The stellate ganglion block has multiple indications for pain management. The technique has evolved from using anatomical landmarks to image-guided puncture with fluoroscopy and ultrasound.
Ultrasonography is a very useful tool that allows for real time visualization of the vascular structures (carotid, vertebral artery), the visceral structures (esophagus) and thus helps in preventing puncture injuries. This article offers a description of the indications, the ultrasound-guided technique and complications under the author's point of view.
El bloqueo del ganglio estrellado tiene múltiples indicaciones para el manejo del dolor, para este fin la técnica ha evolucionado desde la realización por medio de referencias anatómicas, hasta la punción guiada por imágenes como son el fluoroscopio y la ecografía.
La ultrasonografía es una herramienta muy útil ya que se puede ver en tiempo real las estructuras vasculares (carótida, arteria vertebral), las estructuras viscerales (esófago) y así evitar puncionarlas. En el presente artículo se hará una descripción de las indicaciones, la técnica guiada por ultrasonografía y las complicaciones, bajo la perspectiva del autor.
The stellate ganglion block is a frequently used technique for the treatment of chronic pain. It was originally described in the 1930s by Leriche in the US and by Fontaine in Europe,1 to relieve causalgic pain and the reflex sympathetic dystrophy of the upper limbs.
Whilst fluoroscopy is a reliable method for identifying the nerve structures, ultrasound allows for the identification of the vertebral vessels, the thyroid gland and vessels, the longus colli muscle, the nerve roots and the esophagus. Therefore, ultrasound may prevent the inadvertent puncture of these structures, a risk that may arise with the blind technique or via fluoroscopy.2
Several techniques have been used to block the lower sympathetic cervical chain. The 2 most frequent ones are the transverse process of C6 and the anterior or paratracheal approach at the level of C7, with or without fluoroscopy.2
