Trigeminal neuralgia (TN) affects primarily women over 50 years of age and its etiology is unknown in most cases. Drugs are first line treatment, but they are ineffective in 40% of cases. Interventional therapies are a management option in those cases.
ObjectiveTo determine the safety and efficacy of Gasserian ganglion thermal (TR) radio frequency in patients with TN.
Materials and methodsDescriptive, prospective follow-up study of a cohort of 15 patients with a diagnosis of TN who underwent Gasserian ganglion TR at the Colombian Pain Institute between May 2010 and May 2011, with at least one year follow-up.
ResultsThe mean age of the patients intervened was 52 years, 73% were females with right-sided predominance (67%) with involvement mainly of the second and third branch of the trigeminal nerve. After the intervention, all 15 patients went from severe pain to a condition ranging between mild and no pain, and 50% were even pain-free one year after the procedure.
ConclusionsTN has a significant effect on quality of life. The main treatment is pharmacological but when it fails, Gasserian ganglion TR is an effective and safe option available in our setting.
La neuralgia del trigémino (NT) afecta principalmente a mujeres mayores de 50 años y es de causa desconocida en la mayoría de pacientes. Los fármacos son la primera línea de tratamiento, aunque son inefectivos en el 40% de los casos; las terapias intervencionistas son entonces una alternativa de manejo.
ObjetivoDeterminar la eficacia y la seguridad de la radiofrecuencia térmica (RT) en el ganglio de Gasser en pacientes con NT.
Materiales y métodoSe realizó un estudio de tipo descriptivo, prospectivo, de seguimiento a una cohorte de 15 pacientes con diagnóstico de NT, en quienes se realizó RT del ganglio de Gasser en el Instituto Colombiano del Dolor entre los meses de mayo de 2010 y mayo de 2011, con un seguimiento no inferior a un año.
ResultadosLa edad promedio de los pacientes intervenidos fue de 52 años. El 73% fueron mujeres, con predominio derecho (67%), y las principales ramas trigeminales comprometidas fueron la segunda y la tercera. Después de la intervención los 15 pacientes pasaron de dolor severo a un estado entre nada de dolor y dolor leve, e incluso el 40% se encontraron libres de dolor al año del procedimiento.
ConclusionesLa NT afecta de forma importante la calidad de vida. Su principal tratamiento es farmacológico, pero cuando no es efectivo, la RT del ganglio de Gasser es una alternativa eficaz, segura y disponible en nuestro medio.
TN is a disorder that affects primarily women over 50 years of age, with an incidence of 4–5 in every 100,000 inhabitants.1 Its cause is unknown in most patients and it is characterized by sudden episodes of intense, unilateral pain, usually on the right side, affecting mainly the second and third branches of the trigeminal nerve.2 Diagnosis is basically clinical and imaging studies can only identify a clear cause in 15% of cases, usually in the form of vascular nerve compression.3,4
Pharmacological treatment is effective only in 60% of patients, and interventional management must be considered for the remaining cases. Gasserian ganglion TR is a relatively non-invasive and effective option.5
Materials and methodsBetween May 2010 and May 2011, 15 patients with a diagnosis of TN refractory to pharmacological treatment were selected at the Colombian Pain Institute (Medellín, Colombia) for rhizotomy, with a follow-up of at least one year.
Inclusion criteriaClinical findings for TN; contrast nuclear magnetic resonance imaging emphasizing the Vth cranial nerve that ruled out a vascular loop in its course; failed drug therapy; a history of a positive diagnostic block of the Gasserian ganglion; absence of concomitant disease or chronic medication as contraindications for the procedure; and written consent from the patient.
