Facet block is a procedure used in patients with facet arthrosis in which several other medical techniques have failed. In our country, there is no evidence or studies regarding its efficacy, thus the interest in its demonstration. A retrospective observational cohort study was carried out on patients intervened between January 2005 and December 2009 at Clínica CES. Data were collected from the patient's clinical records by means of a survey designed for that purpose. Also, positive clinical outcomes were correlated to age, gender, occupation, evolution time, motor and sensitive symptoms as well as comorbidities. The sample included 232 patients between the ages of 21 and 92, with an average age of 56.9 (±14.6) years, and a lumbar pain evolution time of 2 years in 40% of the individuals in the sample. The most commonly used imaging test before the procedure was MRI in 42.2% of patients, CT scan was used in 38.31% and X-rays in 7.46%. The procedure was effective in 78% of patients. In sum, facet block is a therapeutic method, given that most patients improved after its completion. These findings are consistent with other studies that have showed a decrease in physical and functional limitations of the patients. Besides, improvement of the patient's state confirms a lumbar facet syndrome, so it is a diagnostic procedure as well.
El bloqueo facetario es un procedimiento usado en aquellos pacientes con artrosis facetaria en los cuales han fallado los múltiples tratamientos médicos. En nuestro país se desconocen estudios o estadísticas que demuestren su efectividad por lo que se consideró pertinente demostrarlo. Se realizó un estudio observacional retrospectivo de una cohorte de pacientes intervenidos en el período comprendido entre enero de 2005 y diciembre de 2009 en la Clínica CES. Se recolectó información de las historias clínicas mediante un formulario diseñado para tal fin, además se relacionó la existencia de mejoría del paciente posterior a la intervención con edad, sexo, ocupación, tiempo de evolución, síntomas motores y sensitivos previos y enfermedades asociadas. La población fue de 232 pacientes entre 21 y 92 años, con una edad promedio 56,9 (±14,6) años, con un tiempo de evolución del dolor lumbar de 2 años en el 40% de la población estudiada. La resonancia magnética fue el estudio más utilizado previo al procedimiento en 42,2% de los pacientes, la tomografía en 38,31% y los Rayos X en 7,46%. El procedimiento fue eficaz en el 78% de los pacientes. En conclusión el bloqueo facetario es un método terapéutico, ya que se vio mejoría de la sintomatología en la mayoría de los pacientes estudiados. Esto es coherente con otros estudios realizados, donde también se ha evidenciado disminución de las limitaciones físicas y funcionales de los pacientes. Además, es un procedimiento diagnóstico ya que la mejoría con esta técnica indica que la patología sí era facetaría.
The structure of the spinal column is very complex as a result of the diversity of components that form it and its close relation to nerve roots and the spinal cord. More than 80% of individuals will suffer cervical and lumbar column related distress at some point in their lives.1
The main functions are muscular insertion and movement, motion restriction, protection of the spinal cord and sustaining the weight of the body. The apophyses, or vertebral facets are contact surfaces between any two vertebrae that restrain certain motions and prevent vertebrae to move forward. There are two superior articular facets and two inferior ones originated between the pedicles and the vertebral laminae.2
Lumbar pain is one of the most common reasons for medical consultations. It is often a cause for physical limitation in patients above 45 years of age and it is the fifth most common cause for hospitalization, which carries a great social, economic and working repercussion.1 It is important in epidemiology because it is a chronic malady, potentially incapacitating that affects the patient's life quality and performance. In 1911, Goldwaith stated the “peculiar qualities of facet articulations” and considered them responsible for instability and lumbar pain. Ghormley used the term “facet syndrome” in 1933 and labeled it the most common cause of chronic lumbar pain.1
Lumbar facet articulations are acknowledged for the origin of lower back pain and referred limb pain. The facet articulations are innervated by the medial branch of the dorsal root. Studies in neuroanatomy, neurophysiology and biochemistry have shown the presence of encapsulated nerves in lumbar articular facets.3
Facet arthrosis is caused by normal erosion of the articular cartilage. The prevalence of thoracic pain is 15% of the general population compared to 56% for lower back pain and 44% for cervical pain.4 As of the age of 30, initial signs of arthrosis are normal findings. Facet pain occurs because these articulations are very close to the intervertebral orifices and the related nerves are affected. The pain is transmitted by dermatomes and the associated muscles show spasms. Other less common conditions that may lead to facet arthrosis are capsular osteochondral anomalies, bone anomalies, degenerative changes, sinovial cysts, unilateral facet hypertrophy and bad postures. Within the etiology of facet pain and facet articulation syndrome is trauma, inflammation, arthritis, sinovial impingement, meniscus entrapment and chondromalacia.
