A considerable amount of literature has been dedicated to the topic of difficult airway management and a number of algorithms and recommendations have been established to safely manage patients at risk for difficult intubation. Only recently, however, has extubation of the difficult airway gained more awareness since this procedure, although elective, is often fraught with complications. The importance of developing pre-planned strategies for extubation of the difficult airway to improve patient safety and outcomes is apparent from data from both the ASA Closed Claims Analysis and the UK's recent Fourth National Audit Project of major complications of airway management. The key to successful management of patients at risk for difficult extubation is accurate risk assessment, application of appropriate strategies, and preparedness by both the individual practitioner and the institution.
Existe un volumen importante de literatura dedicada al tema del manejo de la vía aérea difícil, y se han desarrollado una serie de algoritmos y recomendaciones para el manejo seguro de pacientes en riesgo de una intubación difícil. Sin embargo, solo recientemente se ha despertado una mayor conciencia acerca de la extubación de la vía aérea difícil, pues aun cuando sea un procedimiento programado, suele estar plagado de complicaciones. La importancia de desarrollar estrategias pre-programadas para la extubación de la vía aérea difícil a fin de aumentar la seguridad del paciente y sus desenlaces se hace evidente a partir de los datos del ASA Closed Claims Analysis y del reciente Cuarto Proyecto Nacional de Auditoría del Reino Unido sobre complicaciones mayores en el manejo de la vía aérea. La clave para un manejo exitoso de los pacientes en riesgo de extubación difícil es efectuar una evaluación precisa de riesgo, aplicar estrategias apropiadas y la preparación tanto del médico como de la institución.
Over the last 20 years, much of the attention on difficult airway management has been focused on intubation. The development of Practice Guidelines for Management of the Difficult Airway and the Difficult Airway Algorithm by the American Society of Anesthesiologists (ASA) Difficult Airway Task Force in 1993 has led to improved outcomes associated with airway-related complications at induction.1,2 Successful management of the difficult airway, however, does not end with placement of an endotracheal tube (ETT). Analysis of the ASA Closed Claims database has shown that the trend of improved outcomes at induction and intubation has not been seen at extubation.2 Airway management complications are not confined to the US. As was made evident in the recent 4th National Audit Project report of the Royal College of Anesthetists in the United Kingdom, safe extubation is by no means guaranteed.3,4 This report demonstrated that one third of major complications of airway management occurred at extubation or in the recovery room with a mortality rate of 5%. The most common problem was airway obstruction, with causes including laryngospasm and airway edema.3 Poor anticipation of an at-risk extubation and poor planning for management after intubation were found to be common contributing factors.3–5 Data such as this has led to increased recognition for the need to develop strategies for the safe and successful extubation of patients with a difficult airway.
In 2012, the Difficult Airway Society (DAS) published the first comprehensive guidelines for management of tracheal extubation in adult perioperative practice.6 While not explicitly focused on extubation of the difficult airway, the guidelines included recommendations and strategies for “at-risk” extubations. In all versions of the ASA Practice Guidelines for Management of the Difficult Airway, including the most recent revision in 2013, formulation of an extubation strategy for the difficult airway is recommended.1,7,8 This strategy should include a consideration of clinical factors which may adversely affect ventilation post-extubation, and an airway management plan that can be implemented if extubation fails.7
Extubation failure refers to the inability to tolerate removal of an ETT due to airway obstruction after intubation.5,9 Possible mechanisms for this include laryngospasm, laryngeal edema, tracheomalacia, and upper airway collapse due to edema, hematoma, or residual anesthetic effects.5 This should be differentiated from a failure to wean from ventilatory support.10 Patients who fail to meet extubation criteria during spontaneous breathing trials should not be extubated regardless of the presence of a difficult airway.11 On the other hand, usual weaning indices are poorly predictive of extubation failure because they do not assess airway patency.12
The difficult airway poses multiple challenges at extubation. Many conditions associated with difficult mask ventilation and/or intubation may also predispose to a higher risk for failed extubation.5,13,14 Reintubation then poses a greater challenge in the difficult airway. Because of the potential for serious morbidity related to failed extubation if reintubation is not quickly achieved, anesthesia practitioners must: (1) be armed with techniques that successfully address the specific challenges in extubation of the difficult airway, and (2) appreciate the potential complications associated with extubation. Determining which patients are at risk for extubation failure and a discussion of the strategies that can be used to aid in reintubation of the difficult airway is the focus of this review.