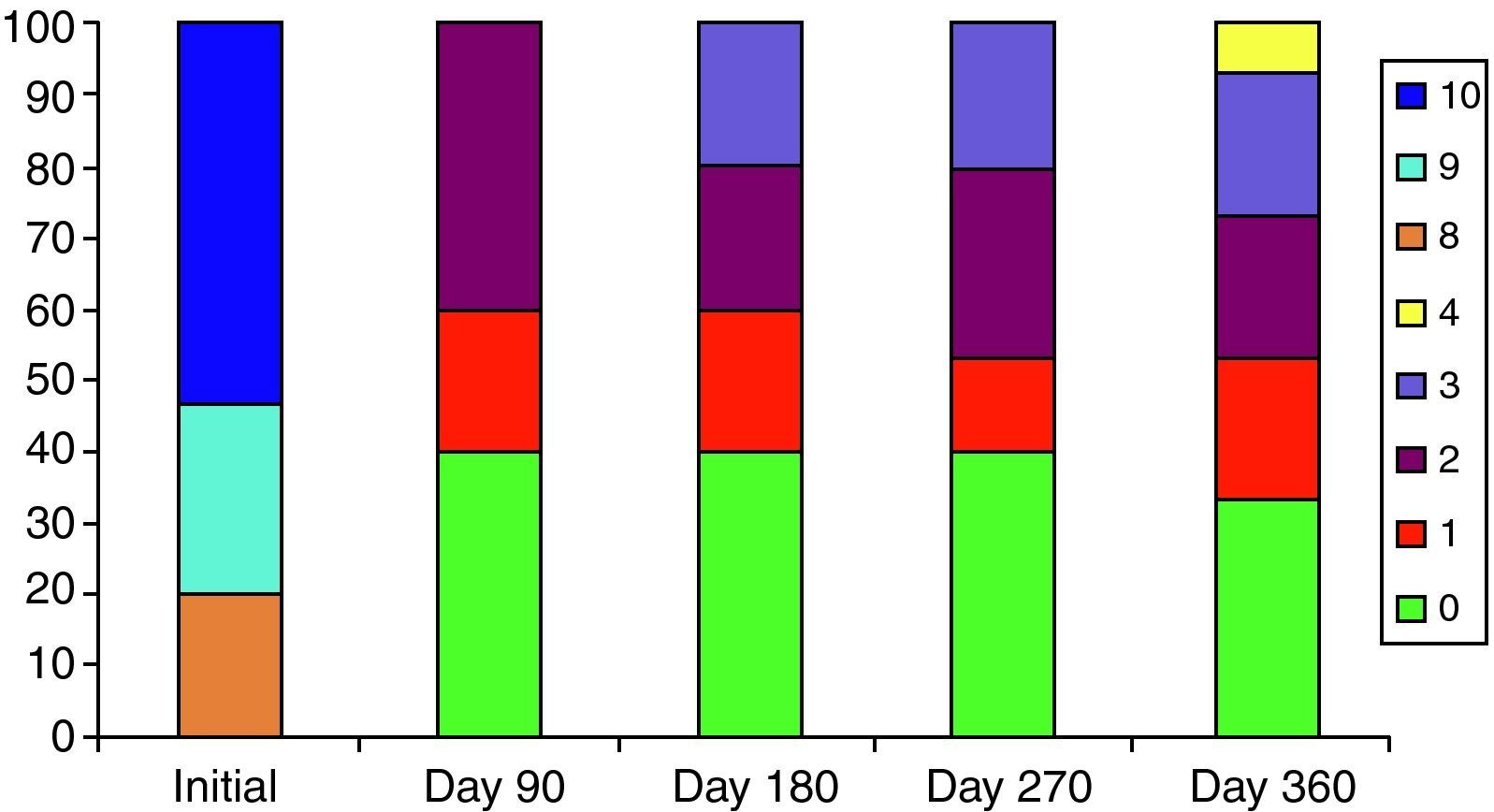
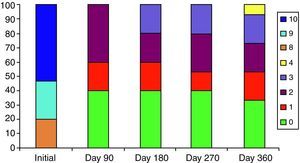
Pain intensity was assessed using the visual analogue scale (VAS) with a score from 0 to 10, and classified as 0=absence of pain, 1–4=mild pain, 5–7=moderate pain 8–10=severe pain, at 90, 180, 270 and 360 days after the procedure.