The physiopathology of facet arthrosis is inflammation that causes sinovial distension and can easily compress a nerve root and thus cause irradiated pain. Lumbar arthrosis generally causes irradiated pain in lower limbs.5 Diagnosis can be confirmed by any of the following imaging techniques: facet arthrography, X-rays, CT scan and MRI (the two latter are the most reliable).6 Diagnosis is based on a clinical basis, infiltrations and some uncertain radiographic signs. Unclassified changes in CT scans and X-rays have been reported. In MRI, it is possible to classify facet arthrosis in three degrees.7
Regarding treatment and potential diagnosis, there is lumbar facet block to consider, in which either a local anesthetic and a steroid are injected into the articulation or selective blocking of the medial branches of the spinal nerve that involve the facets. This steroid reduces inflammation and the anesthetic reduces the pain when applied on the nerve or the facet. If the patient improves, the diagnosis of facet joint arthrosis is confirmed, regardless of the time in which it occurs. These patients are candidates to medial branch RF, a more definite treatment. CT scan and MRI provide a better visualization of anatomical structures and are also the guiding methods of choice for this procedure.6
The patient is taken to the operating room after sedation and proper antiseptic measures are carried out. In a prone position, with a needle, the articular facets are identified with an image intensifier and fluoroscopy. Diagnostic imaging in facet and nerve root blocking is considered useful as a diagnostic and therapeutic tool and decreases morbidity when compared to those carried put without imaging techniques.6 Once location is ensured, two drugs are injected: a long effect steroid and a local anesthetic (Bupivacaine 0.25%). No more than 1 cc must be used in facet blocking because it is the maximum average capacity of the articular capsule. With this dose, a significant pain relief and functional improvement of the facet joint has been achieved.8
This procedure was conceived due to the necessity of therapeutic blocking and diagnosis in patients with facet related lumbar pain in which all other existing therapies failed.9 It is a feasible option for treatment of chronic lumbar pain because it is a specific intervention that has shown an important clinical improvement.10
The aim of the study was to determine the efficacy of lumbar facet blocking in a cohort with 5 years of procedures and assessment of the patients with failed back syndrome; hoping to expand treatment options and improve clinical outcomes. The cause for it is offering an option for diagnosis, improvement and treatment to patients who have undergone other several therapies.
Materials and methodsThis is an observational, retrospective study in which the clinical records of patients diagnosed with facet arthrosis at Clínica CES between January 2005 and December 2009 were included. Factors involved in positive outcomes were observed and analyzed. The individuals in the sample were representative of all lumbar pain patients.
Relations between other factors described in literature were sought after, such as occupation, evolution time, pain location, motor and sensitive symptoms, age and gender.
To measure efficacy, the patients were questioned on their post-operative improvement and classified answers into 5 items: no improvement, mild improvement, moderate improvement, fair improvement and full symptom remission.
A recollection instrument was used in data collection to ensure all pertinent data was obtained. It was a self-administered process that guaranteed patient privacy and anonymity. The medical records, the procedures and post-surgical assessment were all carried out by anesthesiologists.
Data processing and analysis were input in an Excel® and was then transcribed into the STATA® VERSIÓN 10 statistics program. A single variable analysis was carried out initially and a multivariable analysis was performed based on the findings of the first.
