Drug interactions represent the cornerstone in the basic anesthetic triangle and knowledge about such interactions contributes to a solid foundation for administering medications.
This article dwells on the anesthetic drug interactions: pharmaceutical (mixing or not mixing), pharmacokinetic (alterations in distribution, metabolism, or clearance), pharmacodynamics (synergism, additive effect) and thermodynamic (affinity and intrinsic activity).
The basic anesthetic triangle is a current concept and drug interactions are the cornerstone for safe anesthesia. These interactions are currently neglected and hence the anesthetist should recognize any drug interactions for a safer practice of anesthesia.
Las interacciones farmacológicas constituyen los pilares de la tríada básica de la anestesia y su conocimiento contribuye a tener unas bases sólidas en la administración de medicamentos.
El presente artículo tiene como objetivo hacer una reflexión sobre las interacciones farmacológicas en anestesia: Farmacéuticas (mezclar o no mezclar), farmacocinéticas (alteración en la distribución, metabolismo o eliminación), farmacodinámicas (sinergismo, adición) y termodinámicas (afinidad y actividad intrínseca).
La tríada básica de la anestesia es un concepto vigente y sus interacciones farmacológicas son los pilares de una anestesia segura. En la actualidad estas interacciones no se tienen en cuenta, razón por la cual es pertinente que el anestesiólogo las tenga presente para hacer un ejercicio más seguro de los medicamentos que administra.
We are living through an unprecedented event in anesthesiology, leaving the dark ages behind – when opening or closing a vaporizer was decided on a whim, where an intravenous drug was administered on a “little bit” or “a fair amount” or “not too much” basis, and the teaching of anesthesia depended on the expertise of the professor with many years of experience, who would finally have found the magic formula to administer a cocktail of drugs to meet the surgeon's needs.1 Now we speak in terms of concentrations, targets, probability of non-response (PNR), synergism, etc. These are all terms supported by scientific trials that are the basis for teaching anesthesia and are repeated generation after generation. However, in order to understand those terms, it is essential to know the foundations of administering safe anesthesia, which basically can be summarized into “INTERACTIONS”.
