Most of the complications related to sedation are preventable. This document defines some recommendations for non-anesthesiologists so that they can provide sedation level I and II with adequate safety. The most important recommendations are: that the sedation be provided by someone different from the person who performs the surgical procedure; designation of the training and monitoring of thje person who sedates; the use of only one medication for sedation, and the availability of medications and equipment to manage complications; the mandatory need of an assessment prior to the sedation, as well as informed consent and record of events during the procedure; and the recommendation of having a low threshold to request the support of an anesthesiologist.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier. All rights reserved.
Las complicaciones relacionadas con la sedación son, en su enorme mayoría, prevenibles. El presente documento establece unas recomendaciones para que los no anestesiólogos puedan realizar sedaciones nivel I y II con un buen nivel de seguridad. Sus aspectos más importantes son: administración de la sedación por una persona diferente del operador; recomendaciones en cuanto a la capacitación, la monitorización, el uso de un solo medicamento para la sedación y la disponibilidad de medicamentos y equipos de respaldo; la necesidad de realizar una evaluación previa a la sedación, así como el consentimiento informado y el registro durante el procedimiento; y recomendaciones para considerar un bajo umbral con el fin de solicitar el apoyo de un anestesiólogo.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier. Todos los derechos resevados.
The safety committee of the Sociedad Colombiana de Anestesiología y Reanimación (SCARE) jointly with several scientific societies of Colombia decided to offer healthcare providers (1) this guide intended to provide the best safety possible for patients during sedation. There is very little regulation in this area in most countries and it is necessary to correct this situation.1
The recommendations described have as a goal, the reduction of preventable morbidity, and it is expected that the compliance to them will help avoid preventable morbidity and mortality, which unfortunately periodically occur in the country.
The literature consistently describes that adverse events during sedation are mostly preventable, which is the reason that compliance with these safety recommendations is critical to avoid adverse outcomes.2–4
With the information in this report it becomes clear that stablishing recommendations for safety during sedation outside an operating room are critical to prevent major morbidity or death.
MethodsThis consensus was developed as a response to a request, at the beginning of the year 2010, by theHealth Authorities in Bogota, Colombia. They requested recommendations for sedation by non-anesthesiologists from the Sociedad Cundinamarquesa de Anestesiología (SCA). The SCA designated a group of anesthesiologists dedicated to sedation administration to develop the first document in May 2010, which was published in a blog of the Sociedad Colombiana de Anestesiología y Reanimación (SCARE) in July 2010 for discussion. Because of the importance of this initiative, SCARE transferred the process to its safety committee with the participation of members of the committee as well as other anesthesiologists dedicated to sedation who participated in the initial document. They, jointly wrote a draft in November 2010 based on the literature available and on guidelines and recommendations, that overall had a low level of evidence, but anyway have been adopted and implemented in other countries.
Once this document was completed, it was presented to the senior members of SCARE who suggested some changes that were made to the draft, and thereafter several public discussions were held at the Secretaria Distrital del Salud de Bogotá (SSD) (2), at the Congreso Colombiano Anestesiología(3) and in virtual) meetings using the Delphi method.5 Multiple modifications of the original draft were made until a final consensus was reached on July 21, 2011 with the approval and signature of six scientific societies and the Secretaria Distrital de Salud of Bogotá, Colombia.
Thereafter, several meetings were held to discuss the incorporation of the document into the update of the mandatory requirements for government approval for health services, Decree 1043 (4) It was then presented at the Plenum de Presidentes of SCARE (5), as well as at an academic meeting of the Sociedad de Anestesiología y Reanimación del Atlántico(6). The recommendations for sedation for patients under 12 years old were simultaneously developed.(7)
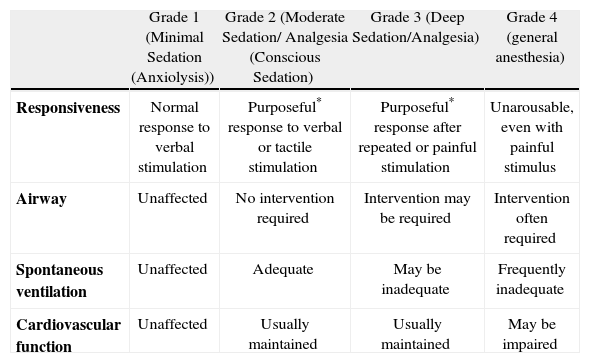
Definitions of sedation and analgesiaThe table 1 describes how the American Society of Anesthesiologists defines the level of sedation:6
Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia
| Grade 1 (Minimal Sedation (Anxiolysis)) | Grade 2 (Moderate Sedation/ Analgesia (Conscious Sedation) | Grade 3 (Deep Sedation/Analgesia) | Grade 4 (general anesthesia) | |
| Responsiveness | Normal response to verbal stimulation | Purposeful* response to verbal or tactile stimulation | Purposeful* response after repeated or painful stimulation | Unarousable, even with painful stimulus |
| Airway | Unaffected | No intervention required | Intervention may be required | Intervention often required |
| Spontaneous ventilation | Unaffected | Adequate | May be inadequate | Frequently inadequate |
| Cardiovascular function | Unaffected | Usually maintained | Usually maintained | May be impaired |
Taken from: Practice guidelines for sedation and analgesia by non-anesthesiologists.
