To describe the epidemiology of post-traumatic acute respiratory distress syndrome.
MethodologyDescriptive observational study of patients with traumatic femoral shaft fracture requiring surgical management.
The variables included in the analysis were demographics, injury severity, treatment methods, and in-hospital outcomes. A descriptive multivariate analysis was performed in order to explore the factors associated with the development of Acute Respiratory Distress Syndrome (ARDS).
ResultsOf the 267 patients with femoral fractures, 86% were male patients with a mean age of 28.7 years and Injury Severity Score (ISS) of 12.7. The overall prevalence of ARDS was 8.6% while the prevalence among multiple trauma patients was 20%. Mortality was 7.5%. In the bivariate analysis, the variables associated with ARDS were the following: time between the trauma and hospital admission, ISS, contused lung, associated tibial fracture, urgent surgery requirement, and need for red blood cell transfusion. In the multivariate analysis, the associated variables were: blunt chest trauma, time elapsed until definitive fixation, and red blood cell transfusion during surgery.
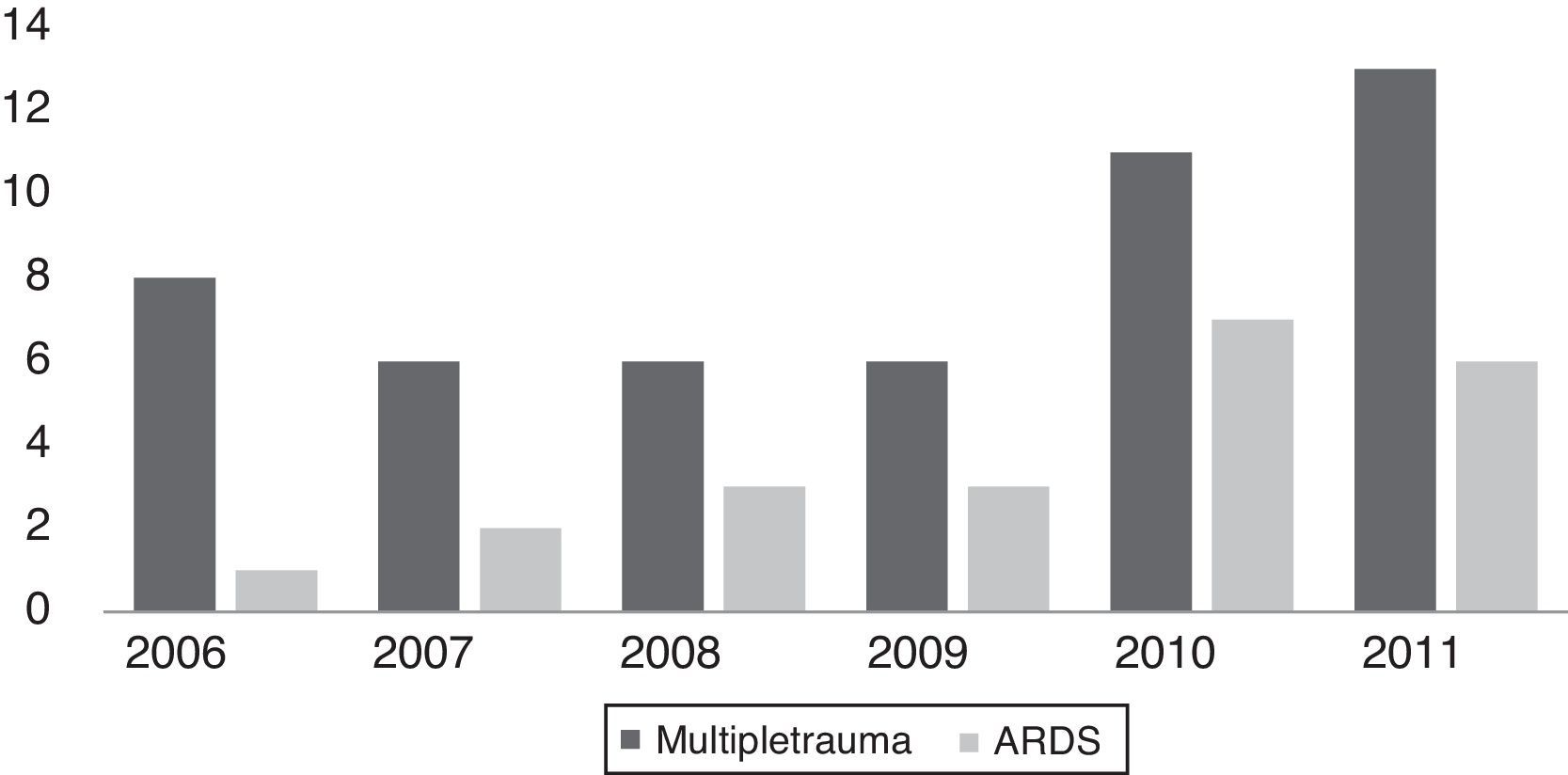
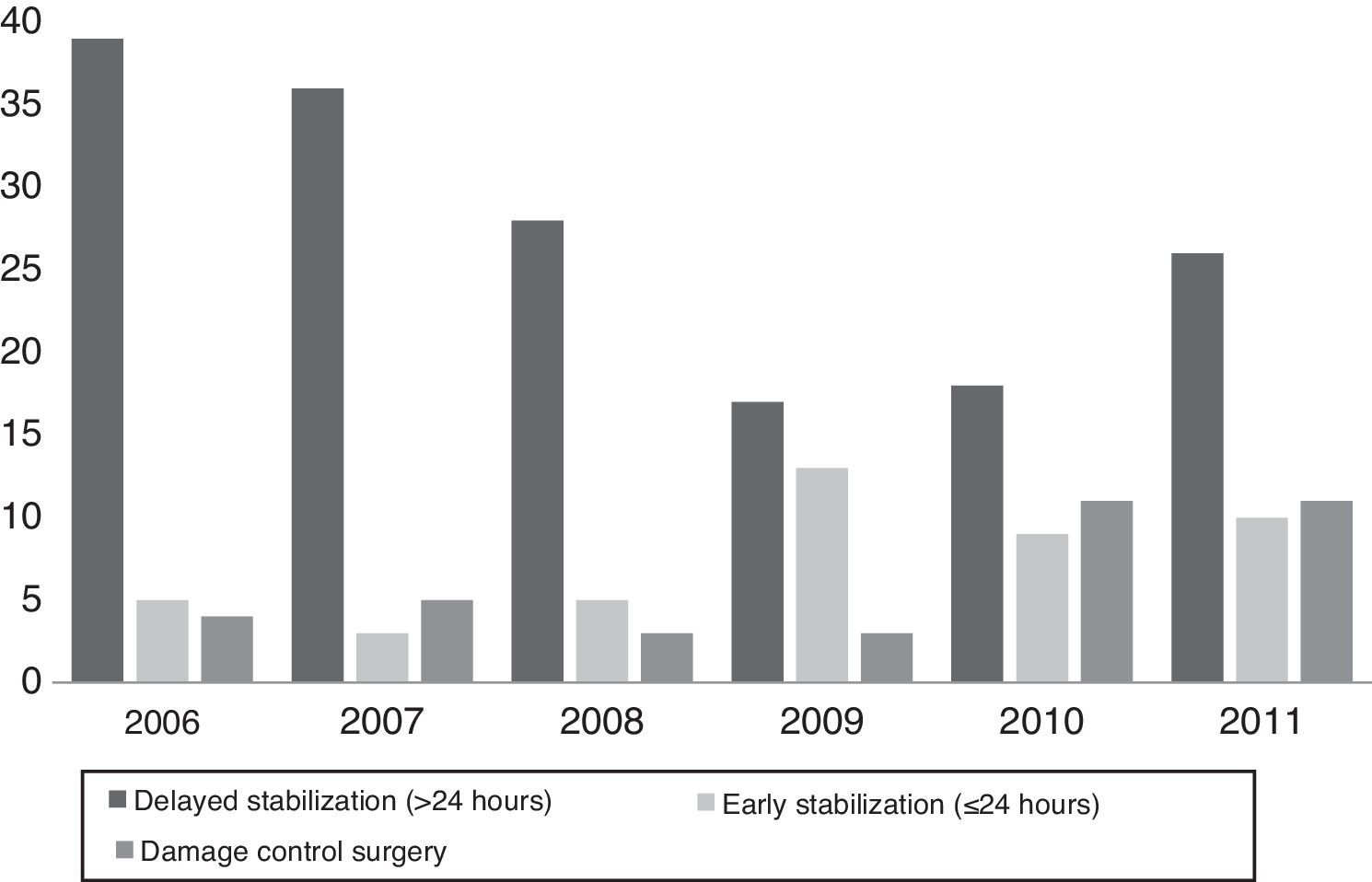
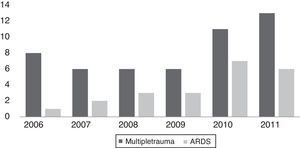
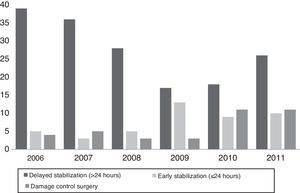
In the cohort, there was an increase in the annual prevalence of ARDS, from 4.3% in 2006 to 26.1% in 2011, as was also the case with multiple trauma, which increased from 14.5% in 2006 to 23.6% in 2011. A change in treatment was also evidenced, with increase in early total care (ETC) and damage control orthopaedics (DCO).
ConclusionsIn our population, the prevalence of ARDS in patients with femoral fractures increases when associated with blunt chest trauma, delayed stabilization time, and the need for blood transfusion.