Ultrasound is a tool to view the structures, guide the needle advancing in real time, and confirm the injection and distribution of the medication, avoiding both the health practitioner and the patient's exposure to radiation.3
The purpose of this article is to describe the most salient aspects of the stellate ganglion ultrasound-guided block, its indications, and contraindications.
AnatomyUnderstanding the anatomy of the cervical-thoracic sympathetic chain and ganglion is key to determine whether the neural block was therapeutic and to avoid unnecessary nerve ablation procedures.4
The cervical sympathetic trunk or the cervical sympathetic chain is a cephalic continuation of the thoracic sympathetic trunk located in a bundle space.5,6
It is made up by three ganglia:6
- •
The superior cervical ganglion, the largest of the three ganglia, is spindle shaped, measures 2–5cm long and is usually located across the first vertebra and is associated with the 4 superior cervical vertebrae.
- •
The middle cervical ganglion is occasionally absent, never exceeds 10mm long and is placed below and in front of Chassaignac's tubercle at the level of the sixth cervical vertebra. When present it is associated with C5–C6.
- •
The inferior cervical ganglion is constant, usually located in front of the 7th cervical vertebra and the 1st thoracic vertebra, fused with the first thoracic ganglion forming an irregular mass con el primer (spider-like shape).7
In about 80% of the population this inferior cervical ganglion fuses with the first thoracic ganglion to form a single structure, the cervical-thoracic ganglion or stellate ganglion.8,9
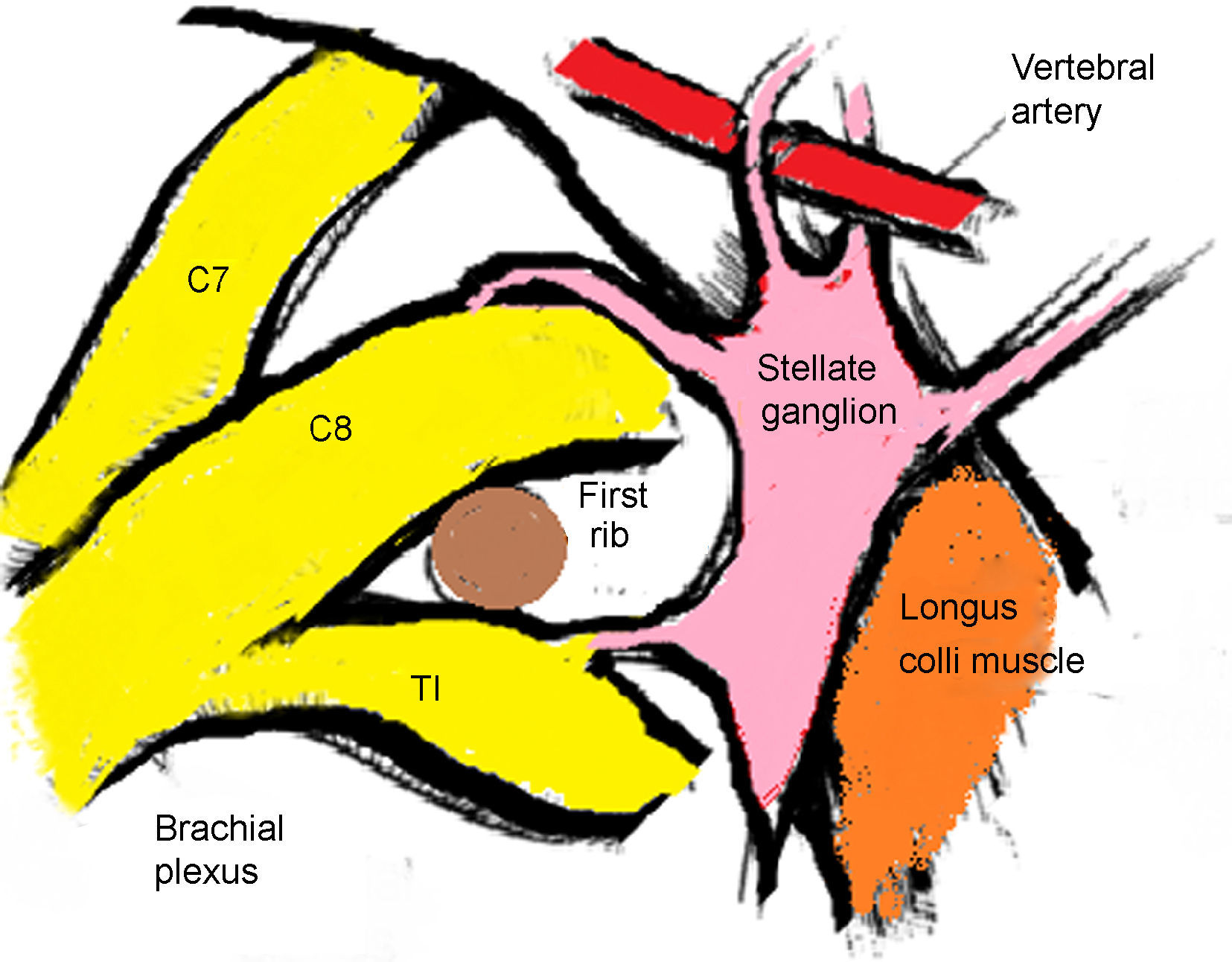
The stellate ganglion is located medial to the scalene muscles, lateral to the longus colli muscle and the trachea, together with the laryngeal recurrent nerve, anterior to the transverse process; the inferior most section is located posteriorly to the superior margin of the first section of the subclavian artery and at the origin of the vertebral artery, posterior to the apex of the lung. At the level of C6 it is in close relation with the anterior tubercle of Chassaignac and at the level of C7 is more medial at the level of the anterolateral aspect of the vertebral body 10 (Fig. 1).