ResultsThe studied sample was formed by a total 232 patients between 21 and 92 years and averaging 56.9 years (±14.3 years). 65.5% (152/232) of individuals in the sample were females.
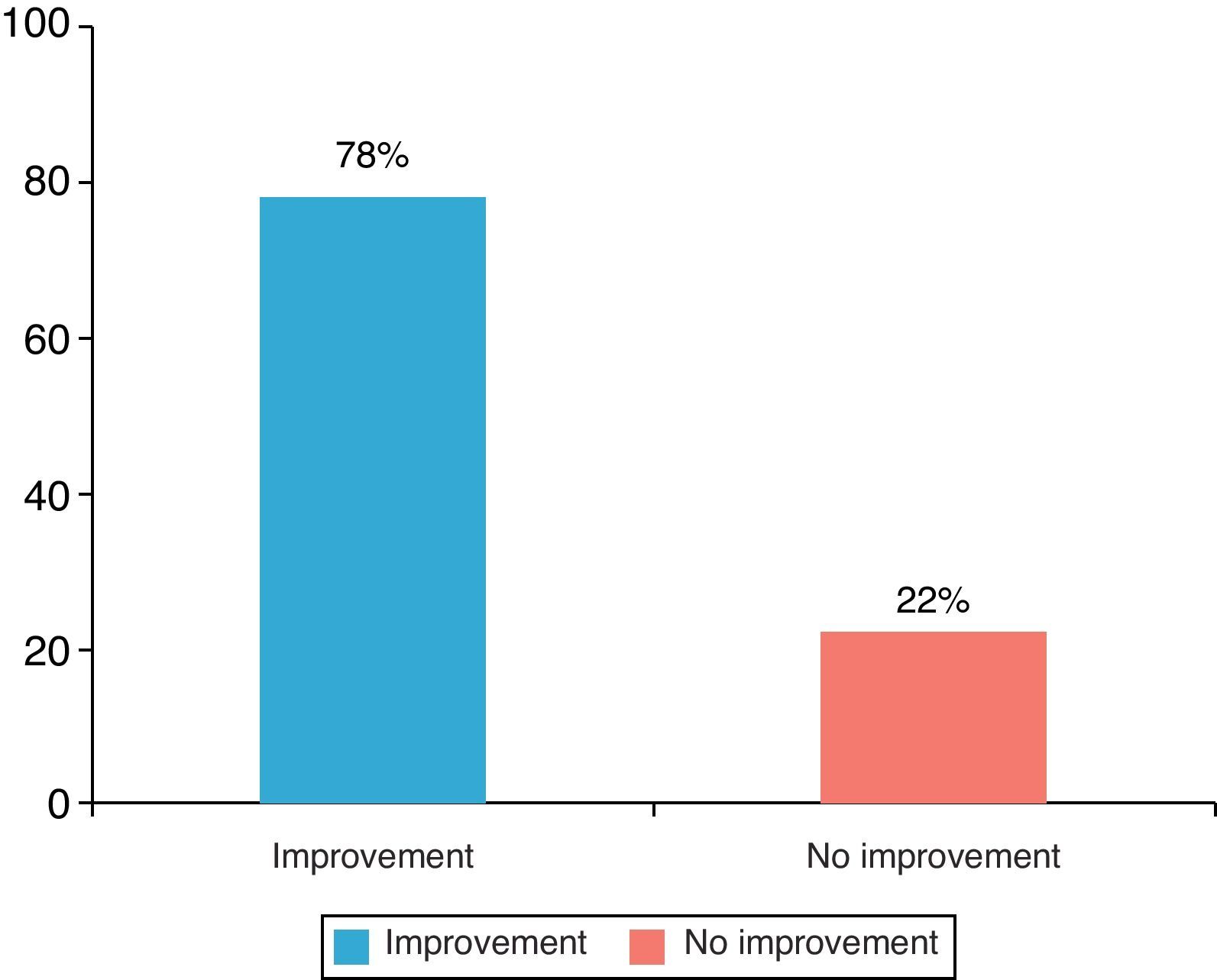
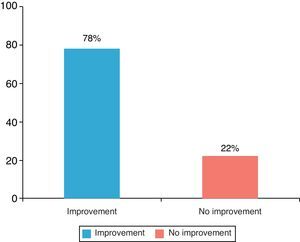
Regarding symptoms, 78% (170/218) of patients reported some degree of improvement as shown in the following graph (Fig. 1).