Describir la epidemiología del síndrome de dificultad respiratoria aguda (SDRA) postraumático.
MetodologíaEstudio observacional descriptivo de pacientes con fractura traumática de la diáfisis femoral que requirieron manejo quirúrgico. Se analizaron variables demográficas, gravedad del trauma, métodos de tratamiento y desenlaces intrahospitalarios. Se realizó un análisis descriptivo y multivariado para explorar factores asociados al desarrollo de Síndrome de Dificultad Respiratoria Aguda (SDRA).
ResultadosDoscientos sesenta y siete pacientes con fractura femoral, el 86% fueron hombres con edad media de 28,7 años e Indice de Severidad del Trauma (ISS) de 12,7. Se observó una prevalencia de SDRA del 8,6%en toda la población y del 20% en politraumatizados. La mortalidad fue del 7,5%. Las variables asociadas al SDRA en el análisis bivariado fueron: tiempo entre el trauma y el ingreso, ISS, contusión pulmonar, fractura asociada de tibia, requerimiento de cirugía urgente y necesidad de transfusión de glóbulos rojos. En el análisis multivariado, las variables asociadas fueron: trauma contuso de tórax, tiempo transcurrido hasta la fijación definitiva y la transfusión de glóbulos rojos en cirugía. En la cohorte hubo un incremento en la prevalencia de SDRA anual, siendo del 4,3% en 2006comparado con el 26,1% en 2011, al igual que el politrauma que pasó del 14,5% en 2006 al 23,6% en 2011. Se evidenció también un cambio en el tratamiento, aumentando el control temprano total y el control de daño ortopédico.
ConclusionesEn nuestra población, la prevalencia de SDRA en pacientes con fracturas de fémur aumenta cuando hay trauma contuso de tórax, cuando se prolonga el tiempo de fijación y la transfusión sanguínea.
The acute respiratory distress syndrome (ARDS) is a rapidly progressing disorder with clinical manifestations than include dyspnoea, tachypnea and hypoxaemia. In up to 43% of the cases it may evolve to respiratory failure, multiple organ failure (MOF) and death, affecting medical as well as surgical patients.1 Muscle-skeletal trauma has been associated with post-traumatic ARDS, femoral shaft fractures having been shown to be more frequently associated with lung complications.2
White described a 0.5% prevalence of ARDS in trauma patients, with an increase to up to 10.2% in multiple trauma patients in the same cohort.3 In a study of risk factors associated with ARDS development in multiple trauma patients, Navarrete-Navarro found, after a multivariate analysis, that the presence of a femoral fracture was an independent risk factor for the development of ARDS, with an OR of 3.16 (95% CI 1.41–7.03), just like an APACHE II score and the use of blood transfusion during resuscitation.4
The strategy for treating femoral fractures associated with multiple traumas has been a topic of discussion in the orthopaedic literature over the past decade. In a clinical trial in the late 1980s, Bone showed that early fracture stabilization (<24h) reduced lung complications from 38% (delayed stabilization group) to 4% (early stabilization group), leading to the recommendation of early fixation.5 However, some studies were published in the 1990s linking multiple trauma and total early fixation with the onset of the systemic inflammatory response syndrome (SIRS), ARDS and multiple organ failure (MOF).6,7 This gave rise to questions regarding the method and the timing of bone stabilization and whether they played a role in the onset of lung complications.6,8 Pape et al. described a “borderline” group of patients who would not benefit from early total care (ETC). It was constituted by patients with severe multiple trauma, chest trauma with an abbreviated injury score (AIS)>2 and alteration of other systemic variables that increased their susceptibility to SIRS and pulmonary complications. It was based on these findings that the double-hit theory and damage control orthopaedics (DCO) were popularized.9–11 At present, there is a clinical trial already in the data collection phase, designed to determine which is the most effective strategy; in the meantime, however, we have no strong evidence in favour of either treatment.12
DCO is a management strategy that seeks to contain and stabilize orthopaedic injuries until the physiological condition of the patient improves and definitive bone stabilization is possible. The strategy consists of controlling haemorrhage, managing the soft tissues and providing temporary fracture stabilization by means of minimally invasive techniques, usually external fixation, in order to avoid worsening of the inflammatory response caused by the initial trauma (first hit) as a result of the surgery (second hit), and of the patient's condition.13 This concept has been a matter for debate among trauma surgeons, and multiple retrospective series have not been able to demonstrate that damage control orthopaedics offers any relevant clinical benefit for “borderline” patients.13 On the contrary, it would appear that this strategy delays final stabilization, increasing costs, length of stay in critical care units, and overall hospital stay.14
Pape's recommendations were adopted in Hospital Pablo Tobón Uribe, and temporary external fixation in multiple trauma patients became the most widely utilized strategy – although undocumented – and even overused in multiple trauma patients and femoral fractures with clinical criteria of stability in whom the world trend is to perform early total stabilization with intramedullary nails. Bearing in mind that Hospital Pablo Tobón Uribe has become the referral centre for multiple trauma patients, and considering that surgical treatment has not been standardized and there is great variability in care depending on undocumented factors, with this study we want to assess: the prevalence of ARDS in patients with isolated femoral shaft fracture or femoral shaft fracture associated with multiple trauma; describe the demographic profile of this population; evaluate factors mentioned in the literature that could be associated with ARDS; evaluate the differences betweens the methods used at Hospital Pablo Tobón Uribe for the treatment of femoral shaft fractures; and evaluate their effect on the prevalence of ARDS by treatment group.