The stellate ganglion measures approximately 2.5cm×1cm×0.5cm. It is located in front of the neck of the first rib extending to the union of the seventh cervical vertebra and the first thoracic vertebra. However, its shape and location vary depending on the individual. It is localized lateral and posterior to the lateral border of the long muscle of the neck.11 The ganglion may have a spindle, triangular of globular shape.9
The most important vascular relationships are the carotid and vertebral arteries located at the level of C7. However, there can be a 10% anatomical variation when the vertebral artery enters above C7. It should be noted that incomplete osteogenesis might be present at the level of C7 so a medial-most approach should be maintained to prevent puncturing of the vertebral artery.10
The longus colli muscle is the muscular landmark usually lateral to the ganglion and varying in thickness from 5 to 10mm in C6 and from 8 to 10mm in C7. The total depth from the subcutaneous cell tissue to the transverse process at C6 usually does not exceed 16.6mm.10
The sympathetic fibers of the head, neck and lower limbs cross the stellate or cervical-thoracic ganglion.10,12
The efferent postganglionic nerve fibers go cross the head, the neck, the upper limbs and the heart. The sympathetic postganglionic nerve endings release noradrenaline as the transmitter substance.13,14
The stellate ganglion block causes a more complete denervation of the head and neck structures. However, there are a considerable number of people in whom somatic intrathoracic branches of the second nerve come together with the first spinal thoracic nerve. These intrathoracic branches join the gray communicating vessels of the sympathetic fibers and arise from the second sympathetic thoracic ganglion and probably from the ganglion at T3. These fibers join the lower section of the brachial plexus without crossing the stellate ganglion. This explains the incomplete block of the upper extremities when only the block of the stellate ganglion proper is done.11
Indications- •
Complex regional pain syndrome type 1 and type 2 of the upper extremities.10,11,13,15,16
- •
Herpes Zoster-associated pain.10,17,18
- •
Ischemic neuropathies.10,13
- •
Post-radiation neuritis.10,11
- •
Atypical facial pan, orofacial pain syndrome, including neuropathic orofacial pain.10,11,13
- •
Sympathetic nerve maintained pain.10,11
- •
Vascular failure/occlusive vascular disorder, both acute and chronic of the upper extremities, Raynaud's disease.11,19
- •
Quinine poisoning.11,13,20
- •
Phantom limb.11,13
- •
Hyperhidrosis of the upper limb.11,19
- •
Cardiac arrhythmias: cardiac ischemic pain, long QT syndrome.10,11,13
- •
Neuropathic pain syndromes due to cancer pain.13,18
- •
The patient refuses to undergo the procedure.11
- •
Poor knowledge of the technique and of the anatomy.10,11
- •
Acquired coagulopathy (anticoagulant therapy without bridge treatment).10,11
- •
Congenital coagulopathy.11
- •
Localized infection.10,11
- •
Drug allergies (local anesthetic or steroids).10,11
- •
Unable to sign the informed consent.10
- •
Lineal transducer (high frequency 8–12MHz)
- •
4–5cm long short bevel 22, 23 or 25G gauge needle6,13; 22 gauge spinal needle may also be used.21
- •
Selection of medicines: Lidocaine (1–2%) and bupivacaine (0.25%) have been used for the stellate ganglion block. 22 Lidocaine is a fast-acting short-duration anesthetic (1–3h), usually with less cardiovascular side effects. Bupivacaine has a longer life, lasting 2–3 times more that lidocaine. However, Bupovacaine has high cardiovascular risks but it has become increasingly popular for stellate ganglion and other nerve blocks because of its excellent differential block of various nerve fibers and relative long action.23 The systemic effects of lidocaine or bupivacaine over the central nervous system and the cardiovascular system are not increased at a 10ml dose, unless there is intravascular spread. 23
- •
Other drugs: Local anesthetic (0.5% – bupivacaine, 0.5% ropivacaine, 0.25–0.75% levobupivacaine)3,10,21,24–26 and steroid (methylprednisolone)27; however, some authors do not recommend the use of steroids.10
- 1.
The patient is placed in decubitus supine position or in lateral decubitus, with the head slightly extended (a small pillow may be used between the shoulders) and it has to be neutral or slightly rotated toward the opposite side of the procedure.
- 2.
Adequate asepsis of the neck is performed and sterile dressings are applied.
- 3.