This classification is very useful to clearly define the competencies necessary to provide safe sedation. It is critical to understand, however, that these levels are part of a continuum, and the progression from one level to another can easily occur in brief periods of time. These recommendations take into account this circumstance and unpredictable reality that demand, to some extent, that caution in excess of some level is necessary, because if some safety considerations are appropriate for one level, they may not be for the next level to which the patient may progress due to physiological and pharmacodynamic variability. Therefore the assessment of the level of sedation should permanently be assessed by reviewing the verbal capability in every patient.
Level I : AnxiolysisIt describes a scenario which allows the patient to tolerate an uncomfortable procedure, while maintaining adequate cardiopulmonary function and the capability of responding to a verbal or tactile stimulus. At this level, the sedation is minimal and has the least impact on patient safety. This is the level that has the least requirements for patient safety.
Level II: conscious sedationLevel II is moderate sedation, and can be achieved with the use of one medication. In this level of sedation, as seen in the previous table, the airway is rarely compromised, therefore expert competence in airway management is not essential, and basic airway competences suffice. With basic airway management training, it is possible to correct the airway issues that may arise.
Level III: deep sedationIf a response is only obtained with a painful stimulus, it is considered that the patient is under deep sedation. At this level of sedation, protective reflexes are obtunded, there is no capability of maintaining airway, and there is a possibility of hemodynamic compromise.
This level is usually achieved by combining medications (opioids in addition to a sedative), and therefore demand expert airway management skills, as the airway can be significantly compromised, and the lack of expert management can be associated with a lethal outcome in a short period of time. In Colombia, airway management expertise is almost exclusively achieved during training in the specialty of anesthesiology, and to a much lesser degree in critical care or emergency medicine.7
For these reasons, the physicians or dentists that require this level of sedation, like radiology, gastroenterology and dentistry, rarely attain these competencies during their training. Therefore, when the loss, or obstruction of the airway, or respiratory depression occur, these can lead to a serious adverse outcome, which is almost always preventable, either by avoiding this level of sedation or by obtaining support from anesthesiologists.
The ad hoc Sedation Committee of the SCARE considers that this level of sedation should be restricted to anesthesiologists, as the safety recommendations necessary for this level are rarely met in most of the country.
With these considerations, only an anesthesiologist, the expert in deep sedation (level III), or exceptionally individuals with the competences described below, should provide level III sedation (deep sedation).
Level IV: general anesthesiaLevel IV, general anesthesia, is of exclusive practice by an anesthesiologist according to the Colombian law. After the enactment of Law 6a of 1991, this Law has been related to a dramatic decrease in anesthesia related malpractice suits, which suggests that when anesthesia is provided by a trained physician in anesthesiology, there is a profound impact on patient safety.8
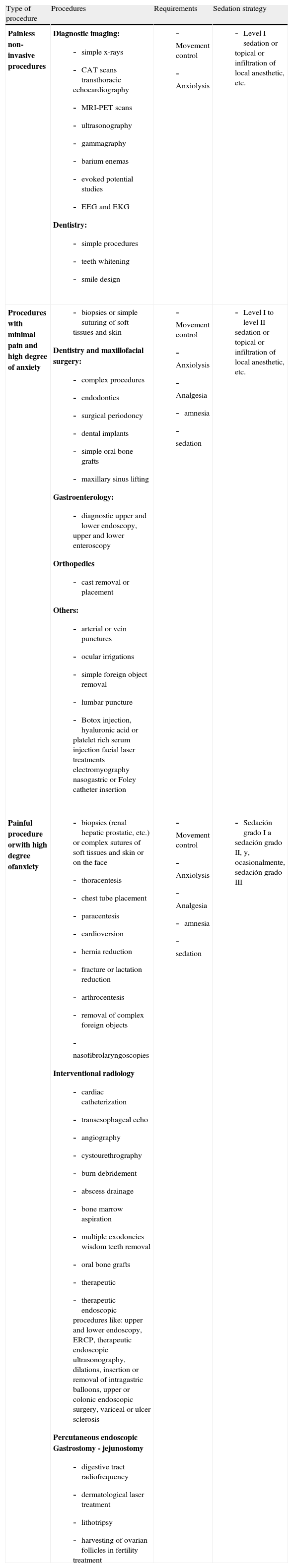
Procedures that could require sedation (table 2)Who should administer the sedation?These recommendations indicate that the sedation should always be performed by a physician, dentist, a certified registered nurse or nurse assistant, under the supervision of trhe person who practices the procedure, and foremost should be a person different from the one performing the procedure. This person should have these minimal competences:
- 1)
Monitor the vital signs of the patient, heart rate, blood pressure and pulse oximetry
- 2)
Should be certified in basic life support if performing sedation level I or II. It should be periodically updated according to the prevailing standards.