MethodologyType of studyObservational descriptive study that evaluated all hospital admissions due to femoral shaft fractures at Hospital Pablo Tobón Uribe between January 1st, 2006 and July 31st, 2012.
Inclusion criteriaAdult patients 16–65 years of age with traumatic acute (first 24h) femoral shaft fractures according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) 32A1 a 32C3 classification,15 requiring surgical management, seen directly or by referral to Hospital Pablo Tobón Uribe, and who had not received any surgical treatment for the fracture in another institution.
Exclusion criteriaPatients with isolated distal femur or hip fractures, death within the first 24h of injury, pathological fractures, re-interventions due to non-union or osteomyelitis, and who had not received surgical treatment during hospitalization.
The project was approved by the Ethics Committee of the Hospital Pablo Tobón Uribe, and was a no risk study in accordance with Article 11 of Resolution 8430 of 1993.
Data collection and variablesAll admissions to Hospital Pablo Tobón Uribe during the period mentioned above with the CIE-10 diagnosis code S72 were evaluated. The data collection form was designed by the investigators based on experience and a review of the literature, and included the following: demographic variables (age, gender, comorbidities and presence of underlying lung/cardiac pathology); pattern of injury (mechanism of injury, time between trauma and admission, Glasgow Coma Scale, abbreviated injury severity score (AIS), injury severity score (ISS), multiple trauma defined as an ISS equal or greater than 16); associated fractures using the AO femoral fracture classification, and the Gustilo and Anderson classification for open fractures; clinical parameters such as vital signs on admission; type of initial bone stabilization; time between admission and initial stabilization; urgent surgery requirement; non-orthopaedic associated injuries; blood product transfusions within the first 24h; time until definitive surgery; and definitive treatment strategy. Outcomes were defined as follows: ARDS according to the Berlin criteria, including the time criterion of “before one week from the known trigger event”; radiographic findings such as bilateral opacities not explained by fluid overload, pleural effusion, atelectasis or nodules, and not completely explained by heart failure or fluid overload, with an objective assessment to rule out hydrostatic oedema (e.g. echocardiography); ARDS severity defined as mild with a PAFI<PaO2/FIO2≤300mmHg with PEEP or CPAP≥5cmH2O, as moderate with a PAFI<200mmHg, and severe with PaO2/FIO2≤100mmHg and PEEP≥5cmH2O16; admission and length of stay in the critical care unit (CCU); ventilator support requirement; hospital length of stay; and mortality.
Statistical analysisSize of the sample: The study included a fixed collected population of 368 patients, 267 of whom met the study criteria. With these number of patients and an expected proportion of 10% ARDS as outcome, 3–6 independent variables would be allowed according to the Harrell criteria. A descriptive statistical analysis was performed using means and medians with standard deviations, according to data distribution, for the quantitative variables, and proportions and relative frequencies for the qualitative variables. Differences between groups were calculated by means of the Chi-square or the Fisher's test for qualitative variables, and a Student's t test for the quantitative variables. Finally, the STAT 12.1 (R) was used to perform the multivariate analysis in order to determine the true relationship with the result, adjusting for confounding factors; a p value of less than 0.05 was accepted as statistically significant.
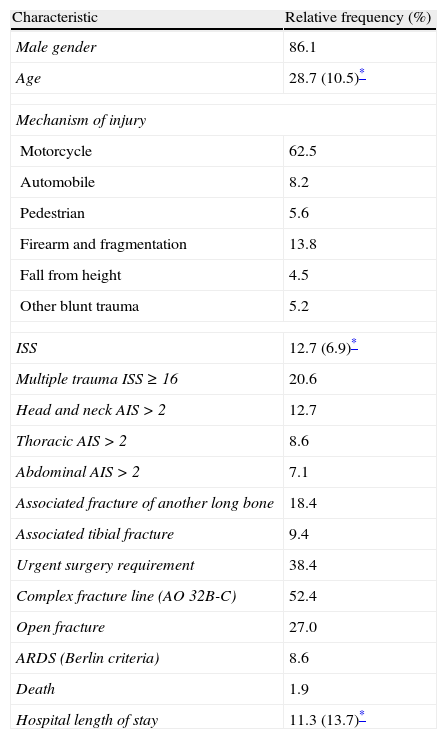
ResultsOverall, 383 patients with femoral fractures were admitted to Hospital Pablo Tobón Uribe between January 2006 and July 2012. Of them, 267 met the inclusion criteria; 86% were male patients with a mean age of 28.7 years (SD 10.5), and the average ISS was 12.7. Motorcycle accidents were the predominant mechanism of injury (62.5%), followed by gunshot wounds, falls from heights, and automobile accidents. Seven patients had some form of pulmonary comorbidity (5 had asthma and 2 had chronic obstructive pulmonary disease); none of these patients developed ARDS.
