Palliative care for end-of-life patients in Bogotá is still in the process of consolidation. This type of care demands high technical and scientific standards, in addition to supporting the patient and family in making end-of-life ethical decisions, particularly with respect to sedation, hydration and feeding.
MethodologyStatistical descriptive analysis of a cohort comprised of 164 terminally ill patients treated in private practice in Bogotá between 2008 and 2012.
ResultsOut of the 90 patients who received care until their demise, the average age was 77 years old, including 63% women, 30%, university students, 41% widowers, and 84% Catholics. 8 patients had no medical insurance. 52% of the patients were cancer patients, 91% received home care, the average number of care days was 45 and the usual route of administration of medicines was subcutaneous. The most commonly used drugs were tramadol, ranitidine and midazolam. 73% of the patients required superficial sedation. In some cases, feeding and hydration were administered through alternate routes and in others were discontinued.
AnalysisThere is a need to study the conditioning factors for private medical home care and for maintaining this type of care until the end of life. Characterizing this population enables the identification of some useful information for the administration of end-of-life care in the country.
El cuidado médico paliativo en Bogotá para pacientes terminales sigue en proceso de consolidación. Esta atención exige altos estándares técnicos y científicos, así como el apoyo a las decisiones éticas al final de la vida del paciente y sus allegados, especialmente en cuanto a la sedación y al uso de hidratación y alimentación.
MetodologíaSe realizó un análisis estadístico descriptivo de una cohorte de 164 pacientes terminales atendidos en práctica médica privada en Bogotá entre 2008 y 2012.
ResultadosDe los 90 pacientes atendidos hasta su fallecimiento se encontró un promedio de edad de 77 años; el 63% mujeres, el 30% universitarios/as, el 41% viudos/as, el 84% cató-licos/as, y 8 pacientes sin afiliación al sistema de seguridad social. El 52% de los pacientes fueron oncológicos, y el 91% se atendieron en sus casas. El promedio de atención fue de45 días, y la vía más utilizada para la administración de medicamentos fue la vía subcutánea. Los medicamentos más usados fueron el tramadol, la ranitidina y el midazolam. El73% de los pacientes requirieron sedación superficial. En algunos casos se continuaron y en otros se interrumpieron la alimentación y la hidratación por vías alternas.
AnálisisSe requieren estudios que den cuenta de los factores que condicionan la solicitud de atención médica privada domiciliaria, o para mantenerse en este tipo de atención hasta el final de la vida. La caracterización de esta población permite identificar algunos elementos útiles para la práctica del cuidado paliativo en el país.
End-of-life medical care of patients involves some specific internationally defined guidelines. In 2007 the WHO established some palliative care recommendations as an urgent public policy to care for cancer patients and other chronic lethal conditions.1
There are 3 measures for developing palliative care from the public health perspective2: public policy, educational policy, and pharmaceutical policy to ensure the availability of essential medicines.
Palliative home carePalliative home care requires around-the-clock availability, proper, state-of-the-art scientific and humane knowledge and adequate familiar, social and sanitary conditions to meet all the end-of-life needs of the patient. It is based on providing pain relief and alleviating other symptoms, in addition to understanding death as a normal process, as well as helping families to handle the disease of the patient and their own bereavement.
A number of studies show the preference of both patients and families to be at home until the patient's demise,3,4 with home care that ensures good quality of life even in our own environment.5
According to Twycross, the art of medicine resides in deciding when vital support is basically useless and thus when to allow the patient to die with no further impediment. A physician is not legally or ethically obliged to preserve life âat all costsâ. Life should be preserved as long as it is biologically sustainable.6
The physical and psychological end-of-life symptoms demand active and very close medical care. Currently, the therapeutic armamentarium provides excellent levels of analgesia, pursuant to the WHO recommendations for relieving cancer pain that date back to 1986,7 and later revisions, as well as the recommendations by PAHO,8 national associations9 and government agencies.10 The availability of opiates in BogotÃĄ is good; however, there are still some limitations to access the medication.