MethodsThis article is a non-systematic review of the literature regarding extubation of the difficult airway. Targeted literature searches were carried out using databases (PubMed and Medline) and a search engine (Google Scholar). Expert opinion in the form of textbooks and editorials were included.
Recognizing the difficult airway at extubationThe first challenge when formulating an extubation plan is to determine whether one is dealing with a difficult airway or not. A difficult airway, as defined in the ASA Practice Guidelines, is “the clinical situation in which a conventionally trained anesthesiologist experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both”.7 Clearly, if difficulty with mask ventilation or endotracheal intubation was encountered at induction, particular caution should be exercised at the time of extubation due to the expected difficulty of reintubation, if needed. Often, a higher rate of failed extubation is seen in this scenario due to airway trauma as a result of multiple attempts at securing the airway at induction. Airway edema and swelling from the multiple attempts can lead to obstruction after extubation and an inability to adequately ventilate.
On the other hand, there may have been no difficulty with the initial airway management, but because of changes to the airway that have occurred during or after surgery, difficulty may be encountered at extubation. It is important to remember that simply because an airway was easy to manage at the start of an anesthetic, does not mean that airway management will be easy after completion of surgery. Thyroidectomy, carotid endarterectomy, anterior cervical spine procedures, and maxillofacial surgery are only a few examples of surgical procedures performed around the airway that can lead to a difficult airway at extubation.15–18 Many extubation problems associated with these surgical procedures involve postoperative bleeding, nerve damage, or direct tissue trauma. The anesthesia practitioner should also be careful of devices placed near the airway intra- and post-operatively, (e.g., cervical collars, maxillomandibular fixation, or large dressings on the head or neck). These devices may restrict airway access and lead to difficulty with reintubation.19
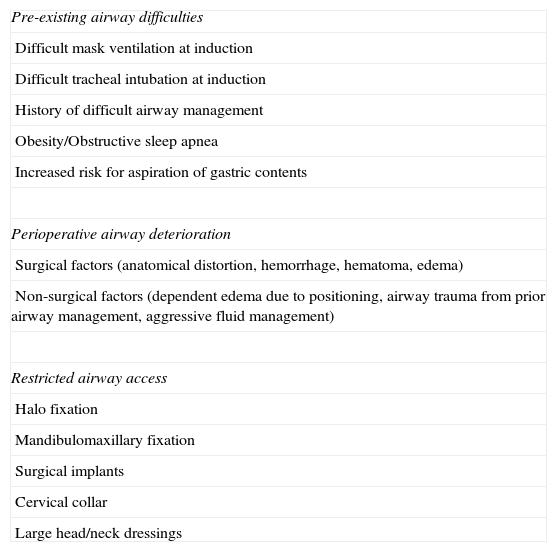
Airway risk factors for extubation failure are summarized in the DAS guidelines (Table 1). The presence of pre-existing airway difficulties (including obesity/OSA and elevated risk for aspiration of gastric contents), perioperative airway deterioration (anatomical distortion, edema, or hemorrhage due to surgical or non-surgical factors), and/or restricted airway access lead to an “at-risk” extubation algorithm that aims to minimize the risk of extubation failure and provide a strategy for reintubation, if necessary.6
Airway risk factors from the difficult airway society guidelines for management of tracheal extubation.
