Fluid mismanagement in liposuction leads to pulmonary edema in a previously healthy individual. Pulmonary edema is considered the third cause of death in plastic surgery after PTE and lidocaine toxicity. The most important risk factor leading to this outcome is inadequate knowledge of fluid management and poor communication between the surgeon and the anaesthetist.
ObjectivesTo review the causes leading up to pulmonary edema in liposuction and the valid options for correct fluid management.
MethodsNon-systematic review of the literature in PubMed and Medline.
Results and conclusionsCorrect fluid management in liposuction is based on a close communication between the surgeon and the anaesthetist in order to keep track of the total amount of subcutaneous fluid infiltration plus fluids delivered intravenously, always bearing in mind that infiltration fluids go to the central circulation.
El mal manejo de líquidos en liposucción, conlleva a edema pulmonar en un paciente previamente sano. El edema pulmonar se considera la tercera causa de muerte en cirugía plástica después del TEP y la Intoxicación por lidocaína. El principal factor de riesgo que conlleva a este desenlace es el desconocimiento en el manejo de líquidos y la mala comunicación entre el cirujano y el anestesiólogo.
ObjetivosRevisar las causas que llevan a edema pulmonar en liposucción y las opciones validas de manejo correcto de líquidos.
MétodosSe realizó una revisión de la literatura no sistemática en las bases de datos PubMed y Medline.
Resultados y conclusionesEl correcto manejo de líquidos en liposucción se basa en una estrecha comunicación entre el cirujano y el anestesiólogo para sumar los líquidos infiltrados a nivel subcutáneo y los colocados por vía venosa, siempre teniendo en cuenta que los líquidos de la infiltración pasan a la circulación central.
Liposuction is the most common cosmetic surgery procedure performed in the United States1 and also in Colombia. Advances in the techniques for infiltration, designed to allow placement of epinephrine in a solution, thus reducing bleeding during lipoaspiration, have enabled removal in large volumes during liposuction. This induces significant changes in fluid behaviour inside the compartment, with the risk of pulmonary oedema and heart failure.2
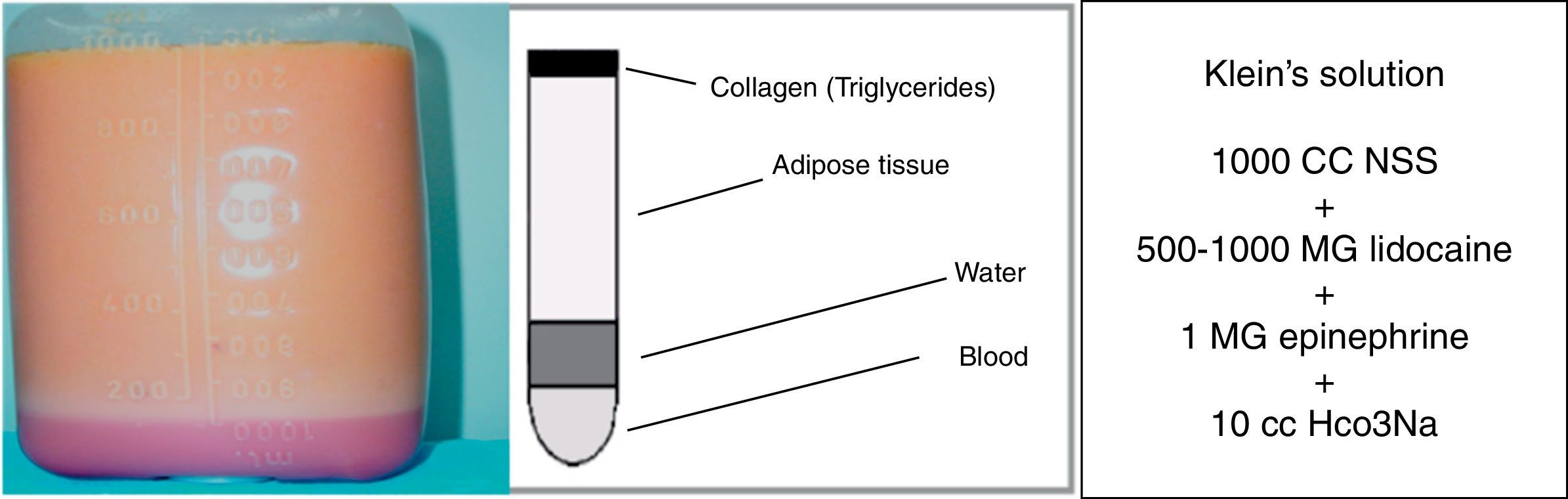
Added to the invention by Klein in 1987 of a tumescent solution that included 500–1000mg of lidocaine plus 1mg of epinephrine for every 1000cc of NSS3 (Fig. 1) and which is widely used today for subcutaneous infiltration, the risk of lidocaine toxicity is a reality and the second cause of death in plastic surgery according to the American Society of Plastic Surgeons (ASPS).