While there is an increasing number of consolidated units and palliative care groups in Colombia, due in part to advances in the legislation,10 there is still considerable difficulty to provide enough coverage to this population and to ensure ethical end-of-life decisions.11
Palliative care sedationPalliative care sedation is valuable at different points in time, whether intermittent or continuous, in accordance with the patient's condition. The Spanish Society of Palliative Care defines sedation as the purposeful administration of drugs, at the doses and combinations required, to reduce the awareness of a patient with advanced or terminal disease, to the extent needed to adequately relief one or more refractory symptoms,12 provided that the patient or legal representative has given his/her explicit consent.13
Guidelines for end-of-life sedation have been developed in various countries.14,15 In Colombia there are several case reports16,17 and a consensus was recently published for sedation administered by non-anesthesiologists.18
Use or interruption of hydration and nutrition during permanent sedation in palliative careOne of the most complex end-of-life interventions is caring for the pathophysiological mechanisms while the patient is dying. When the process is irreversible and death is imminent, starting interventions to hydrate and provide nutritional support that require hospital transfers, surgical procedures (venodisections, central venous catheters, gastrostomies) and even regular venopunctures for a patent venous access does not help in reducing the suffering of the family, the patient or the health team. Moreover, these measures fail to respond to the pathological conditions arising in most patients with a reduced osmotic pressure that translates into symptoms (edemas, rattles, fluid weight gain) that hinder the adoption of comfort measures or actions to at least avoid any further discomfort.
The instructions given by the patient while still aware, informed, escorted and with certainty that his/her suffering will not be further aggravated, and who enjoys the support for a family or social network that ensures that the patient is not experiencing any physical symptoms such as thirst or hunger, shall be followed. Within this context, the ethical recommendations for decision-making based on the proportionality of the medical intervention are applicable.19
There are no studies in Colombia â more specifically in BogotÃĄ â describing the characteristics of the population that asks for palliative care. Neither the methodology nor the results of interventions such as home care sedation, hydration and nutrition management in the terminal patient are well known. Thus, the purpose of this paper is to describe a population of terminally ill patients that asked for private medical care from 2008 to 2011 in BogotÃĄ, including the proportion of patients requiring sedation and nutritional and hydration management during this stage.