The concept of anesthesia with three basic components as described by Gray, is essential for a sound anesthetic technique.2,3 These components have been expanded through the years4,5; nevertheless, they continue to revolve around the three fundamental components: hypnosis, analgesia, and relaxation. Understanding the interaction among these basic components paves the way to a clear understanding of the range of responses elicited when administering anesthetic agents.
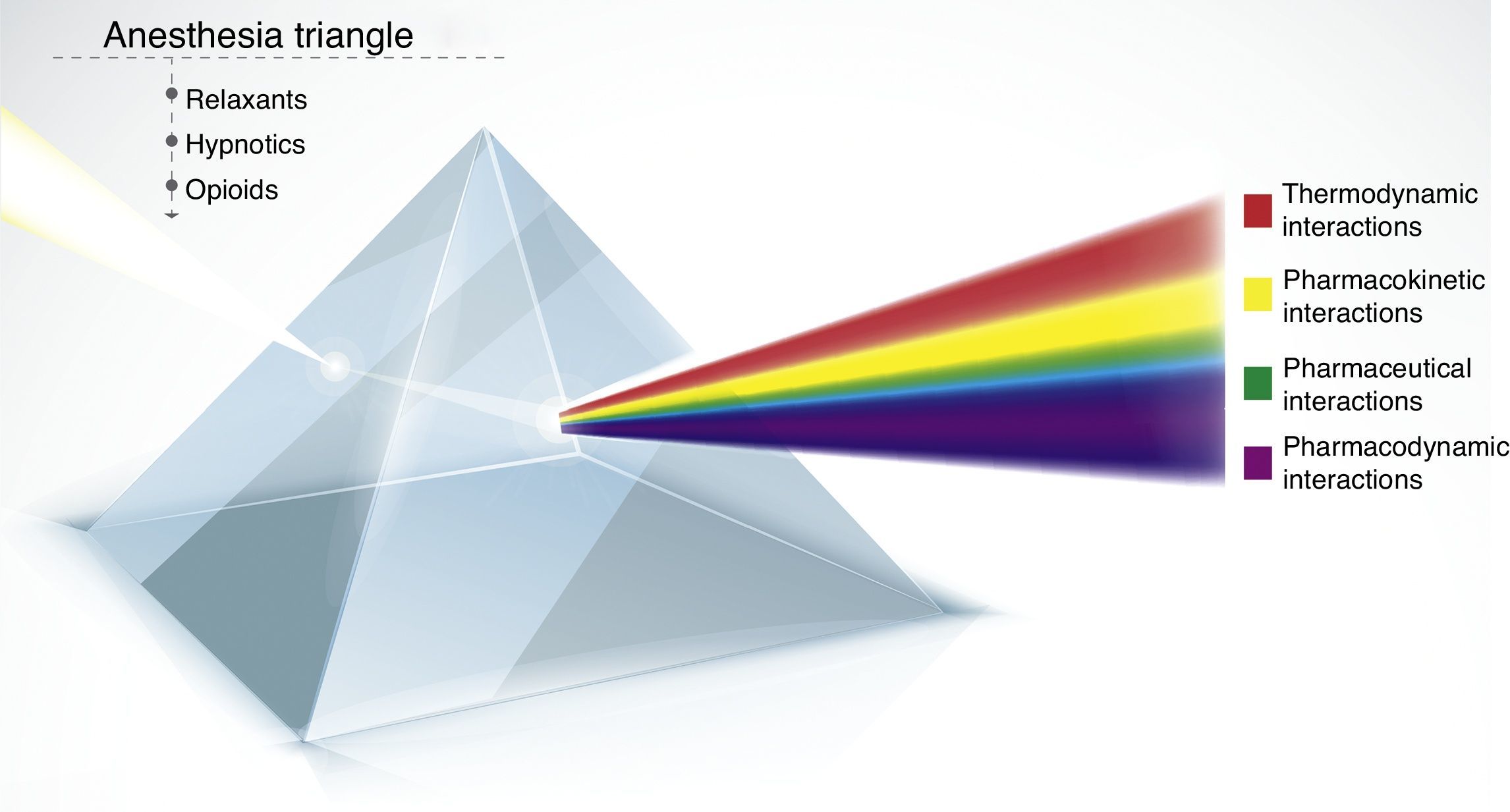
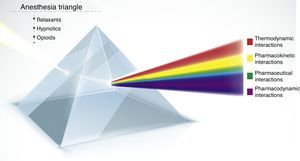
The concept of the anesthesia triangle (AT) goes beyond a triangle representing the key components of anesthesia and according to the initial model was represented by a prism with each side representing one component and the barycenter of the triangle exemplified the interactions among those components.6
The primary interaction submitted among the three components of anesthesia was pharmacodynamics, that entailed recording the ventilation depression associated to the interaction of the opioid, the hypnotic agent and the relaxant.
Five decades later, the AT continues to be valid and the principle of interactions resulting from the triangle has been expanding.
Today we still have the three basic components, but the range of interactions among them has grown beyond pharmacodynamics to include four interactions: pharmaceutical, pharmacokinetics, pharmacodynamics, and thermodynamics.
In sum, we have three components – opioid, hypnotic, and relaxant – that when present in the body may interact in four different ways: pharmaceutical, pharmacokinetics, pharmacodynamics, and thermodynamics.
These interactions are the foundation for the current triad and being clear about what each one involves will enable a safe administration of anesthesia with a multimodal approach that is safer and reproducible (Fig. 1).
Pharmacological interactions of the anesthesia triangle. Represents the concept of the anesthesia triangle – hypnosis, analgesia, relaxation – and their interactions. Any medications entering the prism may result in different interactions: pharmaceutical, pharmacokinetics, pharmacodynamics, and thermodynamics. A larger number of incoming drugs leads to increased complexity and more interactions.
Currently, few drugs are available to build the AT: remifentanil, propofol, rocuronium, inter alia. Getting to know the interactions of this small group of drugs is critical for administering a multimodal safe, target controlled anesthesia – TACAN.7 In addition to these drugs, there are others that while are not part of the AT, are commonly used in the OR (i.e. dexamethasone, midazolam, etc.); hence being familiar with their potential interactions is a guarantee for preventing adverse drug-related events.