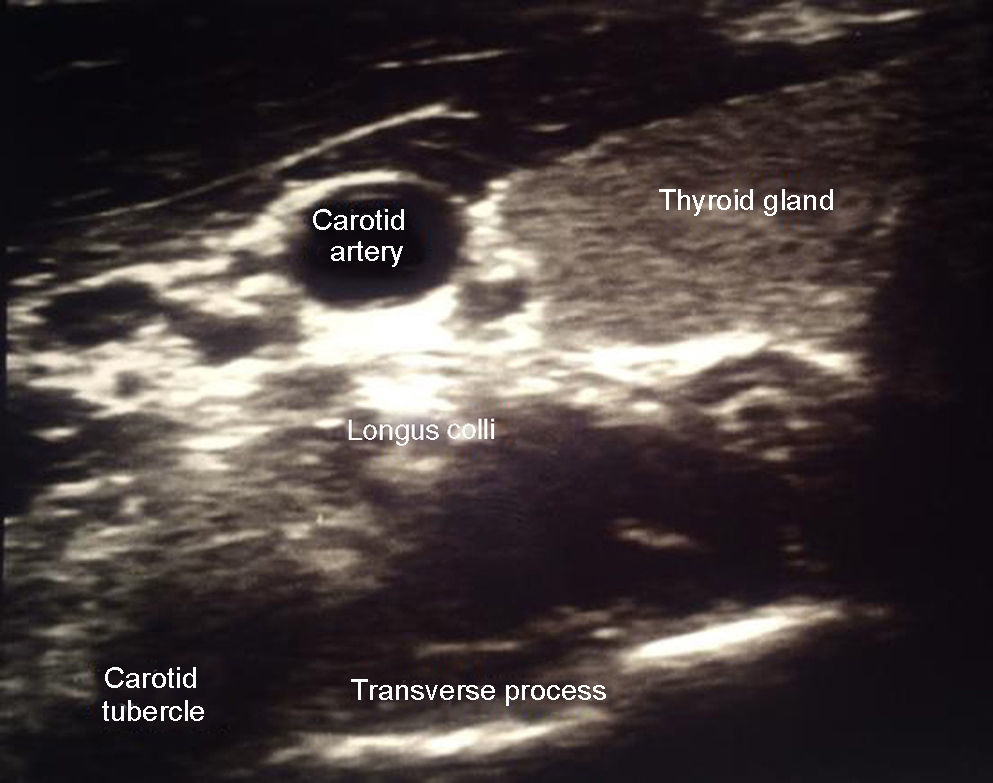
An initial scan is performed to identify structures: thyroid, carotid artery and jugular vein.
- 4.
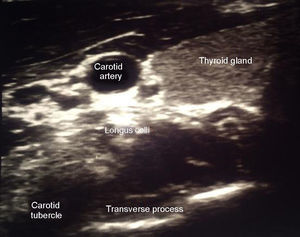
The transverse process at C6 has been identified because of its prominent anterior tubercle, different from C5 that is flat and C7 that does not have a tubercle10 (Fig. 2).
- 5.
The long muscle of the neck or longus colli is found above the transverse process of C6.
- 6.
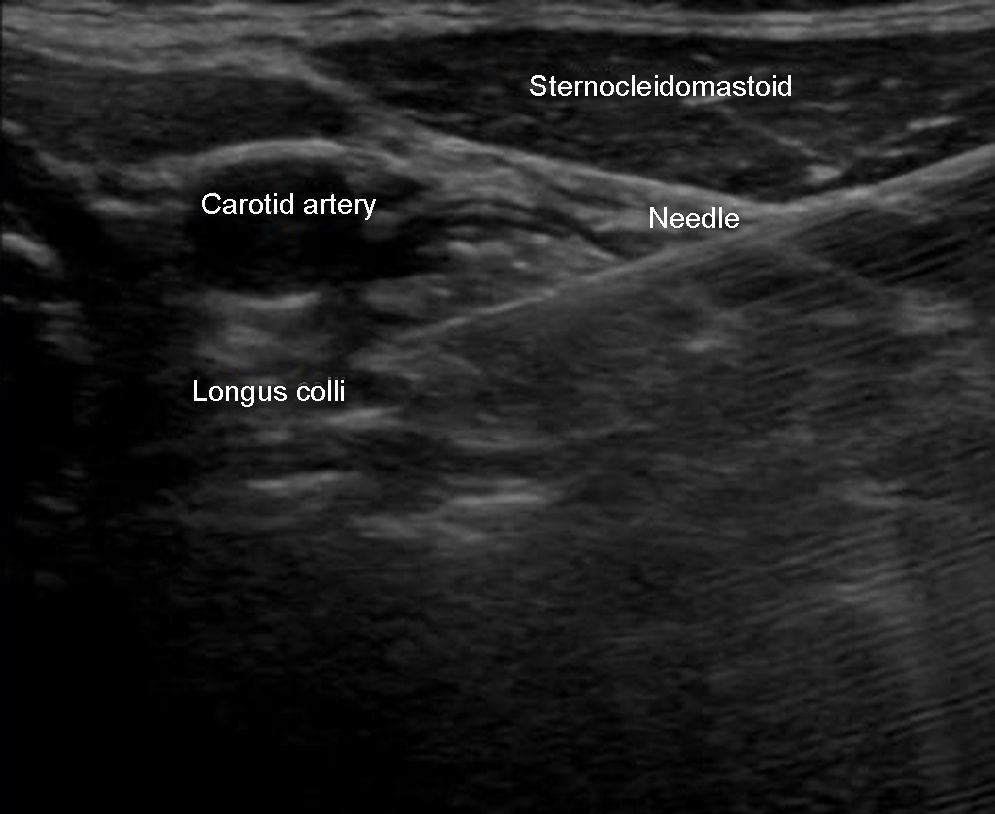
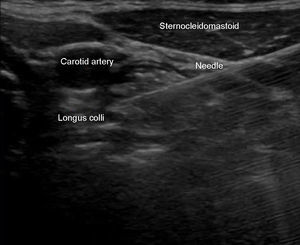
Plain approximation is used to observe the needle path; or, in some cases, outside the plane such as in the case of patients with a high body mass index (Fig. 3).
- 7.
Ideally the puncture should be on the plane to see the tip of the needle at all times; the needle is directed medially until it passes through the deep cervical fascia, above the longus colli muscle.
- 8.
Approximately 5ml of drug are injected, observing the dissection between the carotid artery and the longus colli muscle.
- 9.
The patient is transferred to the recovery room for 30–60min to assess any potential complications.
The stellate ganglion block may be performed several times, according to the pathology and the patient's response. When the response is adequate but the effect is short lasting, radiofrequency may be considered.28
Signs of a successful blockComplicationsInjury to the surrounding nerves and viscera: brachial plexus injury, trachea and esophagus trauma, injury to the pleura or lung and bleeding or local hematomas.12
- •