Materials and methodsA cohort of 164 patients undergoing medical care were followed from January 1st through June 30, 2012. The patients were diagnosed with end-stage disease and they asked for private medical care in BogotÃĄ, Colombia. The information was collected from the medical records of a private health care provider, using a form designed to record the information that was transferred to an Excel database. A descriptive statistical analysis was then performed on the socio-demographic variables, the place where care was provided, the primary lethal diagnoses, the management of the patients, length of care, use of terminal sedation and limitation of therapeutic efforts. This article was endorse by the Colombian Institute of Bioethical Studies (ICEB).
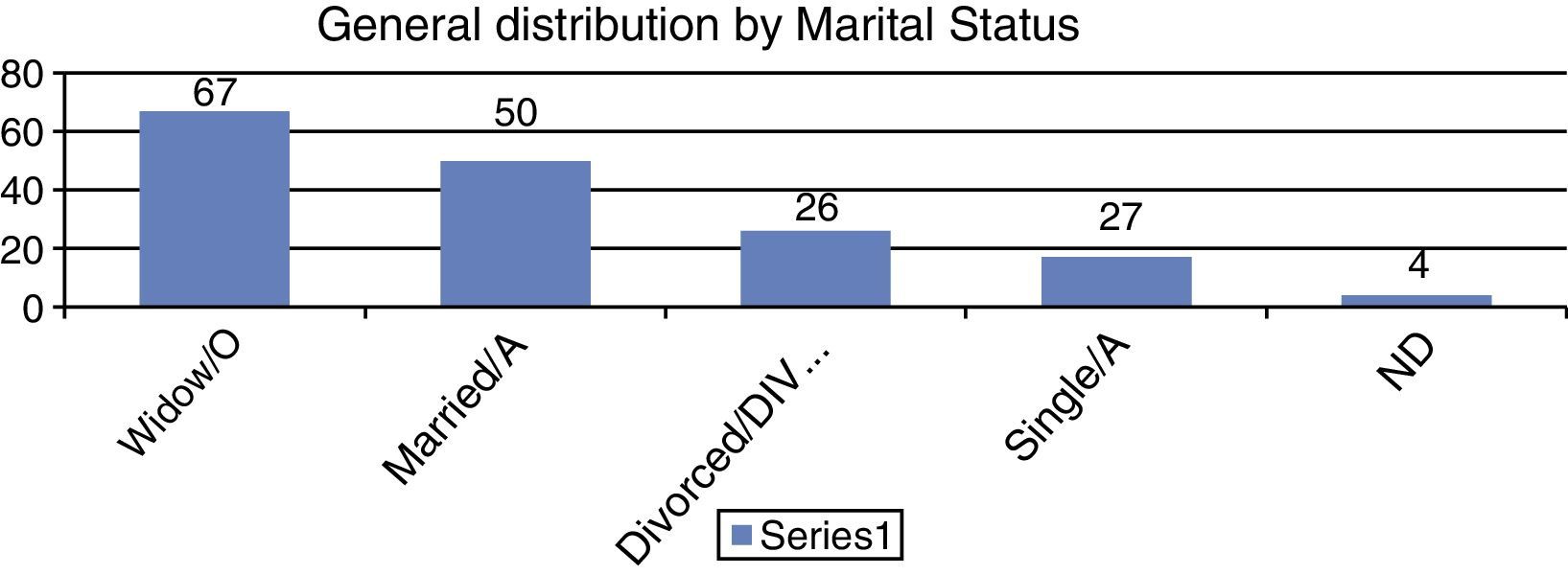
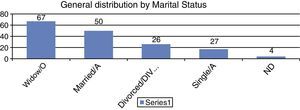
ResultsOf the 164 patients, 54% (n=90) received care until their demise and the corresponding death certificate was issued. The rest of the patients decided to seek care elsewhere. The age range of the patients that were taken care of until their demise was 37â94 years old, with a mean of 77 and a 3.5 standard deviation. The age range of the dropout patients was 13â99 years old, with a mean of 74 and a standard deviation of 4.0. The gender distribution was similar, with 63% females (n=103) and 41% widowers (n=67). The total distribution is presented in Fig. 1.
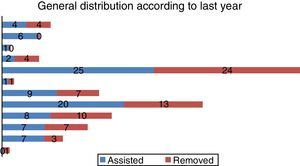
The general distribution in accordance with their last year of education was as shown in Fig. 2; most patients completed their last year of university education and high-school. The range included no education in one patient, to 6 people with a master's degree.
According to the medical record, 138 patients were Catholics (84%), and 20 medical charts fail to specify the religion; 3 patients said they did not practice any religion, while 3 of them were: Jew, Adventists and Menonits.
Most patients were affiliated to the Social Security System: 49.4% (n=81) were in the obligatory prepaid medicine system; 7.9% (n=13) belonged to special regimes (military, professors, Ecopetrol) and 1% to the subsidized regime 1% (n=2). Additionally, 25% (n=41) had national or international insurance, complementary insurance plans or HMOs. Only 8 patients did not have any type of insurance and were paying for their care from their own pockets.
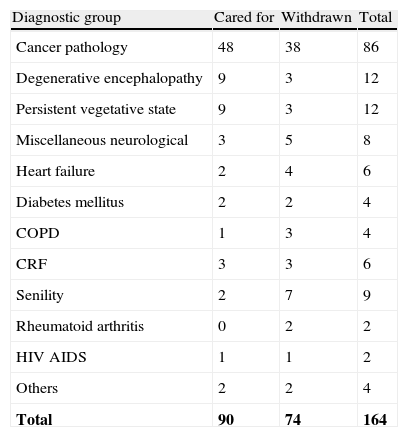
Diagnoses52% (n=86) of the patients cared for had some form of cancer and 25% (n=41) had neurological conditions; the rest included heart disease, pulmonology, renal and other conditions as shown in Table 1. Among the group of oncology patients, the most frequent tumors were prostate tumors (n=11; 6.7%), breast (n=9, 5.48%) and brain (n=9, 5.48%).