Following is a description of drug interactions (DI) associated with physical-chemical incompatibilities that preclude mixing two or more drugs into one solution: pharmacokinetics (PKI), drug interactions involving distribution volume, clearance and metabolism; pharmacodynamics (PDI), additive, over-additive, and under-additive; and thermodynamic (TDI), affinity and intrinsic activity.
Pharmaceutical interactionsPIs are changes in the physical–chemical structure of a drug due to the action of a second drug when combined in the same solution, whether in a bag, a syringe, or in a Y-infusion system.8,9 This type of interactions provide information about drug stability and compatibility. The classical tests to identify stability are chromatography and the main source of information about such interactions is the Handbook on Injectable Drugs.10 Interactions not reported in the book may be looked-up in Internet under the terms: Stability analysis, Mixture, compatibility.
Whenever two or more drugs are mixed for anesthesia purposes or when these agents share the same infusion route, the question about the compatibility of such agents must be asked. Hypnotics are usually combined with opioids or with other hypnotics with no consideration as to their compatibility or potential instability when combining them. Let us consider two examples:
The combination of remifentanil and propofol is usual in some medical institutions.11,12 However, is it appropriate to mix these two agents? The Handbook on Injectable Drugs, gives little information about this topic, but a search using the terms “stability compatibility remifentanil-propofol” takes us to a trial by Stewart that concludes that the stability of the mix combining these two drugs depends on time, the proportion of remifentanil – propofol and the recipient. Hence, according to this trial you may conclude that remifentanil may be mixed with propofol, provided the above variables are considered. However, any compatibility study with propofol shall include an analysis of the stability of the emulsion,13 and this information is not currently available in the remifentanil literature.
The mechanism responsible for pain at the site of injection of propofol is mediated by the kallikrein–kinin pathway and the production of bradykinin, a process that may be inhibited by lidocaine.14,15 But, is it possible to combine propofol and lidocaine to prevent such pain? Are these compounds compatible? Masaki et al., concluded that the addition of lidocaine to propofol increased the diameter of the lipid vesicles making the mix physically and chemically unstable in time, and potentially a risk for pulmonary embolism.16
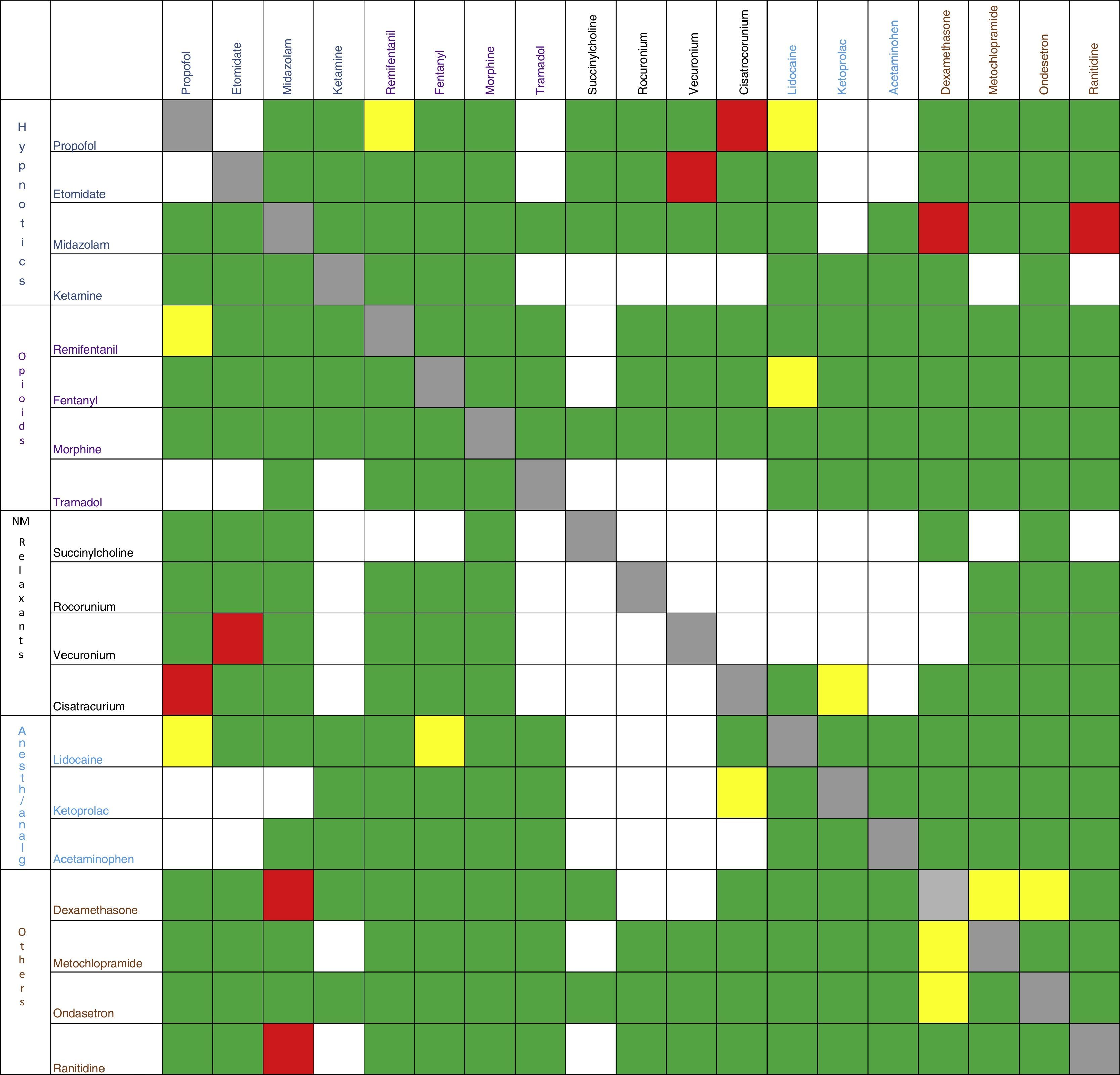
The same exercise shall be repeated whenever different medicines share the same infusion route, whether it is antibiotics, vasoactive drugs, antiemetic agents, etc.17–20Fig. 2 summarizes some of the Pharmaceutical Interactions of the most commonly used drugs in anesthesia.