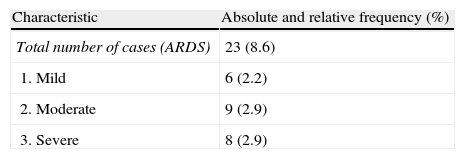
The most frequently associated long bone fracture was tibial fracture (9.4%), mostly ipsilateral (floating knee), while bilateral femoral fractures were found in 2.2% of the cases. The most common type of femoral fracture was AO 32A 130 (47.4%) and 27% were open fractures (Table 1). Fifty-five multiple trauma (ISS≥16) patients were observed (20.6%). The prevalence of ARDS for the total population was 8.6%, and 20% in multiple trauma patients. Overall mortality was 1.9%, and ARDS-associated mortality was 8.7%. Table 2 shows ARDS classification in the study population according to the Berlin criteria.
Demographic and trauma characteristics in patients with femoral shaft fractures HPTU 2006–2012 (N=267).
| Characteristic | Relative frequency (%) |
| Male gender | 86.1 |
| Age | 28.7 (10.5)* |
| Mechanism of injury | |
| Motorcycle | 62.5 |
| Automobile | 8.2 |
| Pedestrian | 5.6 |
| Firearm and fragmentation | 13.8 |
| Fall from height | 4.5 |
| Other blunt trauma | 5.2 |
| ISS | 12.7 (6.9)* |
| Multiple trauma ISS≥16 | 20.6 |
| Head and neck AIS>2 | 12.7 |
| Thoracic AIS>2 | 8.6 |
| Abdominal AIS>2 | 7.1 |
| Associated fracture of another long bone | 18.4 |
| Associated tibial fracture | 9.4 |
| Urgent surgery requirement | 38.4 |
| Complex fracture line (AO 32B-C) | 52.4 |
| Open fracture | 27.0 |
| ARDS (Berlin criteria) | 8.6 |
| Death | 1.9 |
| Hospital length of stay | 11.3 (13.7)* |
Study data.
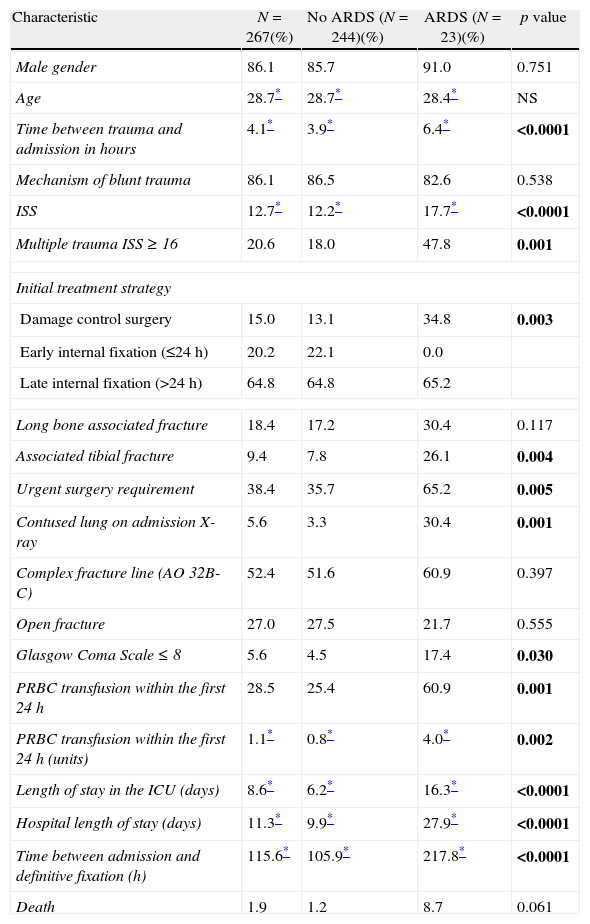
Table 3 shows the characteristics on admission and factors associated with ARDS development. There were no statistically significant differences found for the variables of age, gender, blunt trauma and systolic blood pressure on admission. In contrast, the univariate analysis showed statistically significant associations with time between trauma and admission in hours, ISS, presence of a contused lung on admission, associated tibial fracture, urgent surgery requirement, and the need for red blood cell transfusion on admission. The length of stay in the ICU and total hospital stay in days were longer for patients who developed ARDS (16.3 vs. 6.2 and 27.9 vs. 9.9, respectively).