Regarding occupation, it was observed that 66.96% (150/224) did mild physical activity, 24% (54/224) were sedentary and 8.93% (20/224) had grinding work.
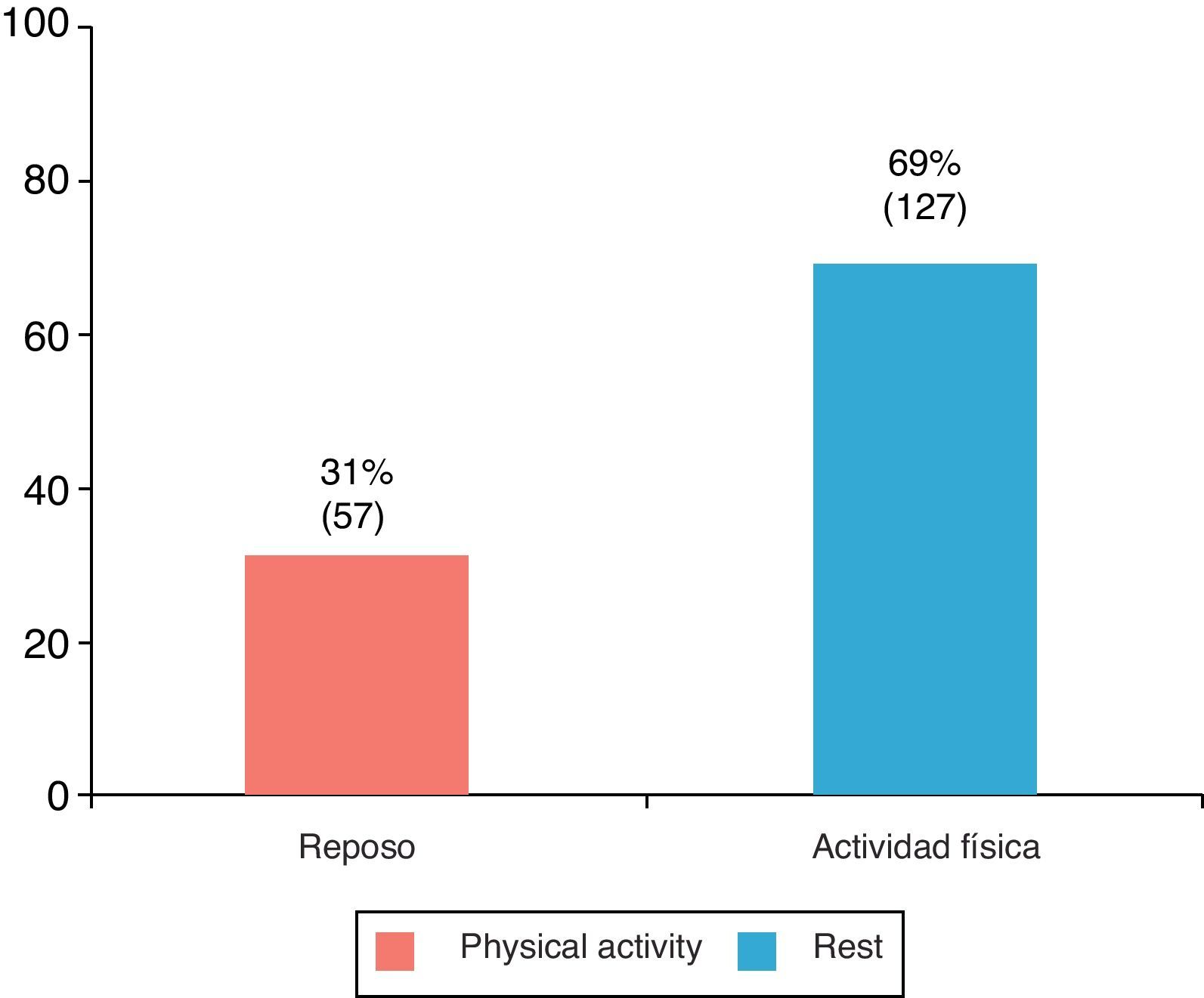
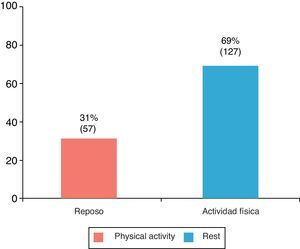
When factors related to worsening of the symptoms were studied, findings were: 69% (127/184) worsened with physical activity and 31% (57/184) worsened with rest (Fig. 2).