| Pre-existing airway difficulties |
| Difficult mask ventilation at induction |
| Difficult tracheal intubation at induction |
| History of difficult airway management |
| Obesity/Obstructive sleep apnea |
| Increased risk for aspiration of gastric contents |
| Perioperative airway deterioration |
| Surgical factors (anatomical distortion, hemorrhage, hematoma, edema) |
| Non-surgical factors (dependent edema due to positioning, airway trauma from prior airway management, aggressive fluid management) |
| Restricted airway access |
| Halo fixation |
| Mandibulomaxillary fixation |
| Surgical implants |
| Cervical collar |
| Large head/neck dressings |
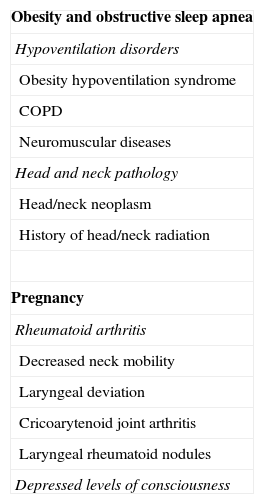
Certain co-existing medical conditions may also cause problems at the time of extubation, including rheumatoid arthritis, obstructive sleep apnea (OSA), hypoventilation disorders, neuromuscular conditions, and depressed levels of consciousness (Table 2).5,20–24 General risk factors, such as impaired respiratory or cardiovascular function, neuromuscular impairment, hypo- or hyperthermia, and metabolic derangements can also complicate extubation.6
Medical conditions associated with increased risk for extubation failure.
| Obesity and obstructive sleep apnea |
| Hypoventilation disorders |
| Obesity hypoventilation syndrome |
| COPD |
| Neuromuscular diseases |
| Head and neck pathology |
| Head/neck neoplasm |
| History of head/neck radiation |
| Pregnancy |
| Rheumatoid arthritis |
| Decreased neck mobility |
| Laryngeal deviation |
| Cricoarytenoid joint arthritis |
| Laryngeal rheumatoid nodules |
| Depressed levels of consciousness |
Deciding to extubate a patient with a known or suspected difficult airway can be problematic. The main goal of extubating the difficult airway, as any airway, is to avoid reintubation, if at all possible. This goal is extremely important when faced with a difficult airway because reintubation is almost always more hazardous. At the time of reintubation, one may be faced with emergent situations such as poor oxygenation and/or ventilation, an uncooperative patient, a compromised airway, and inadequate expert help if reintubation takes place outside of the operating room.25 If not properly addressed, the above factors combined with a difficult airway may lead to a less than desirable outcome.
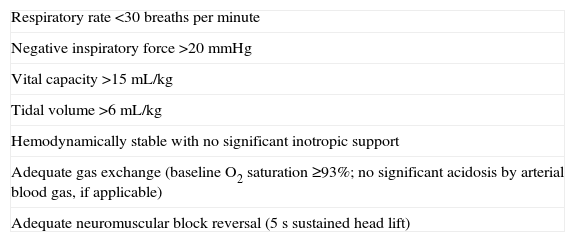
Prior to extubation, the usual criteria should be met, including hemodynamic stability, satisfactory oxygen carrying capacity, normothermia, adequate respiratory rate and tidal volume, good oxygen saturation, and a conscious, alert patient who is able to clear secretions, protect the airway, and maintain airway patency (Table 3).26,27 Patients at high risk for failed extubation are those with any potential for hypoventilation, ventilation/perfusion mismatch, failure of pulmonary toilet, or airway obstruction. One should also take into consideration the patient's future operative schedule – it makes no sense to extubate a patient with a difficult airway and later find out that the patient will be returning the next morning for follow-up surgery.
Routine extubation criteria.
| Respiratory rate <30 breaths per minute |
| Negative inspiratory force >20mmHg |
| Vital capacity >15mL/kg |
| Tidal volume >6mL/kg |
| Hemodynamically stable with no significant inotropic support |
| Adequate gas exchange (baseline O2 saturation ≥93%; no significant acidosis by arterial blood gas, if applicable) |
| Adequate neuromuscular block reversal (5s sustained head lift) |
Two maneuvers common to anesthetic practice are often performed when determining the feasibility of extubation. The first is the performance of direct laryngoscopy prior to extubation.28 This practice is frequently cited as a way to evaluate the airway prior to extubation for edema and to assess the feasibility of reintubation and is recommended in the DAS guidelines in combination with suctioning of the larynx prior to extubation.5,6 While laryngoscopy prior to extubation may facilitate suctioning or provide some information about the degree of laryngeal edema when a small ETT is used,5 the authors believe that, in most cases, this practice is of limited value for assessing airway patency or ease of reintubation. The reason for this is that the ETT blocks the laryngoscopist's view of the laryngeal inlet and the airway anatomy is deformed by the ETT in situ, leading to an inability to adequately gauge the degree of laryngeal edema and an underestimation of the difficulty of reintubation. No studies have shown that laryngoscopy prior to extubation decreases the incidence of reintubation.