- 3)
Should have basic training in sedation obtained from approved courses endorsed by the scientific society of the area (dentistry, gastroenterology, radiology, etc.) and jointly by SCARE.
- 4)
The sedation certification should include training in managing crises and complications.
- 5)
The certification is valid for only four years and should be periodically renewed.
Table of procedures that could require sedation in adults
| Type of procedure | Procedures | Requirements | Sedation strategy |
| Painless non-invasive procedures | Diagnostic imaging:
|
|
|
| Procedures with minimal pain and high degree of anxiety |
|
|
|
| Painful procedure orwith high degree ofanxiety |
|
|
|
The SCARE checklist for sedation should always be verified (Web appendix 1: http://www.revcolanest.com.co (appendixes)). Its verification should be recorded in the patient's chart.12,13
Patient assessmentThe completion of the patient's chart, including a full physical examination and relevant tests, is critical to avoid complications. Special attention should be made to airway assessment and verification of a proper fasting (minimal six hours for solid and non-clear fluids, and two hours for clear fluids). All this information should be recorded in the chart.
Procedure preparationWritten and informed consent: the patients and their relatives or responsible person should be informed of the benefits, risks and limitations of the procedure, and the person responsible for sedation should also explain the possible existing alternatives and post-procedural indications.
Death should be also considered as a possible complication of the procedure or sedation13 . After this the patient or the responsible person should sign to complete the consent. Postprocedural indications should always be provided. It should be known that if whoever administers the sedation is not a physician or dentist, the person directly responsible for the adverse or morbid events of the sedation is the physician or dentist who practices the procedure requiring sedation.
MonitoringConsciousness level: verbal responses are the guide for the level of consciousness. They also help to confirm that the patient is breathing. Monitoring the verbal response of the patient should be routine, except in patients were unable to respond properly (for example patients with mental handicap or non-collaborating patients), or during procedures in which patient movement could affect the results. All patients under sedation or analgesia should be constantly monitored (at least with a pulse oximeter with its alarms properly functioning) and the blood pressure should be measured intermittently.
Monitored parameters recordIn the clinical chart there should be a record of the hemodynamic and respiratory variables at regular intervals before, during and after the procedure. The adverse events should also be recorded in the chart (Web appendix 2: http://www.revcolanest.com.co (appendixes)).
Necessary personnelA physician, dentist; a certified registered nurse or nurse assistant under the responsibility of who practices the procedure and different from the person who practices the procedure, should be responsible for monitoring and assisting the patient. If whoever performs the sedation is not a physician or dentist, the professional who performs the procedure has full medicolegal responsibility of the personnel performing the pre-procedural assessment or sedation.
Personnel trainingThe person responsible for the monitoring and assistance of the patient should have training that allows him/her to:
- -
Be knowledgeable in the pharmacology of the medications used, their adverse effects and possible complications.
- -
Have competency in airway management.
- -
Be able to provide basic life support (sedation level I and II).
- -
Have current certification in basic life support and in a course in sedation training with the curriculum that SCARE, along with the scientific society of the area (gastroenterology, radiology, endoscopy, dentistry, etc.), consider appropriate.
- -
There should always be a defined strategy to manage situations when complications arise during the sedation. The complications during sedation are almost always preventable, as long as there is compliance with these recommendations.
El sitio donde se realiza la sedación debe tener estas características:
The site where sedation is practiced should have these characteristics:
- 1)
Enough space should be available for CPR.
- 2)
There should be appropriate lighting.
- 3)
A table or chair that allows horizontal positioning should be available.
- 4)
An oxygen source, as well as face masks or cannula for spontaneous breathing ,should be available.
- 5)
There should be a resuscitation bag (AmbuH type) with reservoir.
- 6)
A pulse oximeter with or without plethysmographic curve should be available.
- a.
The alarms must never be switched off.
- a.
- 7)
Advance resuscitation medications should be available:
- a.
Epinephrine or adrenaline
- b.
Atropine
- c.
Amiodarone or Lidocaine without epinephrine
- d.
Intravenous fluids
- e.
Flumazenil (can be omitted if benzodiazepines are not used)
- f.
Naloxone (can be omitted if opioids are not used)
- g.