Technique description- •
Anesthesia: Conscious sedation with midazolam and fentanyl was initiated under basic monitoring. The patient was given 40–50mg of propofol once the cannula was placed on the target, before the thermal lesion. The patient was awakened after the first lesion to assess the result and, if required, a repeat dose of propofol was given for additional TR time.
- •
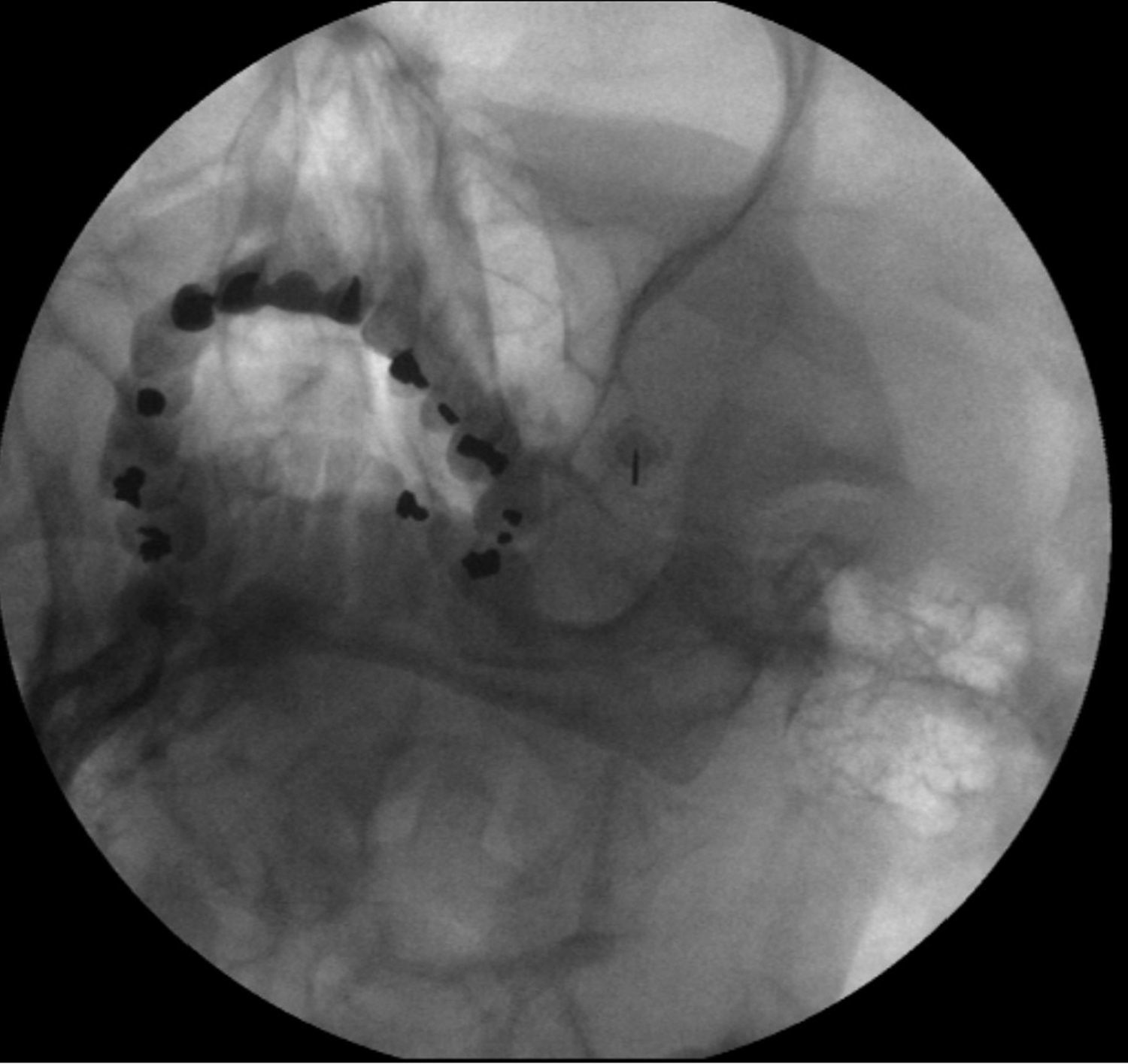
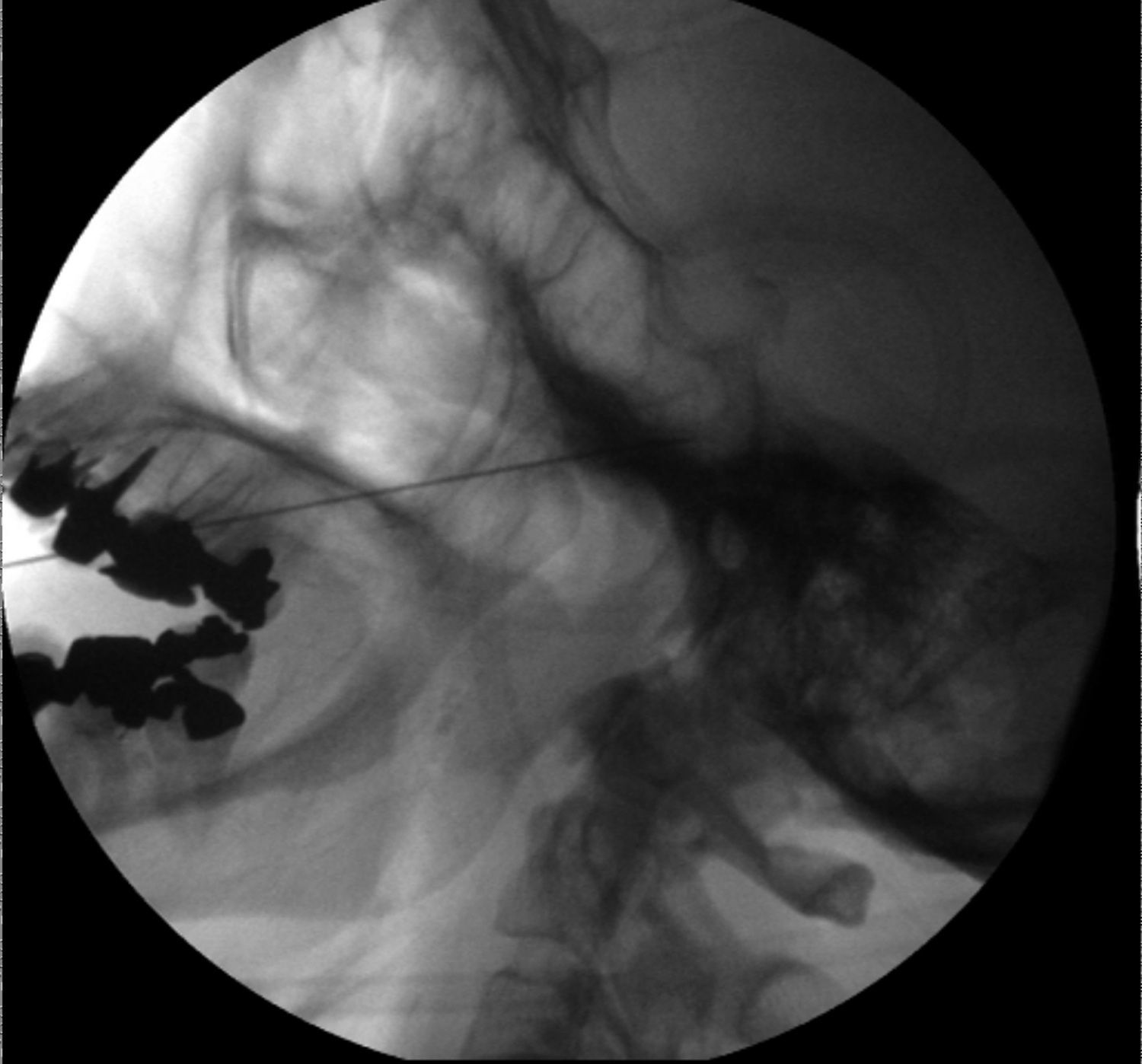
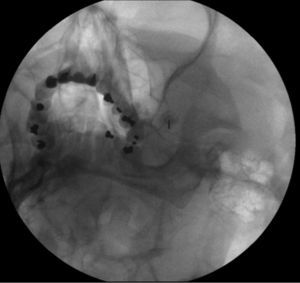
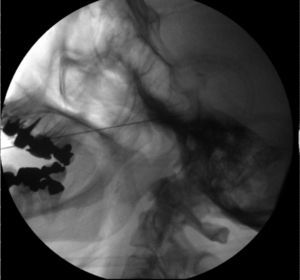
Surgery: The patient is positioned in supine decubitus with the image intensifier at 0° laterally and 30°–45° of caudal inclination (submental view). Patient head is in extension, rotated approximately 30° opposite to the painful side; with the mouth open, the foramen ovale is identified medially to the mandibular ramus. The insertion point is 3cm lateral to the lip commissure, following an imaginary line to the pupil with the target at a 3cm depth anterior to the external auditory meatus (Fig. 1). A 22-gauge, 10cm-long radiofrequency cannula with an active tip