The biggest problem with these new infiltration techniques, in particular the super wet and the tumescent techniques is associated with the large infiltration volumes, at infiltration/aspiration ratios ranging from 1:1 in the super wet technique up to 2–3:1 in the tumescent technique.4 This means that in a 3-litre liposuction, subcutaneous fluid infiltration may amount to 3–9 litres, and this fluid volume requires special consideration from the point of view of anaesthesia.
MethodsNon-systematic review of the literature using the PubMed and Medline databases, introducing key words in English like Fluid Management, Liposuction, pulmonary oedema, larger infiltration, Aspiration volumes. All the articles were read and other articles of the selected references regarding the topic were also queried. Overall, 151 references were selected using this methodology.
ReviewThe use of large infiltration volumes in the tumescent solutions increases the difficulty of anaesthetic management in liposuction significantly. The risk of hypervolemia, pulmonary oedema, epinephrine-related cardiovascular effects, and lidocaine toxicity is always present.5
The purpose of using infiltration solutions with 1mg of epinephrine in 1000cc of Hartman's or NSS is to reduce bleeding into the lipoaspirate down to less than 5% of the extracted volume.6 This results in the ability to perform large-volume liposuction, with the ensuing complications. Some studies conducted by Burk and Vasconez7 have shown the use of up to 10mg of epinephrine at concentrations of 1:1,000,000 in healthy patients, with no deleterious effects from toxicity such as tachycardia and hypertension, although these megadoses may lead to fatal consequences in patients with underlying cardiac disease in whom no workup has been done.
The second problem, when Klein solutions are used, is the infiltration of high doses of lidocaine (500–1000mg of 1% lidocaine for every 1000cc of NSS). There are multiple studies in the world literature conducted in plastic surgery patients that show that very high doses of lidocaine (up to 35–55mg/kg) could be safe8,9 considering that the infiltration is applied to scarcely vascularized adipose tissue and, moreover, considering the additional vasoconstriction derived from the use of epinephrine in the dilution. These studies have shown a margin of safety in thousands of liposuction procedures performed, with no risk of toxic levels despite the high doses of infiltrated lidocaine.
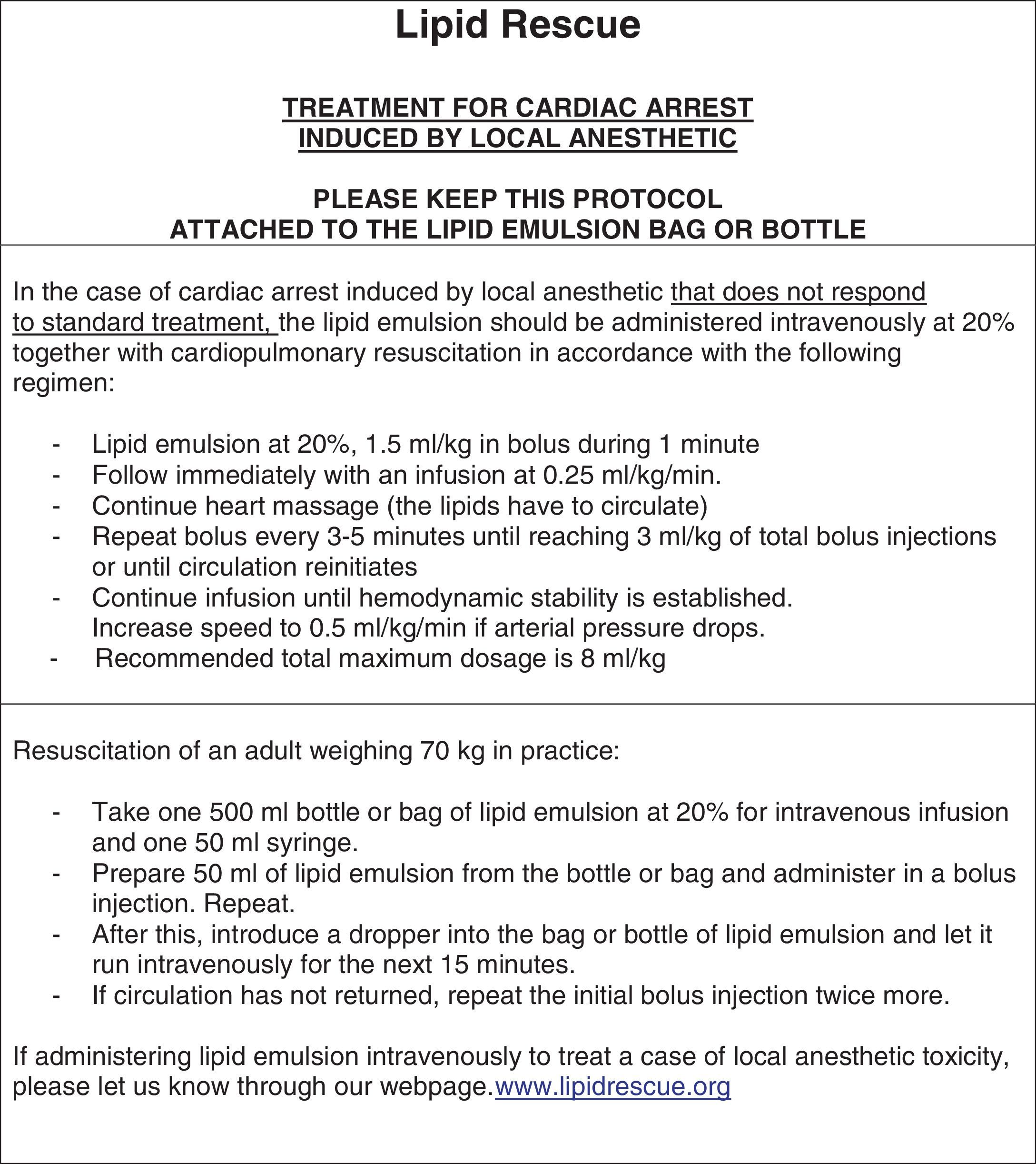