Non-oncological diagnostic characteristics leading to the end-of-life phase.
| Diagnostic group | Cared for | Withdrawn | Total |
| Cancer pathology | 48 | 38 | 86 |
| Degenerative encephalopathy | 9 | 3 | 12 |
| Persistent vegetative state | 9 | 3 | 12 |
| Miscellaneous neurological | 3 | 5 | 8 |
| Heart failure | 2 | 4 | 6 |
| Diabetes mellitus | 2 | 2 | 4 |
| COPDÂ | 1Â | 3Â | 4Â |
| CRFÂ | 3Â | 3Â | 6Â |
| Senility | 2 | 7 | 9 |
| Rheumatoid arthritis | 0 | 2 | 2 |
| HIV AIDSÂ | 1Â | 1Â | 2Â |
| Others | 2 | 2 | 4 |
| Total | 90 | 74 | 164 |
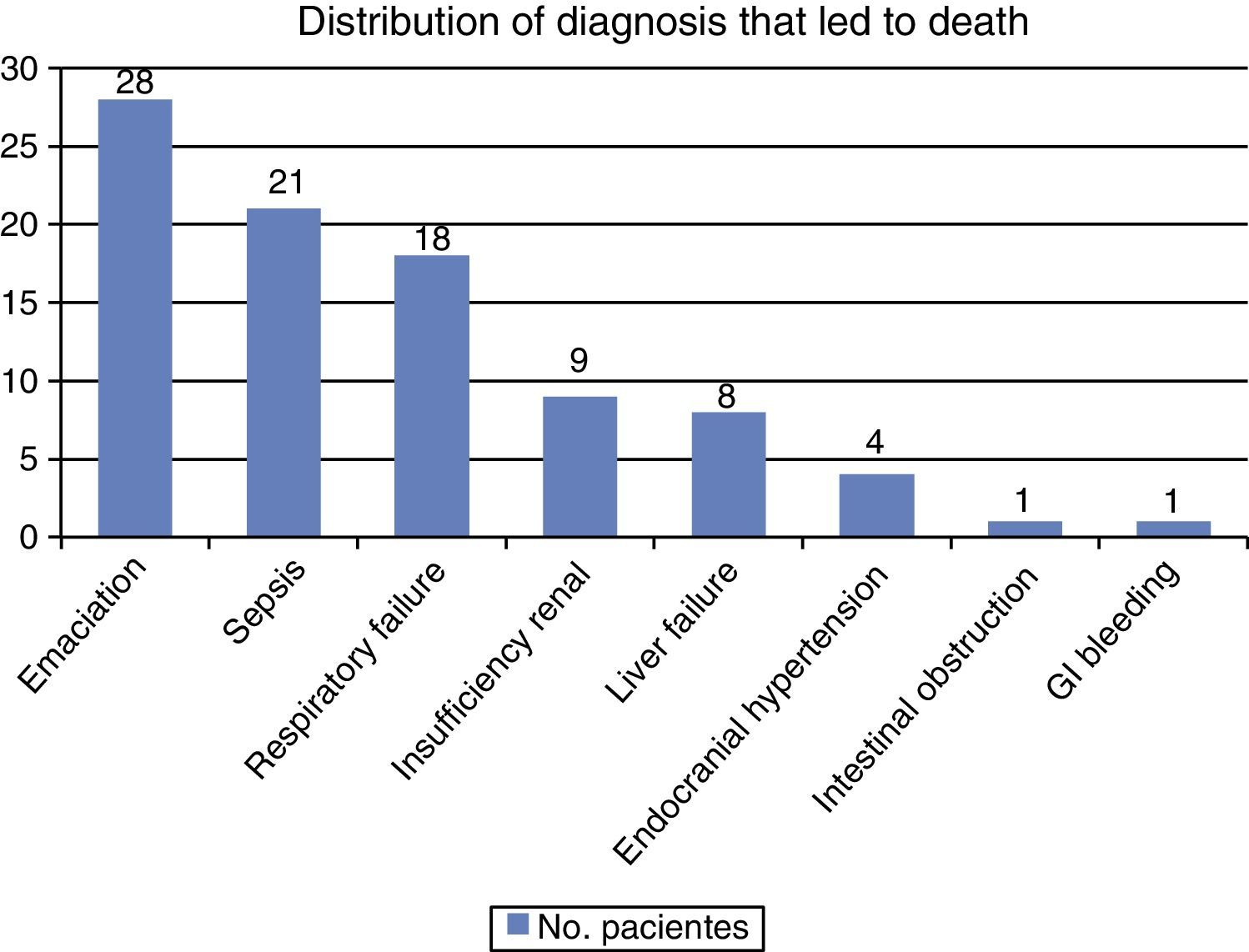
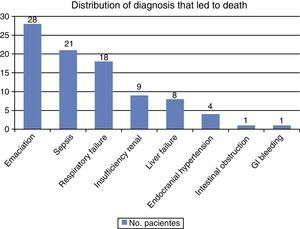
Of the patients that were taken care of until their demise, the main causes of death were emaciation, sepsis and respiratory failure. Fig. 3 illustrates the various lethal diagnoses.