is introduced under tunnel vision directed towards the medial portion of the foramen ovale. The foramen is entered (Fig. 2), with the entry point identified because of a change in tissue resistance. The lateral view is then used to determine depth and ensure that the tip of the cannula does not exceed a distance of 2mm from the plane of the clivus (Fig. 3). The stimulation process is initiated with the tip inside the foramen in order to determine which branch is involved, using a Cosman G4 radiofrequency equipment; for stimulation to be considered adequate, thresholds must be lower than 0.4 volts. Once the target branch is identified, deep sedation is administered in order to perform the lesion with an initial test at 40° for 30s in order to test for tolerance. The final lesion is performed at 80° for 90s. The patient is awakened in order to assess the result and determine the need for a repeat procedure. Two lesions – maximum three – were performed based on the response and the branches involved (Fig. 4).
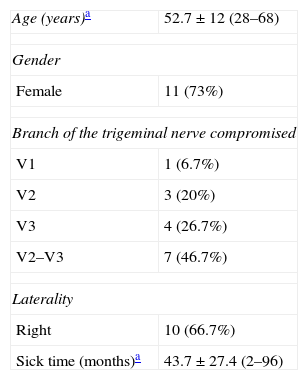
As observed in Table 1, mean age was 54±12 years, with a range from 28 to 68.
The average time of symptoms at the time of the intervention was 43±27.4 months, with a range between 2 months and 96 months.
Of the total number of patients, 73% were women, with right-sided predominance (66.7%). In terms of the trigeminal branch involved, only one patient had V1 involvement (6.7%), V2 was involved in 3 patients (20%), V3 in four patients (26.7%) and 7 patients had concurrent involvement of V2 and V3 (46.7%).
All of the patients started out with severe pain. After 90 days, 40% of patients were pain free and the remaining 60% had mild pain. This proportion was maintained at 180, 270 and 360 days. Fig. 5 shows that pain levels after the intervention remained low during the one-year follow-up.
Two patients had complications, the first (6.6%) a transient masseter weakness on the side of the lesion, which had resolved completely one month after the intervention, and the second (6.6%) an ipsilateral transient hyperesthesia that resolved within three weeks. All cases were treated as outpatients, and no patient required a second TR session during the follow-up period.