We determined that 88.46% (101/114) of patients had degenerative arthrosis as their first associated diagnosis, followed by disc pathology in 62.28% (71/114) and 4% (4.5/114) were other less relevant illnesses, such as narrow lumbar conduct, disc hernia or radiculopathy.
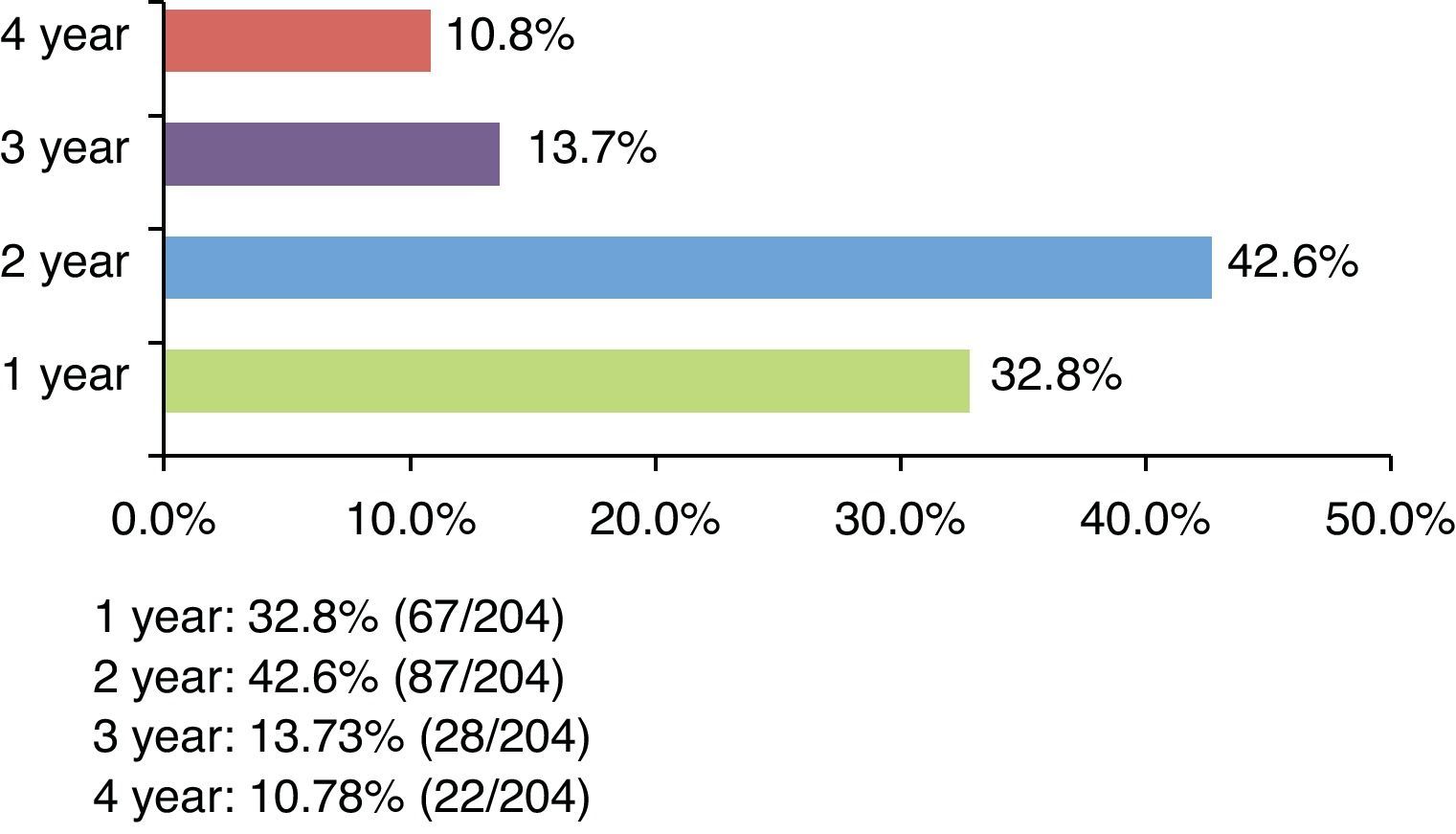
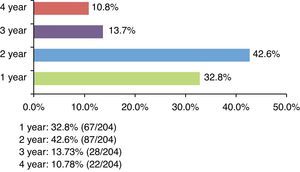
The time span of evolution yielded the results shown in the following graph (Fig. 3):
1 year: 32.8% (67/204)
2 years: 42.6% (87/204)
3 years: 13.73% (28/204)
4 years: 10.78% (22/204)
The main motor symptom was walking difficulty, and it was present in 67.65% (69/102). The sensitive symptoms were mostly paresthesias, found in 48.10% (76/158) and paresthesia and dysesthesia 43.67% (69/158); single dysesthesia were found in 8.23% (13/158). 