As far as anaesthesia is concerned, the FDA only accepts maximum doses of 7–10mg/kg. The ASPS has reported that lidocaine toxicity may be an important cause of death in plastic surgery and might account for some intra- and post-operative deaths resulting from cardiac arrest in conditions of normal oxygen saturation. However, this is very difficult to demonstrate because of the difficulty in measuring post-mortem serum levels, something that is usually done late or not done at all. It is worth noting that the use of high lidocaine doses has enabled dermatologists and surgeons to perform liposuction in their offices using local anaesthesia without the support of an anaesthetist, with the sole purpose of lowering the costs associated with the use of the operating room and the support of the anaesthetist. For this reason, our recommendation, when large quantities of lidocaine are used for infiltration, is that an anaesthetist must be present in the room and must be prepared to manage lidocaine toxicity-related cardiac arrest. Additionally, 20% lipids must be available in the room as the only effective measure to revert cardiac arrest while waiting for resuscitation. Fig. 2, shows the protocol for the management of local anaesthetic toxicity-related cardiac arrest, endorsed by the American Society of Regional Anaesthesia and the American Society of Plastic Surgeons, and published in www.lipidrescue.org together with the supporting literature.
The third issue relates to the large volumes of infiltrated fluids and volume overloading: in a 4-litre liposuction, subcutaneous fluid infiltration may be as high as 12 litres.
In 1998, the University of Texas Southwestern Medical Centre defined that a large-volume liposuction is the removal of more than 4000cc of fat, while a small-volume liposuction corresponds to the removal of less than 4000cc. The same study determined that the volume of fluids delivered is equal to the volume of infiltration fluids given by the plastic surgeon plus the volume of intravenous fluids given by the anaesthetist. When added together and then divided by the liposuction volume, the ratio should not be greater than 2 for liposuctions under 4L (or 8 litres of fluids administered when intravenous and infiltration fluids are added together, in a 4-litre liposuction), or greater than 1.4 for liposuctions of more than 4 litres. In this study of 53 patients there were no cases of complications or fluid overload, and diuresis was maintained at a level higher than 1cc/k/h. In a later study by Rohrich in 89 patients,10 it was shown, in essence, that the use of this same formula for liposuction does not result in complications.