The second maneuver commonly performed is the “cuff-leak test”. A qualitative cuff-leak test is accomplished by removing a spontaneously ventilating patient from the ventilation circuit, deflating the ETT cuff and occluding the end of the ETT with a finger.29,30 If no significant laryngeal edema is present, the patient will be able to breathe around the ETT, as evidenced by auscultation of breath sounds or by the measurement of exhaled CO2 from the oral cavity.31 This test should be performed with caution, as negative pressure pulmonary edema could result if the patient takes a deep breath and no leak is present. A quantitative cuff-leak test is accomplished by comparing the exhaled tidal volumes with the cuff inflated and deflated while the patient is on volume-control mechanical ventilation. A difference between the inflated and deflated tidal volumes of at least 10–25% or 110–130mL in an adult suggests a low probability of laryngeal edema.32–34 Higher cut-off values may be useful in patients with a difficult airway in whom difficulty with reintubation is expected.5 A meta-analysis of the cuff-leak test has shown moderate accuracy of the test for predicting post-extubation stridor and low accuracy for predicting the need for reintubation.35 In the difficult airway, however, where the pre-test probability of extubation failure is greater, the cuff-leak test may still provide valuable clinical information to assist in the decision of whether or not to proceed with extubation.
In the authors’ opinion, a cuff-leak test should be performed on any patient who is felt to be at-risk for extubation failure. While the presence of a cuff leak does not necessarily guarantee successful extubation, the strategic extubation of a difficult airway in the presence of a cuff leak is reasonable. In the absence of a cuff leak, controlled extubation over an airway exchange catheter (AEC) is a consideration; however, it may be prudent to delay extubation if reintubation is expected to be particularly difficult, especially if it is felt that conditions may improve in time. For example, if patient positioning intraoperatively has led to dependent edema of the airway, positioning in a head-up position for a number of hours may decrease airway swelling and result in the development of a cuff leak. Extubation might also be delayed when the lack of a cuff leak is thought to be due to airway inflammation as a result of traumatic intubation or upper airway, maxillofacial, or neck surgery. In these situations, there is some evidence for the administration of corticosteroids at least 4h prior to extubation.36,37 Patients with a difficult airway who persistently fail the cuff-leak test may be considered for tracheostomy.
Strategies for extubation of the difficult airwayOnce the decision has been made that the difficult airway patient can be weaned from ventilatory support and extubated, strategies for a safe extubation can be formulated. The anesthesia practitioner must understand the various options for extubation and formulate a plan of action to regain control of the airway if extubation fails. Benumof considers the optimum approach to difficult airway extubation to be a controlled, step-by-step, and reversible withdrawal of the airway support – an approach the authors are in agreement with.38
The ASA Task Force on Management of the Difficult Airway recommends consideration of the risks and benefits of an awake extubation vs. extubation in the deeply anesthetized state.7 The so-called “deep extubation” has been described in patients with difficult airways. Extubation of a patient while in a deep plane of anesthesia has been widely taught as a means to decrease the risk of laryngospasm or bronchospasm, but there are no adequate studies indicating any real benefit from this approach. While a deep extubation may decrease the risk of coughing and “bucking” prior to extubation, the risk of airway obstruction due to the effects of deep anesthesia on pharyngeal muscle tone is significant.39 A survey of anesthesiologists in the United States identified the difficult airway as the most common contraindication for deep extubation,40 and the authors agree that this practice should generally be discouraged in the face of a difficult airway. Awake extubation is the most appropriate method of removing the ETT in most patients with a difficult airway.
Some practitioners choose not to take any special precautions when extubating the difficult airway with the notion that reintubation is facilitated by prior knowledge of the initial intubation. This “sink or swim” approach is discouraged primarily because the assumption that the technique used for the first successful intubation will be effective for reintubation is incorrect. The airway is dynamic and a completely different airway may be encountered the second time around.