81.90% (190/232) of patient described the pain as irradiated.
Diagnostic aids used were: nuclear MRI in 42.29% (85/201) CT scan: 38.31% (77/201) and simple X-rays: 7.46% (15/201). The rest were combined methods.
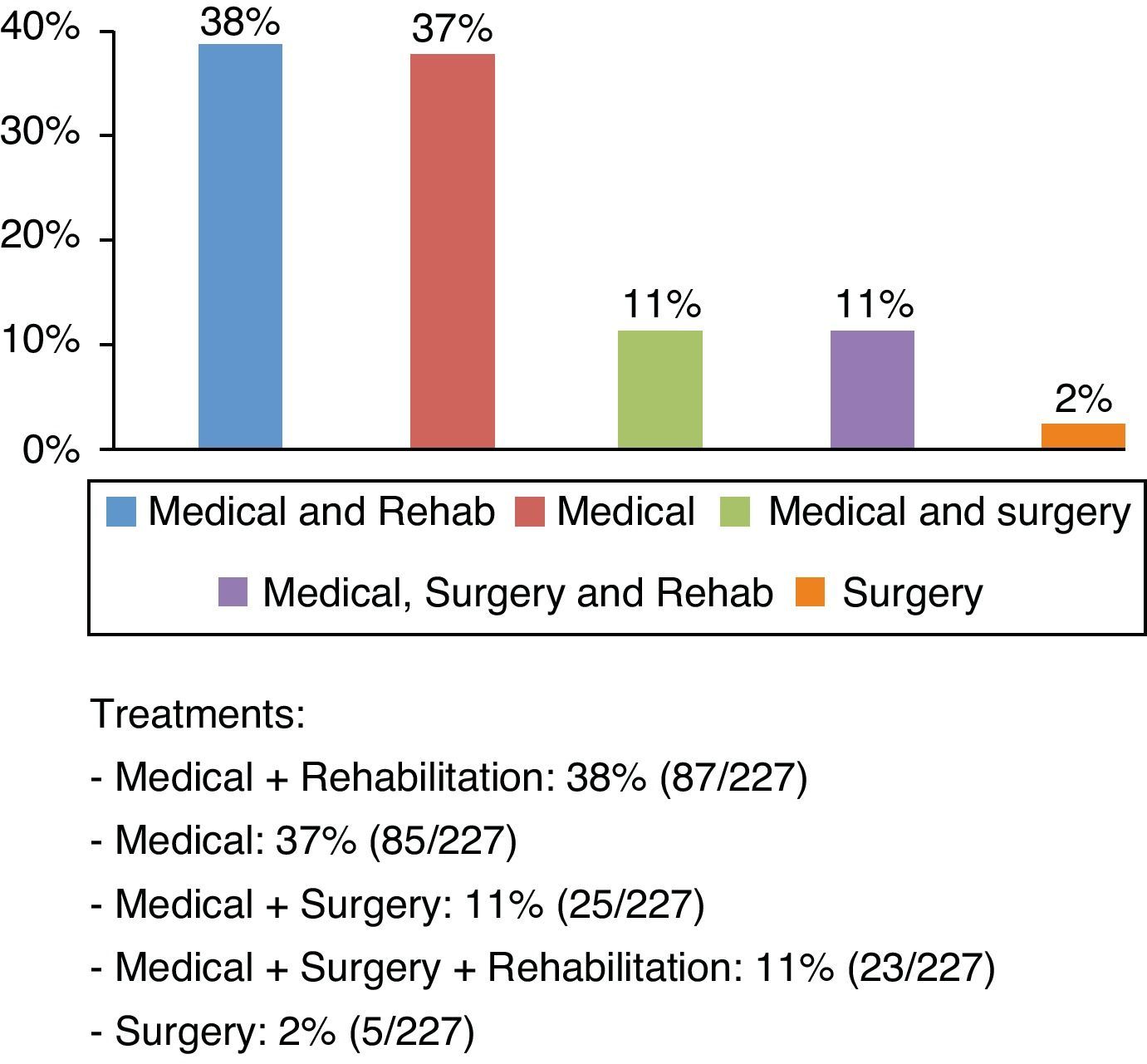
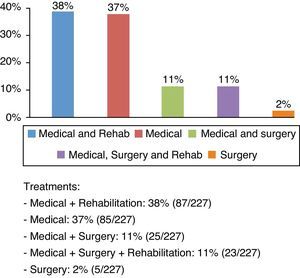
Regarding previous treatments of the patients the following combinations were found (Fig. 4):
Treatments received by patients. The type of procedure was bilateral in 93.10% (216/232), unilateral right in 5.17% (12/232) and unilateral left in 1.72% (4/232). The location of the procedure was mainly in 4 points: L1–S1: 36.36% (84/231); L2–S1: 22.08% (51/231); L2–L5: 15.15% (35/231); L1–L5: 13.42% (31/231). Medical and Rehab: 38% (87/227); Medical: 37% (85/227); Medical and Surgery: 11% (25/227); Medical, Surgery and Rehab: 11% (23/227); Surgery: 2% (5/227).
Treatments:
- -
Medical+rehabilitation: 38% (87/227)
- -
Medical: 37% (85/227)
- -
Medical+surgery: 11% (25/227)
- -
Medical+surgery+rehabilitation: 11% (23/227)
- -
Surgery: 2% (5/227)
The procedure was carried out in four main locations:
L1–S1: 36.36% (84/231)
L2–S1: 22.08% (51/231)
L2–L5: 15.15% (35/231)
L1–L5: 13.42% (31/231)
The procedure type was bilateral in 93.10% (216/232), unilateral right in 5.17% (12/232) and unilateral left in 1.72% (4/232).