In plastic surgery, pulmonary oedema is the third cause of death, resulting mainly from human error associated with the lack of knowledge of the basic physiological principles of infiltration, the lack of protocols, and poor communication between the surgeon and the anaesthetist. In a study conducted in The Netherlands in 50% of the hospitals between 1995 and 1997, it was found that 2–4% of all anaesthesia-related deaths were due to poor fluid management and pulmonary oedema, and medical error was demonstrated in 85% of these fatal cases.11
The main physiological consideration is that most of the infiltrated fluids go into the general circulation and only 22–29% is recovered with lipoaspiration.12,13 This means that up to 70% of infiltration fluids, lidocaine and epinephrine go into the intravascular space. Later studies have shown that 1 litre of subcutaneous infiltration is fully resorbed if not removed within 163min, and that 70% of the lidocaine and epinephrine is totally resorbed, with maximum peaks at 12 and 5h.4
In a study of 5 healthy ASA 1 women14 undergoing large-volume liposuction, a Swan-Ganz catheter was used for 24-h monitoring in the ICU, with continuous measurement of the haemodynamic parameters in order to assess the effects of the infiltration and the high adrenaline doses. It was determined that cardiac index, heart rate and mean pulmonary artery pressure increased by more than 45%, while central venous pressure increased from 4 to 14cm H2O 8h into the postoperative period.14 Moreover, the same study showed that all patients were hypothermic during surgery with recorded temperatures under 35.5°C.
High doses of epinephrine are used routinely in liposuction, with all the haemodynamic implications. Epinephrine reaches maximum concentration levels 3–5h after subcutaneous administration. After infiltrating 7mg of adrenaline, serum levels reach 323pg/ml, very similar to the levels found in aortic clamping or coronary bypass,15,7 which are 3 or 4 times as high as baseline levels. In fact, there are anecdotal reports on epinephrine-related complications in patients with previously undiagnosed coronary heart disease; this is due to the low rate of its systemic absorption in fat and to its vasoconstriction effect, and the potential protective anti-arrhythmic effect of lidocaine.7
The presence of lidocaine in the infiltration may lead to serious and even fatal complications. Neurological symptoms appear when levels are above 5¿g/cc, and there is cardiovascular collapse with levels higher than 10¿g/cc.16 Apparently, many studies have shown a certain margin of safety with subcutaneous lidocaine infiltration, even in doses as high as 55mg/kg, due to the low vascularity of fat and the vasoconstrictor effect of adrenaline.17–19 The problem is that its release from fat is also slow, and it has been shown that maximum levels are reached within 8–12h after the infiltration20 when the patient is already at home, creating an additional risk. It is also important to take into consideration differential absorption rates, given that when the face is infiltrated, maximum concentrations are reached after 5h, but when the abdomen and the thighs are infiltrated, they peak at 12h, and at some point there may be a summation effect.18 Lidocaine metabolism may worsen the situation in cases of toxicity. Lidocaine is cleared mainly through liver metabolism (95%) while only 5% is cleared through the urine.21 It is deacetylated to monoethyliglycinexylidine (MEGX) which is then deacetylated to glycinexylidine (GX). The two enzymes responsible for this action are CYP3A4 and CYP1A2 which belong to the cytochrome P450 family of isoenzymes.21,22 These isoenzymes may be inhibited by various commonly used drugs, including ciprofloxacin, cimetidine, erythromycin, amiodarone, ketoconazole, fluconazole and even propofol;21,22 or the metabolism may be altered by drugs that compete for the same enzyme, as is the case of midazolam and fentanyl, which are also metabolized by CYP3A4.21,22 This is very important because these drugs not only may alter the metabolism but also may mask the initial signs of intoxication, leading to serious neurological or cardiovascular symptoms. Although these subcutaneous megadoses of 35–50mg/kg of lidocaine may seem suboptimal, intraoperative deaths have been reported due to heart block in conditions of normal oxygen saturation. In those cases, the autopsy does not find any abnormality,23 and lidocaine levels may appear normal; however post-mortem stability of lidocaine has not been demonstrated so far. In a census carried out among all the members of the American Society of Plastic Surgeons in 2000, mortality from liposuction was shown to be 1 out of every 5000 procedures. The primary cause of death was PTE, but it was also found that most deaths occurred on the first postoperative night, so lidocaine toxicity and residual anaesthetic effects are not ruled out as an important cause of mortality.