Pharmacokinetic interactionsThese interactions are rarely taken into account; however, they are responsible for the atypical behavior of certain medicines.21,22
It is usual to find that when infusing remifentanil and propofol, upon the administration of a bolus of propofol it may seem that an extra dose of remifentanil was also administered. How can this phenomenon be explained? Bouillon et al., concluded from a trial to establish the PKIs between propofol and remifentanil that propofol's PK remains unchanged by remifentanil. Secondly, that propofol reduces the central volume of distribution (41%), clearance (41%) and removal (15%) of remifentanil. Thirdly, that the dose requirements of remifentanil to reach plasma concentration decrease with the co-administration of propofol in bolus, but this is not the case when propofol is administered as an infusion.23 This classical IPK study shows that propofol, when changing the remifentanil volume of distribution, the dose of the latter to reach plasma concentrations decreases and this is the factor responsible for adverse events such as bradycardia and extreme hypotension when these drugs are given as bolus.
However, probably the drug that causes more PKI is midazolam, a drug frequently used as a preoperative sedative, with variable behavior and impacting the metabolism of other medications due to the inhibition of cytochrome P4503A4. In terms of fentanyl, Labroo et al.,24 showed that midazolam decreases the production of norfentanyl by almost 95%. With regards to propofol Vuyk,25 documented a disruption of metabolism increasing its blood concentration by around 25%. Such changes in drug metabolism are likely to cause events such as depression, hypotension, and bradycardia.26 These events could probably be prevented if these interactions were taken into account. Other drugs that are frequently used and that affect this enzyme are: dexamethasone, prednisolone, ketamine, antidepressants and alfentanil, inter alia.27
Pharmacodynamic interactionsThe simultaneous administration of anesthetic agents acts on various receptors resulting in different PDIs that may be additive, synergistic, or inhibitory.28,29
Additive interactions present when two or more drugs sharing similar action mechanisms are simultaneously administered and the effect of such combination equals the effect expected from the summation of their effects.30 Additive behavior is typical of hypnotic agents and their simultaneous use only contributes to rise the number of adverse events because each individual action is not being enhanced, but rather replaced. This type of PDI may be seen when administering sevofluorane and propofol simultaneously.31
Synergistic interactions occur when the combination of drugs results in a considerably higher effect as compared to the expected for the addition of the effects.32 This type of interaction is ideal for the practice of anesthesia since the dose required of two medications administered simultaneously is lower as compared to individual separate infusions. In other words, the drug action improves when both medications are present.