Comparison of patients with and without ARDS between admission characteristics and factors associated with ARDS development.
| Characteristic | N=267(%) | No ARDS (N=244)(%) | ARDS (N=23)(%) | p value |
| Male gender | 86.1 | 85.7 | 91.0 | 0.751 |
| Age | 28.7* | 28.7* | 28.4* | NS |
| Time between trauma and admission in hours | 4.1* | 3.9* | 6.4* | <0.0001 |
| Mechanism of blunt trauma | 86.1 | 86.5 | 82.6 | 0.538 |
| ISS | 12.7* | 12.2* | 17.7* | <0.0001 |
| Multiple trauma ISS≥16 | 20.6 | 18.0 | 47.8 | 0.001 |
| Initial treatment strategy | ||||
| Damage control surgery | 15.0 | 13.1 | 34.8 | 0.003 |
| Early internal fixation (≤24h) | 20.2 | 22.1 | 0.0 | |
| Late internal fixation (>24h) | 64.8 | 64.8 | 65.2 | |
| Long bone associated fracture | 18.4 | 17.2 | 30.4 | 0.117 |
| Associated tibial fracture | 9.4 | 7.8 | 26.1 | 0.004 |
| Urgent surgery requirement | 38.4 | 35.7 | 65.2 | 0.005 |
| Contused lung on admission X-ray | 5.6 | 3.3 | 30.4 | 0.001 |
| Complex fracture line (AO 32B-C) | 52.4 | 51.6 | 60.9 | 0.397 |
| Open fracture | 27.0 | 27.5 | 21.7 | 0.555 |
| Glasgow Coma Scale≤8 | 5.6 | 4.5 | 17.4 | 0.030 |
| PRBC transfusion within the first 24h | 28.5 | 25.4 | 60.9 | 0.001 |
| PRBC transfusion within the first 24h (units) | 1.1* | 0.8* | 4.0* | 0.002 |
| Length of stay in the ICU (days) | 8.6* | 6.2* | 16.3* | <0.0001 |
| Hospital length of stay (days) | 11.3* | 9.9* | 27.9* | <0.0001 |
| Time between admission and definitive fixation (h) | 115.6* | 105.9* | 217.8* | <0.0001 |
| Death | 1.9 | 1.2 | 8.7 | 0.061 |
Study data.
PRBC: packed red blood cells; ICU: intensive care unit.
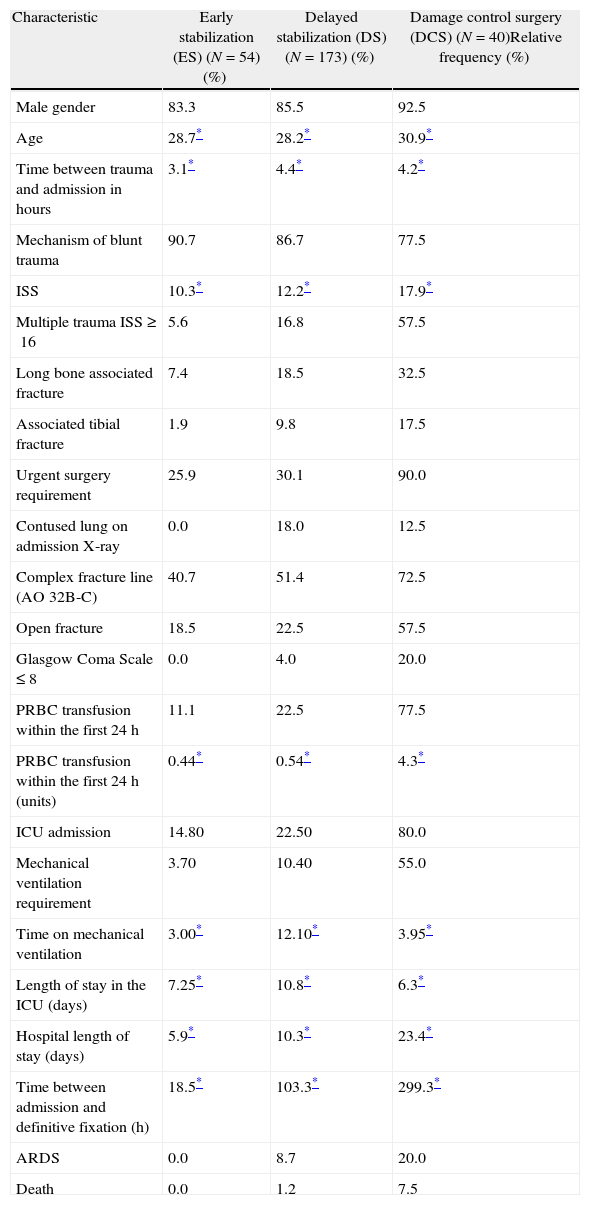
Table 4 shows variable analysis according to the treatment strategy selected for the femoral fracture: of the 267 patients, 54 (20.2%) were taken to definitive stabilization within the first 24h (ETC), 173 (64.8%) were taken to delayed stabilization (DS) with a mean of 4.3 days between admission until definitive stabilization; 40 (15%) were initially treated with the DCO strategy and this group had a mean ISS of 17.9 compared with the early fixation3,10 and delayed fixation2,12 groups. Of the patients undergoing DCO, 57.5% were multiple trauma patients (ISS≥16), 90% required transfer to urgent surgery, 80% were admitted to the ICU, and 20% developed ARDS. Of the patients in the DCO group, 55% required mechanical ventilation compared to DS (10.4%) and ETC (3.7%).