An alternative strategy for extubation in patients with a difficult airway that is mentioned in the ASA Practice Guidelines involves the placement of a stylet-type device or “bougie” through the ETT and removing the ETT over the stylet.7 The stylet is left in the airway until the risk of extubation failure is no longer significant; if reintubation becomes necessary, the stylet is used as a guide over which an ETT is advanced. Many devices have been used in the extubation of the difficult airway including bronchoscopes, nasogastric tubes, gum elastic bougies, and suction tubes.6,15,41 Most of these devices were first described for ETT exchange and many are still used for that purpose.
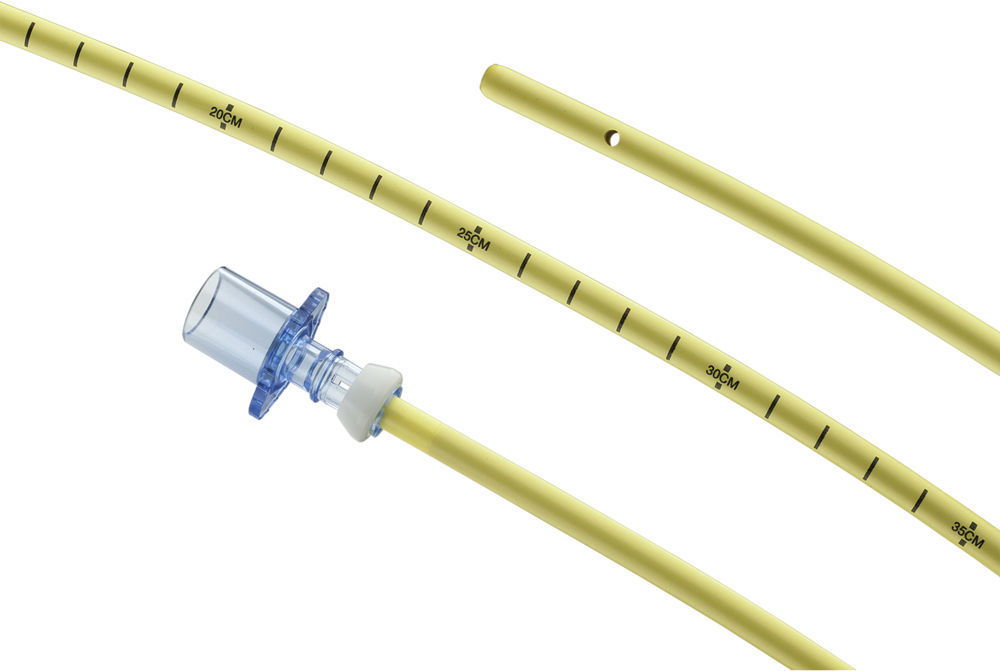
Airway exchange catheters (AECs) are long, hollow, semi-rigid catheters that are designed for ETT exchange, but make ideal catheters for extubation of the difficult airway. There are numerous manufacturers of these types of catheters, but all are based on the same principle: a long, hollow tube is inserted into the in situ ETT to a predetermined depth, the ETT is removed over the catheter, and the catheter remains in place to act as a guide to intubation if reintubation is necessary, to insufflate oxygen via jet ventilation, or to intermittently measure end tidal CO2 from the trachea.18,42–45 These products come in a variety of sizes and have different features depending on the manufacturer. The AEC used most frequently is the Cook AEC (Cook Critical Care, Bloomington, IN; Fig. 1). One study of 51 patients reintubated over a Cook AEC after failed extubation demonstrated a 92% reintubation success rate, with 87% reintubated on the first attempt.44
The recommended size of Cook AEC for use in most adult patients is 11 Fr. This size AEC is well tolerated by an awake patient and allows for reintubation with ETTs as small as 4.5mm internal diameter (ID). Larger patients can usually accommodate a 14 Fr AEC, which will allow for reintubation with an ETT with at least a 5.5mm ID. If it is known that ETT exchange is required (e.g., secondary to a ruptured cuff, resulting in a cuff leak), it may be prudent to use the larger diameter AEC. Smaller AECs can easily be used for the purposes of possible reintubation are usually tolerated without airway topicalization.44 If necessary, 4% lidocaine can be instilled through the AEC to topicalize the trachea or applied directly to the vocal cords in order to increase tolerance of the AEC. These maneuvers should be performed while the patient is still anesthetized to prevent forceful coughing. Once placed, AECs should be taped in place to prevent migration or accidental extubation. The AEC should be well labeled, as they can be easily mistaken for a feeding tube due to their diameter and color.