Synergistic interactions are used to develop surface models, to establish the NRP to a stimulus, and to guide a controlled target anesthesia. Currently, the most widely used surface models to establish NRP are: the remifentanil – propofol surface model and the sevofluorane – remifentanil model.33,34
The absolute requirement for building a synergistic PDI model is that the drugs involved act on different receptors and that such drugs shall cover the complete hypnosis spectrum in case of hypnotics or complete analgesic spectrum in case of opioids. The risk of using drugs with poorly defined pharmacodynamics profiles to reach the expected target must be emphasized at this point. Let us take dexmedetomidine – an α2 receptor agonist – as an example, a drug with a growing interest in anesthesiology and critical care.35 This drug fails to meet all the properties of a hypnotic agent, nor those of an analgesic; it does not meet the principle of versatility since it is unable to cover the complete spectrum of hypnosis or analgesia. What does that mean then? If you were to build a surface model between dexmedetomidine and propofol or dexmedetomine and remifentanil, reaching high PNRs would not be enough. This is why dexmedetominide in anesthesia is not part of the triangle and its use is limited to that of an adjuvant with sedative properties so that in the event of requiring a profound hypnosis, its poor efficiency requires the addition of another hypnotic agent. The same principle applies for analgesia.
Antagonistic or inhibitory interactions occur when the combination of drugs results in a lower effect than expected for the summation of effects.36
Thermodynamic interactionsThe thermodynamic analysis potentially provides a vision of the molecular events underlying the drug–receptor interactions37–40; in other words, the TIs refer to the processes of affinity and intrinsic activity.
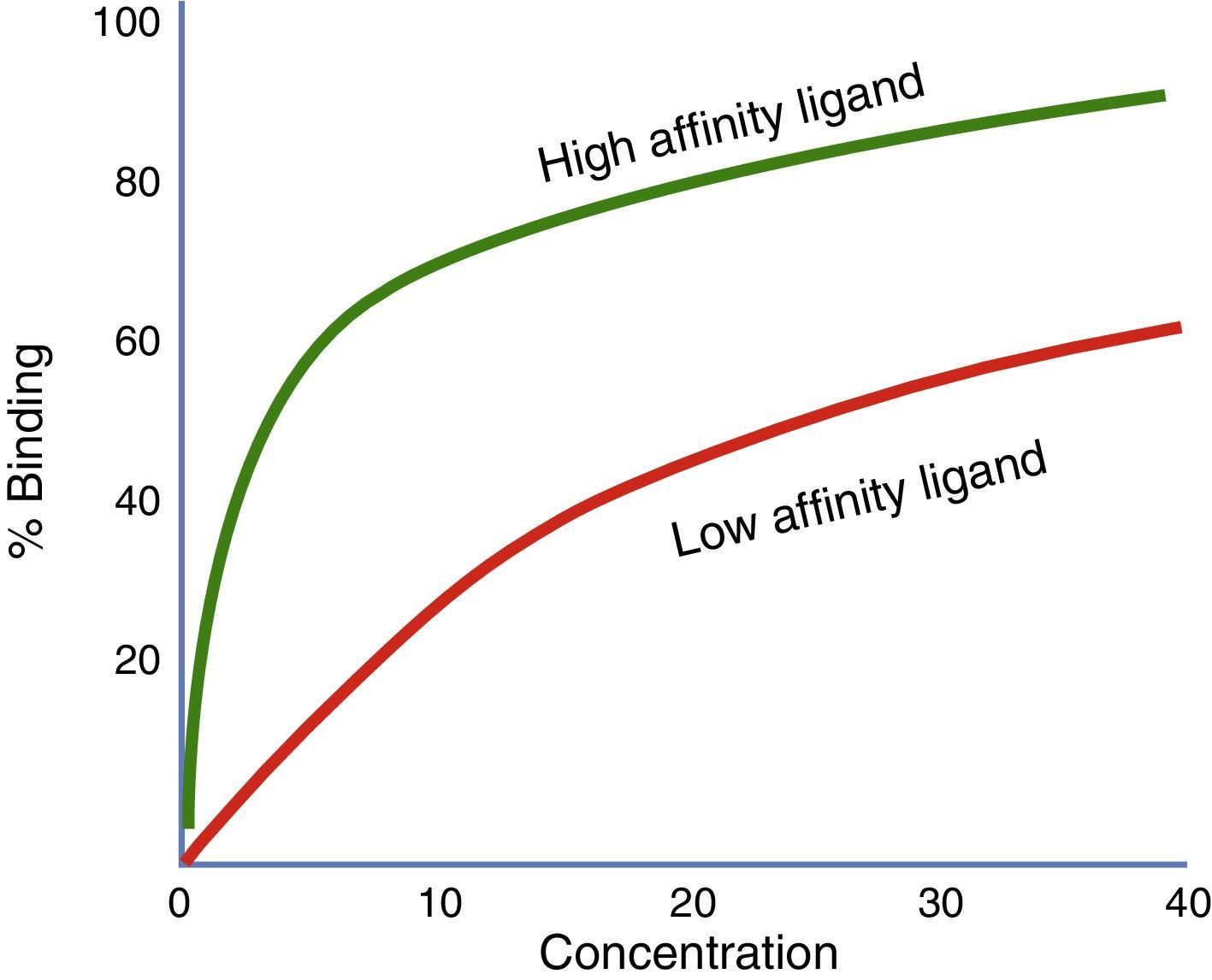
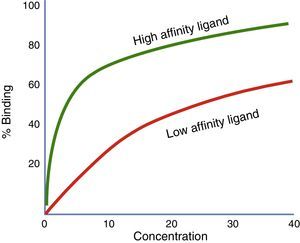
Affinity and intrinsic activityThe strength with which a drug binds to its receptor is called affinity. The level of receptor activation by the drug is called intrinsic activity. The receptor affinity and the receptor activation are two separate traits of a drug.41 A drug may have high affinity for a receptor but failure to activate such receptor (for example, an antagonist).42 When two drugs act on the same receptor and are simultaneously administered, the affinity coefficients (Ki) shall be considered in order to establish which of the two drugs will preferably bind to the receptor, regardless of the intrinsic activity generated (Fig. 3).