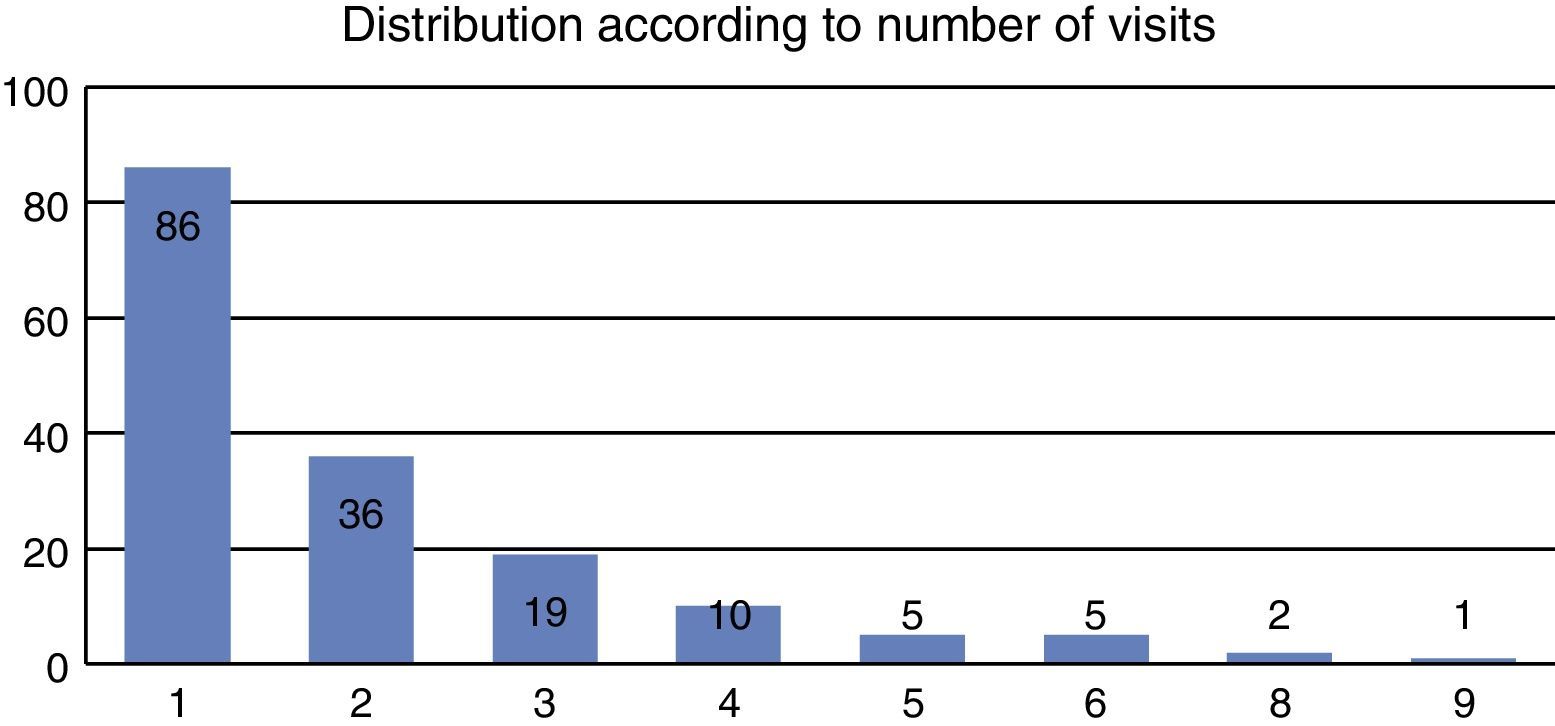
91% (n=150) of the cases received medical home care, 11 (7%) were admitted at geriatric units and 3 (2%) went to private 3rd level health care institutions. The number of visits ranged between 1 and 9 visits, though most of them â 52% (n=86) only had one visit. Fig. 4 illustrates the distribution of the number of visits.