Portable supply of oxygen should be available
- h.
Bronchodilator inhalers like salbutamol or ipratropium should be available
- i.
Hydrocortisone
- a.
- 8)
There should be a manual or automatic blood pressure measurement device.
- 9)
There should be oral or nasopharyngeal cannulas, laryngeal mask airways are highly desirable (ideal) or laryngoscope and orotracheal tubes.
- 10)
There should be a defibrillator (not required with nitrous oxide sedations).
- 11)
There should be an explicit strategy to request assistance in case of emergency.
- 12)
There should be compliance with current government regulatory standards.
The combinations of sedatives and opioids can increase the likelihood of complications, including respiratory depression, hypoxemia, and cardiac arrest. Midazolam and propofol as single medications have demonstrated their safety15 when used by non-anesthesiologists, when this personnel has periodic certified training, and has the indicated monitoring equipment available.
Sedation level IThe recommended medications are: midazolam, nitrous oxide or propofol.16
Sedation level IIMidazolam or propofol are recommended. It is again indicated that its safe use can only be achieved when there is a periodical certification of the personnel; otherwise their practice can be associated with serious outcomes, including death, which can be prevented. In countries, such as the United States, some health authorities have restricted the use of propofol by nonanesthesiologists if an individual without anesthesia training administers it.17
As propofol can produce general anesthesia, it can only be used by non-anesthesiologists when there is periodical certification of training in its use, and deep sedation and general anesthesia is avoided. Otherwise its use can lead to serious adverse outcomes, mostly preventable.17–22
In fact, even when used by anesthesiologists problems can be associated with serious adverse outcomes.4
Sedation level IIIDeep sedation (level III: when the patient only responds to painful or repeated stimuli) can only be performed in the following requirements are met:23
- 1)
Individual with current ACLS certification (this certificate is valid for two years).
- 2)
Training in EKG monitoring.
- 3)
Training in advance airway management.
- 4)
Certified current advanced sedation course at least every four years.
- 5)
Capability of electrocardiograph interpretation.
- 6)
Monitoring equipment that includes: SpO2, NIBP, EKG, and some procedures EtCO2 (as indicated in the sedation guidelines of the United States).
- 7)
Supervised experience when beginning to perform sedations.
If these requirements are not met, this level of sedation cannot be performed as the risk of preventable complications is very high.
Venous accessThere should always be a patent venous access when performing intravenous sedation and it should be maintained until there is no risk of cardiopulmonary depression. In case of sedation with nitrous oxide, these can be omitted whenever the patient has no relevant medical problems.
RecoveryAfter the administration of the sedation or analgesia, the patient should be monitored by a certified registered nurse or nurse assistant until when there is no risk of cardiopulmonary depression or hemodynamic abnormalities. There should be permanent pulse oximetry, with the alarms functioning, until the patient is discharged. This should be when the patient recovers to baseline conditions. Post-procedural indications should be provided. Every patient must be accompanied when discharged.
Special situationsCertain types of patients (for example non-collaborating patients, patients of advanced age or the very young, severe cardiac or pulmonary, hepatic diseases, or CNS abnormalities, or with morbid obesity, sleep apnea, pregnant patients or patients with alcohol or drug abuse) have a high risk of developing complications related with sedation or analgesia, and so special considerations need to be made.
In these types of patients, sedation should be provided by anesthesiologists to minimize the risk of preventable morbidity. The anesthesiologist should decide if additional prior interventions should be performed to assess their risks and to determine their management.
Likewise, the complexity of the procedure could require more complex or lengthy sedations that could require the assistance of an anesthesiologist.
UpdatesThese recommendations are dynamic and should be reviewed periodically.
The present document was developed during public presentations from October 2010 until July 2011. It has been endorsed by the Executive Board of SCARE, and was presented in an open forum about this consensus of sedation by non-anesthesiologists held during the XXIX Congreso Colombiano de Anestesiología, on March 22, 2011.
This document has been endorsed by: Asociación Colombiana de Gastroenterología; la Asociación Colombiana de Endoscopia Digestiva; the Colegio Colombiano de Odontólogos; the Asociación Colombiana de Radiología; the Asociación Colombiana de Cirugía Oral y Maxilofacial; the Federación Odontológica Colombiana; and the Academia Colombiana de Odontología Pediátrica. All these organizations gave their seal of approval during its final presentation on July 21, 2011 at the Secretaría Distrital de Salud del Distrito Capital in Bogotá.
Competing InterestsThe authors Alberto Molano, Sandra Rubiano, and Fernando Vieira / Ana María Orozco are either directors or anesthesiologists of the sedation enterprises Sedarte Ltda., Sedación Ambulatoria SAS, and Meseda, respectively.
Funding sources: Colombian Society of Anesthesiology and Resuscitation SCARE