Represents the proportion of receptors binding to two different agonists at variable concentrations. In this chart, the strongest affinity agonist (green) and the lowest affinity agonist (red) are compared. The ligand illustrated by the green curve has a higher affinity that the red curve ligand. If both ligands are present at the same time, the highest affinity ligand will bind to the available receptors.
The concept of affinity is probably the most important concept when administering multimodal anesthesia. Fig. 4 illustrates the hypothetical case of a cell with different receptors that may be blocked by different ligands. Based on the multimodal anesthesia concept, the ideal would be to block our target from different points or modes,43 as shown in the figure.
Multimodal anesthesia concept. Left: multimodal anesthesia, different drugs looking for different receptors (remifentanil R, propofol P, and lidocaine L). Right: unimodal anesthesia, several drugs looking for one single receptor (remifentanil, fentanyl, and methadone), the drug binding to the receptor will be the one with the highest affinity.
But what could happen if instead of using three different modes, more than two drugs acting on the same receptor are used (single mode); for instance, using blue chips only to block the cell?
Using several drugs that act on the same receptor is quite removed from the principle of multimodal anesthesia; it would be like using captopril and enalapril for blocking angiotensin or to ADP inhibitors to block the platelet. Therefore, using two drugs that bind to one same receptor involves knowing the affinity coefficients to determine which will preferably bind.
The affinity coefficients are determined through thermodynamic testing, whereby a radiolabeled high affinity agonist is released and the mass of another drug able of displacing 50% of the labeled agonist is measured.44 The concept of affinity is based on the concept of power, where the critical variable is the mass so that the more mass is needed (high Ki) to displace a selective ligand, the lower the affinity of the particular drug.