DiscussionThis study found that facet blocking was effective in 78% of patients, given that all of them showed some improvement. These findings are consistent with the results of several studies, such as Manchikanti et al.: lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial: Clinical Trial NCT00355914, in which 82% of patients had pain decrease, and 78% of patients showed functional improvement.6 Another trial by the same author titled: evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up, found that up to 90% of patients showed a 50% or greater decrease in pain and a 40% increase in functionality.11 In addition, the trial titled Therapeutic efficacy of facet joint blocks led by Gorbach et al., although it had fewer patients, showed that 31 patients (74%) improved their condition immediately after facet blocking and 14 patients (33%) showed medium-term improvement.12
This means that these patients did have a facet malady, which is why the facet blocking was effective. If they showed no improvement, it likely they had some other pathology. Because of this, facet blocking is useful for diagnosis as it is for treatment.13 These patients are candidates for RF neurotomy as definite treatment.
Therapeutic facet blocking with or without use of steroids may provide valuable information on the management of chronic lumbar pain and enable more aggressive treatment.14
In all likelihood, the best marker for lumbar facet joint pain lies in a proper assessment and integration of clinical data, physical examination findings, imaging tests and anesthetic facet blocking. In this way, the pain relieved in this procedure is increased because of an adequate patient selection.15
Aside from demonstrated efficacy, other variables were measured to be correlated with the pathology in question. Regarding gender, most of the patients were female. Most patients claimed to have pain related to physical activity, especially walking, as well as irradiated pain with paresthesias and dysesthesias. Also, most patients had a two-year long symptom evolution time span and had undergone several medical treatments, including rehabilitation, medical treatment, and even surgery. This shows that it is a chronic illness of difficult management for which facet blocking is a fair alternative for pain relief; yet it is often performed only after several attempts with other treatment options. The most important data from imaging studies were extracted from MRI and CT scan tests, though some patients only had X-rays. This comes to show that imaging studies may be unclear and that facet blocking has a diagnostic utility.
Psychopathology has shown a positive association with chronic lumbar pain and is often a part of its etiology. Depression, anxiety disorders, individual somatization or combinations of several disorders contribute greatly to the cause of this disease.8 This trial did not analyze the influence of psychopathological disorders.
ConclusionConclusively, the base for this study is that facet blocking is effective for the improvement of symptoms in most patients. As in this trial, other studies carried out in several countries have shown the efficacy of this procedure. It is important to say that facet joint pain is a difficult diagnosis due to the fact that there is no precise method to investigate it. Facet blocking provides a therapeutic strategy for its management as well as a diagnostic tool, as mentioned before.
Regarding variables that may relate to this pathology, it is important to consider that most patients claim to have symptoms for a long time, so it mostly becomes a chronic disease. The most important symptoms appear after physical activity, especially walking and the pain is generally irradiated to the lower limbs, and it becomes an incapacitating illness.
Before considering facet blocking, the majority of patients undergo several treatment options, including rehabilitation and even surgeries. This is because there is no specific treatment for facet joint pain syndrome and because diagnosis is difficult. For all this, facet blocking is an important treatment and diagnostic option that has proved to be effective.
Chronic lumbar pain management is challenging not only for general medicine professionals but specialized physicians as well. Having found the efficacy of facet blocking therapy in this trial, a great door has been opened for the treatment of this pathology. It offers an alternative for patients to undergo temporary or permanent treatment for their pain and to those who have tried other treatment alternatives with no result. The importance of facet blocking is not only regarding pain management but also improving the patients’ life quality.
FinancingThis study was carried out with the support of the Epidemiology Department at Universidad CES for statistical analysis. Data collection was done in collaboration with the Anesthesiology Department and the medical record database at Clínica CES.
Conflicts of interestNone to declare.
Please cite this article as: Ospina Á, et al. Eficacia del bloqueo facetario en pacientes con síndrome facetario lumbar. Rev Colomb Anestesiol. 2012;40:177–82.