The length of care of patients who stayed until the end varied from 1 to 361 days, with a mean of 45.6 days, with a standard deviation of 16.06.
The preferred route of administration of the drugs was the oral route and the second choice was subcutaneous; the intramuscular route was only used in 10 (11%) of the sepsis patients. Inhaled administration was used in all patients with respiratory failure (n=18, 20%) and in 10 (11%) patients with death rattles. No IV or subcutaneous catheters were used.
MedicinesThe most frequently used drug was tramadol in 74 patients (82%). Only ten (11%) patients did not require painkillers. Hydromorphone was used in 2 (2.2%) patients, while morphine was used in 4 (4.44%). The tramadol doses used ranged between 50mg/day and 1800mg/day, with an average of 177mg/day.
The second most frequent drug used was subcutaneous ranitidine in 70 patients (77%) at doses ranging from 50 to 100mg/day.
The proportion of midazolam was similar and it was administered to 70 patients (77%). 5 of these patients only received 2mg rescue doses as needed. The rest of them used a dose range between 2.5mg/day and up to 90mg/day. The only patient who received a 90mg/day dose had a considerable body surface area, had used opiates on an on going basis for over 2 years and was in persistent vegetative state. The average dose used was 15mg/day.
The common antiemetic agent used was metoclopramide in 73% (n=66) and alizapride in 16% (n=15). 10% (n=9) of the patients did not require any antiemetics.
Other less frequently used drugs were furosemide (n=3; 3.3%), vitamin K (n=5; 5.5%), ipratropium bromide solution inhaler (n=25; 27.7%), prednisolone (n=6; 6.6%) and atropine (n=6; 6.6%). Some patients however used more than one medicine.
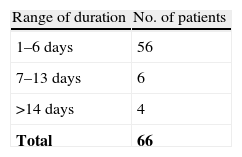
Palliative sedation66 patients, 73% of the total number of patients that received end-of-life care until their demise, were treated with medicines to maintain a superficial sedation. The sedation lasted from 1 to 35 days, with an average of 4.1 days; the standard deviation was 1.12. Table 2 shows the sedation time range distribution; 85% (n=56) stayed sedated for less than one week, while 7 patients were sedated for just one day.
Artificial hydration and nutritionA gastrostomy tube was used for feeding 3 patients, either at the request of the patient or the family. In one patient a nasogastric tube provided hydration, upon consent of the patient and family after being informed about its metabolic effects during the end-of-life phase. Nasogastric or gastrostomy nutritional support was interrupted in 8 patients (n=6 and n=2, respectively).
DiscussionThe population forecast for 2010 based on the 2005 census was 7,363,782 inhabitants.20 The estimated implicit mortality rate for 2005â2010 was around 4.4/thousand inhabitants,21 taking into consideration other causes of mortality besides violence, neonatal and maternal mortality. The percentage of home care patients studied who paid from their own pockets from 2008 to 2012 was 0.19%, by just one private health care practitioner.
Most of the terminally ill patients receiving care were beyond the life expectancy age for the Colombian population; i.e., 73 years.22 However, patients range from adolescents to ninety year olds.
No studies have been made about the reasons why patients or their families ask for private home care or for patients wanting to receive this type of care until their demise. The results presented in this study show that most patients were females. On the other hand, the fact that the wife died meant that most of the patients were widowers. Another characteristic of the population was the level of education, mostly university graduates or at least high-school education. Most patients were Catholics, which is a critical aspect in the end-of-life approach. Knowing the religious or spiritual affiliation of patients and families helps for improved decision-making.23
Most of the patients in this cohort still need end-of-life care due to cancer illnesses; the broad range and the scope of cancer-related symptoms demand aggressive medical interventions for adequate management, in addition to the ârelativeâ ease for an objective and subjective acknowledgment of the fact that every possible therapeutic resource available has been exhausted to move to a purely palliative approach, within the framework of a society that mostly refuses to accept euthanasia or assisted suicide as an option. This distribution by diagnoses is similar to the hospice care offered in the United States.24
Secondly, there are some neurological pathologies with evident additional difficulties, since these patients are no longer self-sufficient, including their sound judgment for decision-making, so it is up to the family to decide if the patient has not previously expressed his/her will. The patient representative finds it hard to decide what their loved one would have liked, and he/she is even influenced by his/her own interests (taking advantage of the patient's pension or housing and even getting the attention of the rest of the family).
