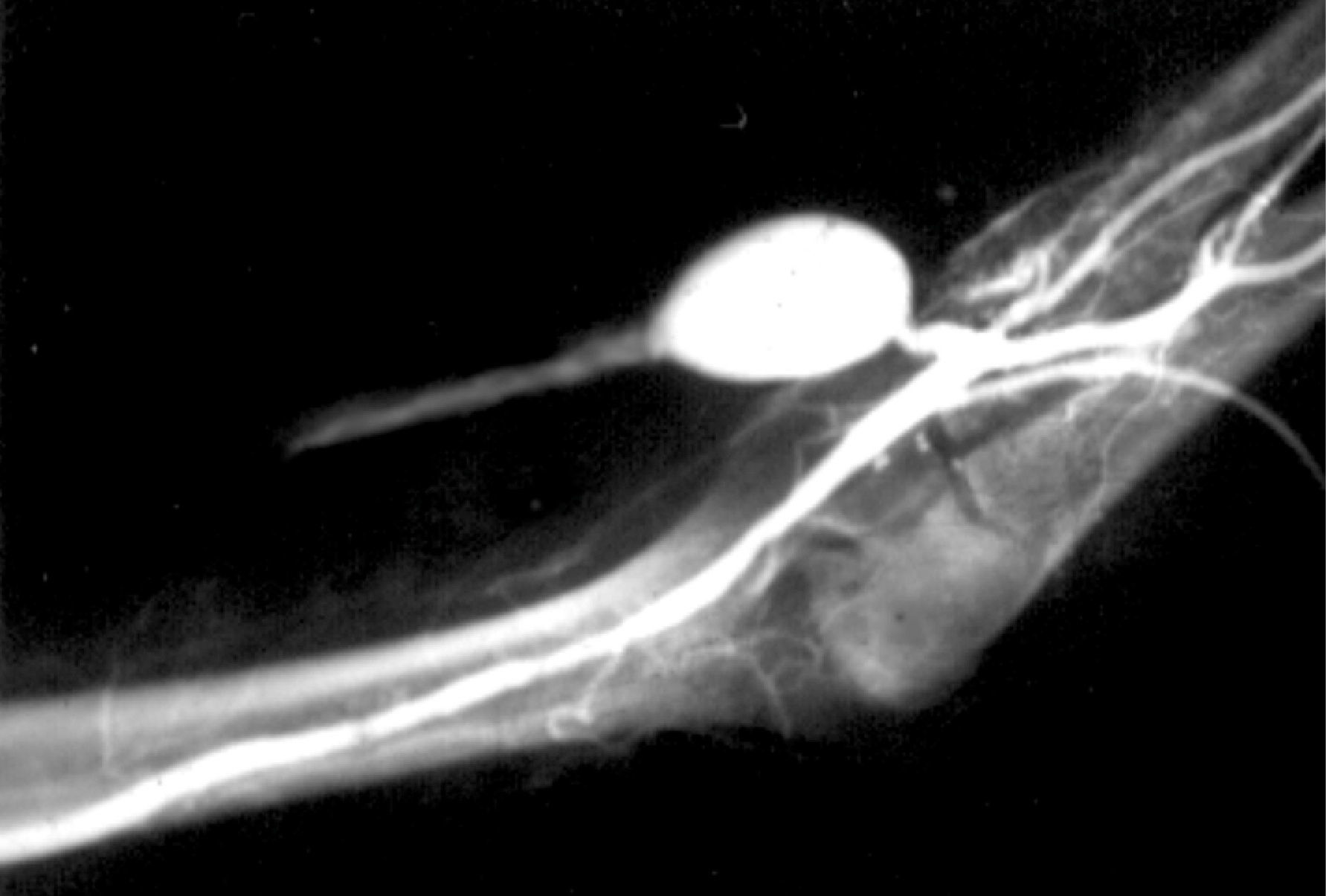
Stenosis or thrombosis of the VA (fig. 1).- This is the most frequent incident with respect to occurrence and also to severity, as it may cause the lack of VA8. The nursing service, given its closeness to the patient, will be the first health department to detect this problem, either due to the reduction in flow or the detection of thrombosis, and they will urgently inform the vascular surgeon to assess the treatment to be followed, and if there are possibilities of carrying out a VA rescue.
- -
Infection of the VA (figs. 2 & 3).- Very infrequent complication in native VA9, about 3%, and somewhat more frequent, around 22%, in prosthetic accesses10. In both cases, it is usually related to infections of the puncture points, and therefore dialysis nursing will detect it in the haemodialysis sessions, informing the nephrologist or vascular surgeon for them to indicate the appropriate treatment.
- -
Distal ischemia (fig. 4).- This appears in a small number of patients, around 1%11, who are generally diabetic, on whom a VA at humerus level is performed. This is triggered because the majority of the arterial flow derives from the VA in proximal direction, leaving the distal part of the limb and basically the hand, in ischemia situation, which may give rise to pain during the dialysis, coldness, paresthesia and, in extreme cases, the appearance of digital trophic lesions. Once again, it is the dialysis nursing that is the first to detect this, either due to the symptoms mentioned by the patient or just by inspecting the hand.
- -
Aneurysms (fig. 5).- They usually occur through the venous route12 and more rarely at anastomotic level. They are due to the actual dilation that occurs in the vein after the arteriovenous fistula has been created, and are favoured by the repeated punctures, that weaken the venous wall. They are subject to treatment if they reach a large size, which would increase the risk of thrombosis of the VA, or else, if they cause the appearance of decubitus in the skin, with the subsequent risk of breaking the skin and bleeding. The nursing staff, during the sessions in the dialysis room, and by inspecting the VA, will evaluate them, will monitor them, and will inform the nephrologists and vascular surgeons when they consider this necessary.
Based on all the information set out above, it is deduced that the function that the nursing service carries out in all that related to haemodialysis is really relevant and of vital importance, at all levels. We have verified that in the pre-dialysis phase they carry out an essential job of informing and educating patients and their families, solving doubts and concepts that might have been left unclear during the visit with the nephrologists, as they represent a care level that is perhaps more accessible for patients.
And during the haemodialysis, they are the ones that detect and warn of the complications that may occur in the VA, given that every 48 hours they are in direct contact with the patient and their VA. Also, and from the psychological support perspective, their work is essential, as the prolonged contact with the patient converts them into the receivers of their doubts, fears as well as their medical and even personal type problems. Based on all of this, I believe that they are the natural link between the patient, nephrologist and vascular surgeon, and returning to the initial paragraph, I am firmly convinced that dialysis nursing is an essential ally of the vascular surgeon, and this is how they must be considered, recognising that the extraordinary work they carry out in this field of Medicine is extremely valuable.