Characteristics on admission and outcomes according to the selected treatment strategy for the femoral fracture.
| Characteristic | Early stabilization (ES) (N=54) (%) | Delayed stabilization (DS) (N=173) (%) | Damage control surgery (DCS) (N=40)Relative frequency (%) |
| Male gender | 83.3 | 85.5 | 92.5 |
| Age | 28.7* | 28.2* | 30.9* |
| Time between trauma and admission in hours | 3.1* | 4.4* | 4.2* |
| Mechanism of blunt trauma | 90.7 | 86.7 | 77.5 |
| ISS | 10.3* | 12.2* | 17.9* |
| Multiple trauma ISS≥16 | 5.6 | 16.8 | 57.5 |
| Long bone associated fracture | 7.4 | 18.5 | 32.5 |
| Associated tibial fracture | 1.9 | 9.8 | 17.5 |
| Urgent surgery requirement | 25.9 | 30.1 | 90.0 |
| Contused lung on admission X-ray | 0.0 | 18.0 | 12.5 |
| Complex fracture line (AO 32B-C) | 40.7 | 51.4 | 72.5 |
| Open fracture | 18.5 | 22.5 | 57.5 |
| Glasgow Coma Scale≤8 | 0.0 | 4.0 | 20.0 |
| PRBC transfusion within the first 24h | 11.1 | 22.5 | 77.5 |
| PRBC transfusion within the first 24h (units) | 0.44* | 0.54* | 4.3* |
| ICU admission | 14.80 | 22.50 | 80.0 |
| Mechanical ventilation requirement | 3.70 | 10.40 | 55.0 |
| Time on mechanical ventilation | 3.00* | 12.10* | 3.95* |
| Length of stay in the ICU (days) | 7.25* | 10.8* | 6.3* |
| Hospital length of stay (days) | 5.9* | 10.3* | 23.4* |
| Time between admission and definitive fixation (h) | 18.5* | 103.3* | 299.3* |
| ARDS | 0.0 | 8.7 | 20.0 |
| Death | 0.0 | 1.2 | 7.5 |
Study data.
PRBC: packed red blood cells; ICU: intensive care unit.
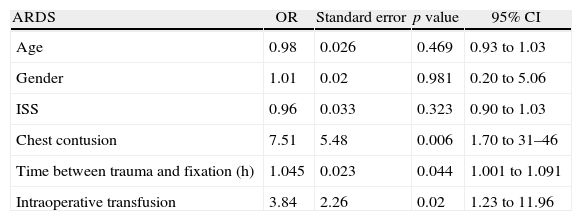
When the binary logistic regression was done as part of the multivariate analysis, the only variables associated with ARDS development in patients with femoral fractures were blunt trauma to the chest, timing of fixation (time between trauma and fracture stabilization), and red blood cell transfusion during surgery (Table 5).
Result of the binary logistic regression.
| ARDS | OR | Standard error | p value | 95% CI |
| Age | 0.98 | 0.026 | 0.469 | 0.93 to 1.03 |
| Gender | 1.01 | 0.02 | 0.981 | 0.20 to 5.06 |
| ISS | 0.96 | 0.033 | 0.323 | 0.90 to 1.03 |
| Chest contusion | 7.51 | 5.48 | 0.006 | 1.70 to 31–46 |
| Time between trauma and fixation (h) | 1.045 | 0.023 | 0.044 | 1.001 to 1.091 |
| Intraoperative transfusion | 3.84 | 2.26 | 0.02 | 1.23 to 11.96 |
Study data.
Fig. 1 shows the prevalence of multiple trauma and ARDS per year. Dividing this historical cohort into two periods before and after 2010, a trend is observed in the number of multiple trauma patients seen and ARDS.
Fig. 2 shows the change in treatment strategy during the study period. As multiple trauma increase there is also an increased trend towards performing DCO.