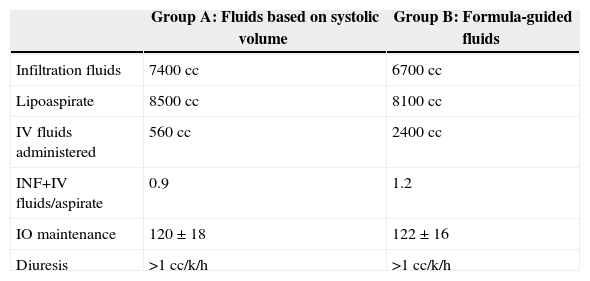
Although PTE is the main cause of death, there are stringent, well developed protocols for prophylaxis that may lower the incidence of DVT and PTE by 85%, and of fatal PTE by 95%. The problem with fluid management in liposuction is that with the new super wet and tumescent infiltration techniques, fluid overload is a potential risk and there is no consensus regarding its management to this date. There are only a few empirical division formulae for fluid delivery versus infiltration fluids to guide the management of fluid therapy.24–26 Using these formulae, fluid delivery in a liposuction under 4 litres must follow a ratio of 2 between infiltrated plus intravenous fluids divided by the aspirate, and a ratio of 1.4 in a liposuction of more than 4 litres.24–26 Despite these formulae, fluid overload continues to be a problem, and there are reports of deaths in liposuction when they are applied. Intravenous fluids are being used less in liposuction, and although the standard is not to use the tumescent technique (3:1) but the super wet technique (1:1), this has contributed to a lowering of fluid delivery down to a ratio of 1.2 between fluids delivered (intravenous plus infiltration) and fat removed, according to Rohrich.24 Recently, a study was conducted with 30 patients undergoing large volume liposuctions of more than 6 litres in which half of the patients received fluids according to Rohrich, i.e. a 1.2 ratio (for a 6-litre liposuction they could receive only a maximum of 7200cc of infiltrated plus intravenous fluids) and the other half of the patients received fluids on the basis of systolic volume variation using the arterial line thermodilution technique (LIDCO).27 This study showed that, in large-volume liposuction where infiltration was greater than 1:1, intravenous fluids were used only for maintenance −500 to 600cc over the 5h of surgery – and an excellent stroke volume was achieved, with diuresis remaining always above 1.2cc/k/h.27–29 Studies show that intravenous fluid quantities must be as low as possible when super wet techniques are used30,31 (Table 1), and there are some that have even proposed abolishing intravenous fluids.32 In conclusion, when liposuction is performed as a single procedure, conservative management of intravenous fluids is required, considering that infiltration fluids go into the central circulation. Consequently, the recommendation is to use only maintenance fluids.
Comparison between formula-guided and systolic volume-guided intravenous fluid administration using the LIDCO method in large-volume liposuction.
| Group A: Fluids based on systolic volume | Group B: Formula-guided fluids | |
|---|---|---|
| Infiltration fluids | 7400cc | 6700cc |
| Lipoaspirate | 8500cc | 8100cc |
| IV fluids administered | 560cc | 2400cc |
| INF+IV fluids/aspirate | 0.9 | 1.2 |
| IO maintenance | 120±18 | 122±16 |
| Diuresis | >1cc/k/h | >1cc/k/h |
As stated above, fluid management also involves managing infiltration, lidocaine and epinephrine levels, and hypothermia.33 Together, these factors are responsible for numerous reports of deaths due to myocardial infarction, pulmonary oedema and lidocaine toxicity.33–43.
Although it is not within the scope of this paper, it needs to be mentioned that the subcutaneous infusion of these large volumes of infiltration fluids at ambient temperature means that temperature in all patients remains under 36°C. Consequently, we are required to take the necessary steps to avoid hypothermia, considering that it may lead to problems such as bleeding, AMI and seromas.44–47
ConclusionsCorrect fluid and infiltration management, together with the steps for preventing DVT and PTE, is the most important measure to reduce complications and deaths in plastic surgery. Regarding fluid management in liposuction, when super wet or tumescent techniques are used, the worldwide recommendation is to use a minimum amount of intravenous fluids, that is, only maintenance fluids, because the infiltrated volume is sufficient (1.2 maximum ratio between fluid delivery and fat removal).
As for the dose of epinephrine in the infiltration, it should not be higher than 6mg or 1kg/kg, as long as the patient does not have an underlying cardiovascular disease.
As for lidocaine, although the FDA recommends a maximum of 7–10mg/kg, there are multiple studies showing that higher doses (35mg/kg) are relatively safe. Consequently, in cases of infiltration with large volumes of lidocaine, our recommendation is that the procedure must be performed under the constant supervision of an anaesthetist who must be prepared to manage lidocaine toxicity-related cardiac arrest. Moreover, 20% lipids must be available in the room as the sole effective measure to revert cardiac arrest while waiting for resuscitation.
FinancingNo.
Conflicts of interestThe author is coordinator of the Committee on Anesthesia for Plastic Surgery, Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.).
Please cite this article as: Marin JEB. Manejo de líquidos, lidocaína y epinefrina en liposucción. La forma correcta. Rev Colomb Anestesiol. 2015;43:95–100.