DiscussionTN is a disorder that has a significant deleterious effect on quality of life. The first line of treatment is pharmacological with carbamazepine as the drug of choice with an NNT (number needed to treat) of 1.7, followed by oxcarbazepine and other anti-convulsants such as lamotrigine, pregabalin and gabapentin, but these are effective only in 60% of patients, with their effectiveness dropping substantially in the long term. When drug therapy fails or gives rise to significant adverse effects, interventional treatment must be considered. It has been shown that the earlier the intervention is performed, the better the long-term prognosis.6
Interventional techniques may be applied peripherally (distal to the Gasserian ganglion), directly on it, or distal to it,7 and the lesion may be ablative (nerve destruction) or non-ablative (nerve function sparing).8
Peripheral techniques include the administration of streptomycin,9 lidocaine,10 alcohol and phenol, cryotherapy, acupuncture or surgical section over distal nerve portions. However, most of these therapies have not been effective11 and one-year recurrence is greater than 50%.12
A vascular loop compressing the nerve may be found in 15% of patients with TN and, in such cases, the most effective therapeutic approach is microvascular decompression.13
Procedures on the Gasserian ganglion include chemical lesion with glycerol, balloon mechanical compression and TR.
Glycerol rhizolysis involves injecting this substance in Meckel's fossa to create a lesion on the Gasserian ganglion. Its effectiveness at 2 years is 60–90%, but it has been abandoned because of potential complications and little ability to control the lesion.14–16
In balloon compression of the Gasserian ganglion, a small balloon is introduced percutaneously into Meckel's fossa, exerting direct compression on the ganglion in 80–90% of cases, with varying recurrence rates in the different studies.17,18
Stereotactic radiosurgery consists of applying a high dose of ionizing radiation on the Gasserian ganglion or on the root of the trigeminal nerve in the posterior fossa, using different systems such as the Gamma Knife, the CyberKnife or the LINAC (linear accelerator). Pain relief with these techniques is not immediate, requiring from 2 to 6 weeks. The effectiveness of this treatment varies significantly among the different studies, ranging from 10 to 61% over a time period between a few months and 3 years, and the recurrence rate is also variable, ranging from 6 to 54%. Moreover, this is a high-cost intervention, which is why it is not considered as a first-line option.19,20
Thermal radiofrequency (TR) consists of using heat to destroy nociceptive A-delta and C fibers, sparing the A-alpha and beta fibers responsible for tactile sensation, considering that lower temperatures are needed to create a lesion in the former.21 The largest study in the literature assessing the effectiveness of this procedure was conducted by Kanpolat et al. with a total of 1600 patients. They found that pain improved immediately in 97.6% of whom 52.3% remained pain free at 10 years, and 41% at 20 years. In this study, the pain recurrence rate was 25.1%, and the most frequent complications included reduced corneal reflex (5.7%), masseter weakness or paralysis (4.1%), dysesthesias (1%), painful anesthesia (0.8%), keratitis (0.6%) and transient palsy of the 3rd and 6th cranial nerves (0.8%).22 Other studies show similar results, as is the case with those by Broggi et al. with 1000 patients23 and Tew and Taha with 1200 patients.24
Pulsed radiofrequency is a non-ablative method, unlike RT, although the method is similar but requires longer pauses between each thermal application, and lower temperatures. Although it is believed that there is no thermal lesion, recent evidence suggests that there may be a microscopic nerve injury.25 A recent study comparing the two radiofrequency techniques suggests that the pulsed technique is not as effective as conventional radiofrequency for the management of TN.26
In this study, the clinical characteristics of the patients were very similar to those described in the literature, with the majority being women over 50 years of age mainly with V2 and V3 involvement and right side predominance. Pain relief with the intervention was immediate and persisted in time, similar to what has been reported in other studies. The complications have also been reported in other studies and did not result in permanent sequelae.
ConclusionsTN is a disease with significant deleterious effects on quality of life. Interventional procedures are being used at present with good results. In our experience, radiofrequency thermal ablation of the Gasserian ganglion is an effective technique with a low complication rate, available in our setting. Moreover, it is the only technique that can be used selectively for managing the nerve branch involved.
FundingFunding of this review came from personal resources. Advice was provided by CES University and Epidemiology Ángela María Builes Aguilar.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rivera Díaz R, et al. Radiofrecuencia térmica del ganglio de Gasser en pacientes con neuralgia del trigémino. Rev Colomb Anestesiol. 2013;41:127–31.