DiscussionARDS is a frequent complication than may occur in medical as well as trauma patients. In the latter, it is associated with high-energy injury and multiple trauma, with mortality ranging between 40% and 60%.1,17
In general trauma, a prevalence of 0.5% has been described, and this value increases to 10.2% when associated with multiple trauma (defined as >3 injured systems).3,18 Femoral shaft fracture has been cited frequently as one of the potential causes of the inflammatory response that could trigger ARDS. In this study, we found a prevalence of ARDS of 8.6% in patients with femoral fracture.
The prevalence of ARDS among multiple trauma patients was 20.6%, higher than what was found by White (3.1%)3 and by Hoyt (12%).19 As far as we are aware, this is the first study that tries to determine the prevalence of ARDS in patients with femoral fracture using the new Berlin criteria, finding a higher frequency of moderate and severe ARDS associated with a mean ISS of 22 and multiple trauma in 92% of the cases.
No differences were found in terms of age and gender in the patients that developed ARDS, compared to those that did not. In their paper, Croce et al.20 propose that early onset of ARDS (<48h from the time of trauma) occurs in the younger population and has longer survival than late ARDS (>48h), with no changes on final mortality. However, that difference was not found in this study. It was found that the increase in the time period between trauma and admission to the hospital, the presence of multiple trauma, associated contused lung on admission, moderate lung injury (AIS>2), associated tibial fracture, and the need for blood transfusion within the first 24h were associated with the presence of ARDS, as has been shown by other studies.4,21–23 However, the same was not true for variables such as head trauma (except according to the Glasgow Coma Scale), fracture complexity and presence of hypotension at the time of admission, which had been reported classically as risk factors for the development of ARDS.3,19,22
Mortality associated with ARDS in femoral fractures was 8.7%. This result is lower than what has been reported in the literature (40–60%), but it is similar to that reported by Zambon et al., who show a 1.1% annual reduction in mortality over the past 15 years, probably associated with early diagnosis thanks to the criteria defined since the ARDS consensus 1994,24 a better understanding of the disorder, and the treatment strategies.25–27
There has been a discussion in the literature about the best treatment strategy for multiple trauma patients, ranging from delayed stabilization at the end of the last century, total early stabilization – with the advantage of reducing lung complications as shown in different studies and meta-analyses28–32 – to damage control orthopaedic surgery. Regarding this latter strategy, an interesting debate has emerged over the past few years following the work by Nicholas,33 who compared his study with a clinical trial conducted by Pape et al. and found that despite not having used the DCO strategy in the cases suggested by Pape – “borderline” patients – there were no statistically significant differences in terms of pulmonary complications; instead, there was an increase in ICU lengths of stay and the number of days on mechanical ventilation when compared to the study by Pape et al.14,34 In our population, it was found that patients who underwent DCO had more severe forms of trauma (multiple trauma 55.7%; shock at the time of admission 20%), 80% were taken to the ICU, and 55% required mechanical ventilation; 20% developed ARDS and 7.5% died. In spite of this, when compared to other ETC and DS groups, it was found that those who underwent DCO remained less time on mechanical ventilation compared to the group with delayed stabilization (DCO: 3.95; ETS: 3.0; DS: 12.1 days) and shorter length of stay in the ICU (DCO: 6.3; ETS: 7.25; DS: 10.8 days); but a longer overall stay (DCO: 23.4; ETS: 5.9; DS: 10.3 days). These results are in contrast with those of Balogh and similar to those described by Pape, although because of the characteristics described above, it is highly probable that our patients taken to DCO were more “unstable” than “borderline”.14,33
As has been mentioned, the recommendations by Pape et al. have been embraced at Hospital Pablo Tobón Uribe, and this is reflected in a more frequent use of ETS and DCO treatment strategies, with less delayed fracture fixation over the past few years. This management strategy may explain why there were lower rates for ventilation, ICU stay and mortality.
The limitations of the study have to do with its retrospective and descriptive nature and loss of data. Although data were complete for outcome variables, it was not possible to homogenize clinical and paraclinical variables in order to compare our results based on the classification of stable, unstable, borderline or extremis patients. The strength of the study is that the presence of ARDS was evaluated in accordance with the 2012 Berlin consensus that uses maximum time of onset, eliminates acute lung injury (ALI) and specifies the radiographic assessment of the syndrome, with guidelines as to which disorders should be ruled out as confounding factors (fluid overload and pulmonary oedema, among others).
FundingsNone.
Conflict of interestsNone.
We thank the Hospital Pablo Tobón Uribe for its support for this work, Connie Arboleda Velásquez for her help with the methodology, and Orthopaedics and Traumatology Residents from Universidad Pontificia Bolivariana Juan Felipe Ramírez, Juan Esteban Mejía and Jorge Hincapié for their assistance.
Please cite this article as: Cardona A JM, Valderrama CO, Gaviria UJ, Arboleda VC, Ramirez NG. Caracterización clínica y epidemiológica del síndrome de dificultad respiratorio aguda en pacientes adultos con fractura diafisiaria de fémur. Rev Colomb Anestesiol. 2014;42:176–183.