The presence of Horner's syndrome is a sign of block success but should also be seen as a side effect.
- •
Dysphonia and a feeling of dysphagia may occur as a result of the recurrent laryngeal nerve. This is the main reason why a bilateral block should not be performed since it may result in a loss of the pharyngeal reflexes and subsequent respiratory involvement.
- •
Brachial plexus block leads to somatic block. If this occurs, the patient shall be instructed to avoid inadvertent trauma.
- •
The intravascular injection of the local anesthetic agent is associated to toxicity; the epidural injection usually enters the foramen with anterolateral angulation, intrathecal injection with neuroaxial block.
- 1.
Transient hoarseness and a foreign body sensation in the throat (recurrent laryngeal nerve block).
- 2.
Horner's syndrome unpleasant effects (miosis, ptosis, enophthalmos).
- 3.
Hematomas.
- 1.
Brachial plexus effects.
- 2.
Phrenic nerve block.
- 3.
Pneumothorax.
- 4.
Osteitis of the transverse process.
- 1.
Intra-arterial injection: immediate neurological effects, loss of consciousness, seizures.
- 2.
Epidural/intratecal injection slow presentation of symptoms.
The stellate ganglion block is a procedure frequently used for pain management. Though there are multiple complications associated with the technique, currently the procedure can be safer using ultrasonography.
Conflicts of interestThe author has no conflicts of interest to declare.
FundingNone.
Please cite this article as: Serna-Gutiérrez J, Bloqueo ganglio estrellado guiado por ultrasonografia. Rev Colomb Anestesiol. 2015;43:278–282.