Care was mostly given at patient homes to avoid the ER or hospital admission, responding to the constantly changing needs of terminally ill patients for prompt relief. Such approach provides the proper environment and facilitates family decision-making in accordance with their realities and with adequate medical and professional information. It most be noted however that while most patients prefer to die at home, there is a group of patients and/or families who do not, and these differences shall be assertively managed.25
Hence it is desirable and recommendations have been made on the characteristics of palliative care programs where medical management should be the core, with nursing support, therapies and mental health, among other components.26 It is not recommended to require time-consuming formalities to include patients in the program, but rather to have programs that are more flexible and suitable for terminally ill patients instead of simply enrolling them in programs for patients with chronic conditions. It is cumbersome to transfer terminally ill patients to and from doctor offices to deal with each of their multiple symptoms, or to repeat the medical record to each specialist visiting the patient at home, with no continuity of the process, which in itself is quite complex and difficult.
The number of visits is an indicator of various factors; first, doing an intervention at the first visit is a sign of the urgency of end-of-life care. A second observation refers to a 24Ã7 hotline, for anticipating any events and keeping in mind a subcutaneous route as a rapid and effective approach for relieving symptoms. Thirdly, the presence of severe pain or any other symptoms as a source of direct stimulus, requires the use of analgesic doses to calm down the agonic patient so that the demise may occur a few hours or days later with no additional interventions required. Finally, when the patient expresses his/her final wishes to the family in a calm and friendly environment that moment becomes cathartic to relief tensions and reduce the anxiety of the final process.
In terms of medicines used, the generalized availability of a moderately strong parenteral opiate at an affordable price such as tramadol that acts on the three types of pain makes it a convenient painkiller to relief pain, including cancer pain. Moreover, the tolerance to tramadol is excellent if antiemetic and laxative agents are anticipated, avoiding the very frequent psychotropic effects of non-synthetic opiates in bed-ridden patients.
The use of subcutaneous anti-ulcer agents such as a prophylactic measure in erosive GI tract diseases is key and prevents the occurrence of alarming symptoms such as GI tract bleeding.
Superficial sedation was used in almost three fourths of the patients cared for until their demise. This is a decision made by those patients with a strong family and social support network that favor pain relief rather than being fully aware till the end; they have been properly informed about what they should expect, they have sufficient economic and social resources to pay for the sedative that is expensive and some times difficult to find.
Certain considerations are involved in the decision to maintain or remove hydration or nutritional support when the oral rout is compromised. Just as nobody made the decision to change the route for accomplishing the same purpose, it was not as easy to decide the removal of the gastrostomy tube, the catheter or the intravenous line. These decisions are extremely sensitive and nothing should be imposed; however, make sure that all the relevant information is shared. This approach gives both patients and family some options to decide in an extremely difficult situation.27
Lastly, a few general observations: presently, medicine provides us with powerful therapeutic tools for managing physical symptoms. End-of-life myths and preconceptions for using drugs that may have side effects â shorten the life span â should be put aside. We must continue to make headway in encouraging the availability of essential medicines for managing terminally ill patients,28 and keep in mind that ultra-short acting benzodiazepines are safe and effective for superficial sedation of these patients.
Absolutely it is better to avoid treating end-of-life patients in a cruel, inhuman or degrading manner at all times, but mostly when death is imminent. Scientific compassion, avoiding forcing the nature of human existence of the patients we assist, is fundamental to guide palliative therapeutic processes.29
There is then a humanistic and scientific approach to the management of end-of-life care; it is however necessary to develop a legislative framework to protect our patients against any actions that are not consistent with such an approach and be able to legally demand proper care.
FundingNone.
Conflicts of interestThe author has no conflicts of interest to declare.
The author conveyed her sincere gratitude to Dr. Giancarlo Buitrago for his kind review.
Please cite this article as: Támara LM. Estudio de cohorte descriptivo de los pacientes terminales atendidos médicamente en su domicilio en Bogotá. 2008–2012. Rev Colomb Anestesiol. 2014;42:100–106.