Studies carried out by Rimmel,45 Schmidtmayer,46 and Clarkson,47 comparing two drugs competing for one single binding site, indicated that under certain conditions the fraction of receptors blocked by the combination of drugs is lower than the fraction of receptors blocked by the higher affinity agent. When the concentrations of both drugs are high, the saturation of the receptors by the higher affinity drug (lower Ki) will prevail.
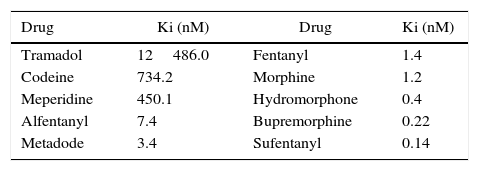
This rule may not be overlooked in the case of opioids administered simultaneously, when their mechanism of analgesia prevails over the same receptor. Table 1 shows the affinity coefficients (Ki) of the various opioids. These coefficients were established using a synthetic opioid with high affinity for the receptor called DAMGO; hence, the less mass an opioid needs to displace 50% of DAMGO, the higher the affinity for the receptor.48
Coefficient of affinity of the various opioids.
| Drug | Ki (nM) | Drug | Ki (nM) |
|---|---|---|---|
| Tramadol | 12486.0 | Fentanyl | 1.4 |
| Codeine | 734.2 | Morphine | 1.2 |
| Meperidine | 450.1 | Hydromorphone | 0.4 |
| Alfentanyl | 7.4 | Bupremorphine | 0.22 |
| Metadode | 3.4 | Sufentanyl | 0.14 |
The less fat the opioid needs to displace an agonist, the more affinity. In the case of analgesia with methadone and morphine, the latter will displace the former. Source: Modified from Volpe et al.49
According to the table, sufentanyl for instance just needs a concentration of 0.14nM as compared to alfentanyl 7.4nM to displace 50% of the labeled agonist; while if both were simultaneously in front of the receptor, sufentanyl will be the opioid binding to the receptor because it requires a smaller mass (greater).49
The affinity of remifentanil vs. morphine for the miu receptors was studied by Poisnel et al. The study documented that morphine is an agonist that fails to discriminate among the three subtypes of opioid receptors, showing values for Ki of 14.9±3.1 to 19.3±3.6nM. The affinity of remifentanil with other miu receptors – which had not been previously characterized, showed a pharmacological profile with a Ki of 21.1±1.2nM, very similar to that of morphine (Ki=17±1nM).50 Based on the data collected documenting the various Ki of the three most commonly used opioids in anesthesia, morphine has the highest affinity for the miu receptors, followed by remifentanil and fentanyl, respectively. Hence, in situations where the concentrations of these drugs are sufficiently high to saturate the miu receptors, the opioid with the highest affinity shall bind to the receptor. When two opioids with intrinsic activity such as fentanyl and remifentanil are simultaneously administered at high concentrations in multimodal anesthesia, you must anticipate that one of them has higher affinity and conceptually that would be an inefficient system. Other opioids like bupremorphine, with high affinity for the μ receptor (low Ki) and a poor intrinsic activity (poor analgesic), is capable of totally displacing morphine, fentanyl, remifentanil, methadone, and other opioid agonists.51 This characteristic makes bupremorphine a suitable treatment for opiate detoxification.52
Another case where the intrinsic activity principle and daily practice affinity are essential is opioid-related depression, and the recommendation is using naloxone, a very high affinity opioid (low Ki), but with poor intrinsic activity.53 Or, when using a neuromuscular relaxant to displace acetylcholine, which has a high receptor affinity but its intrinsic activity is null.
ConclusionDrug interactions are the cornerstone of the anesthesia triangle and being aware of those interactions may contribute to safe anesthesia.
FundingThe author did not receive sponsorship to carry out this article.
Conflicts of interestThe author has no conflicts of interest to declare.
I would like to acknowledge Drs. Diego Rincón and Vladimir Rivas from Universidad Surcolombiana, Neiva, Colombia.
Please cite this article as: Tafur-Betancourt L. El mundo oculto de las interacciones farmacológicas en anestesia. Rev Colomb Anestesiol. 2017;45:216–223.