Cook AECs come with two Rapi-Fit® adapters: one with a 15mm connector for connection to the anesthesia circuit or Ambu Bag and one with a Luer Lock connector for jet ventilation. Prior to use of an AEC for either oxygenation, ventilation, or reintubation, appropriate placement should be confirmed by visualization (with direct or indirect laryngoscopy) or by capnography. The catheters have distance markings to allow proper depth determination. These catheters should be inserted to a 20–22cm depth (no greater than 25cm) when used for orotracheal intubation; when used for nasotracheal intubation, a depth of 27 – 30cm is appropriate. Too deep a placement may result in bronchial perforation and resultant pneumothorax, which is the most significant complication associated with the use of AECs, with one study showing a rate of 1.5%.46 Due to the risk of barotrauma, oxygen insufflation or jet ventilation should only be utilized as a life-saving measure and only in the presence of an unobstructed upper airway.6,47,48
When reintubation over an AEC is attempted, simultaneous direct or video laryngoscopy is recommended in order to retract the soft tissue and facilitate advancement of the ETT over the AEC.49 The smallest effective size ETT should be used in order to minimize impingement of the ETT on laryngeal structures. If a larger ETT is necessary, the Aintree Intubation Catheter™ (Cook Critical Care, Bloomington, IN) can be used to minimize the gap between the AEC and the ETT, facilitating advancement of the ETT through the glottis.50 Alternatively, the Parker Flex-Tip™ ETT (Parker Medical, Englewood, CO), designed with a soft, curved, anteriorly located bevel, minimizes the gap between the AEC and the lumen of the ETT, allowing smooth passage into the trachea.27,51
Monitoring after extubationIt is important to note that extubation failure may not occur immediately after tracheal extubation and, as such, the patient with a difficult airway should be closely monitored during transport and in the recovery area. Otherwise, airway obstruction may go undetected until a severe adverse outcome has occurred. The NAP4 study attributed a significant number of adverse outcomes to a lack of adequate postoperative monitoring.3,5 Continuous standard monitoring (telemetry, pulse oximetry) is required and capnography should be available.5,6 Some patients at particularly high-risk (e.g., those with OSA or rheumatoid arthritis) may need close monitoring for an extended period of time, as long as 24–48h.5 All necessary equipment for reintubation should be readily available n the recovery area, including equipment for invasive airway access.
ConclusionExtubation of the trachea is not without risk. The anesthesia practitioner should take many considerations into account, including the ease of the initial intubation, the patient's medical status, the setting in which the extubation is going to occur, and finally, their skills and preferences. The potential for reintubation following extubation of a difficult airway is always present. The extubation strategy should carry low risk and minimal patient discomfort, and should optimize the objectives of airway access, oxygenation, and ventilation. Tracheal reintubation over AECs is neither without complications nor always successful; therefore, those who use these devices should be familiar with the equipment and their techniques, their potential complications, and alternatives in case of reintubation failure. The anesthesia practitioner should be familiar with the extubation strategies developed by the ASA Task Force on Management of the Difficult Airway and the Difficult Airway Society. Finally, high-risk patients should be identified whenever possible.
FundingNone.
Conflict of interestCarin Hagberg is an unpaid consultant for Ambu A/S and has research grants from Ambu A/S, Cadence Pharmaceuticals, and King Systems. Carlos Artime is a member of the Speakers’ Bureau for Mylan Pharmaceuticals and has a research grant from Cadence Pharmaceuticals.
Please cite this article as: Hagberg CA, Artime CA. Extubación del paciente perioperatorio con una vía aérea difícil. Rev Colomb Anestesiol. 2014;42:295–301.