Rett Syndrome (RS) is a neurological disorder that almost exclusively affects females. RS is characterized by severe mental retardation following a period of apparent normal development in early childhood. The main clinical features include autism, spasticity, microcephaly, scoliosis, stereotyping, abnormal respiratory control and seizures. Patients with RS have been reported to be extremely sensitive to sedatives and exhibit a slow recovery from anesthesia. We describe and discuss the anesthetic management of a 26-year-old woman with RS and distal fracture of the humerus that underwent reduction and fixation with Kirschner's wires under regional anesthesia and sedation. Intraoperatively, the patient experienced respiratory depression following the administration of 1mg of I.V. midazolam. Our experience in this case led us to conclude and suggest that benzodiazepines should not be used in RS and in the absence of contraindications the technique of choice should be regional anesthesia.
El síndrome de Rett (SR) es un trastorno neurológico que afecta principalmente a las mujeres. Se caracteriza por un retraso mental severo después de un periodo de desarrollo aparentemente normal en la infancia temprana. Las principales características incluyen autismo, espasticidad, microcefalia, escoliosis, estereotipias, control anormal de la respiración y convulsiones. Se ha notificado que son muy sensibles a sedantes y tienen una lenta recuperación luego de una anestesia. Nosotros describimos y discutimos el manejo anestésico de una mujer de 26 años con SR y fractura distal del húmero, tratada con reducción y fijación con agujas de Kirschner bajo anestesia regional y sedación; quien tuvo depresión respiratoria luego de administrar 1 mg de midazolam i.v. intraoperatorio. Nuestra experiencia con este caso nos hace concluir y sugerir que no se deben usar benzodiacepinas en SR, y si no existe contraindicación, la anestesia regional es la técnica de elección.
RS is a neurologic pediatric disorder mainly affecting girls of all races. It has a prevalence of 0.5 per 10,000 inhabitants, the diagnosis is clinical and around 70–80% of the syndrome's clinical phenotype shows mutations in the MECP2 gene localized in the distal portion of chromosome X.1
RS was described in 1966 by Andreas Rett and is characterized by a progressive neurological impairment of the central nervous system (CNS) that presents in early childhood and is characterized by a delay in achieving the typical psychomotor skills of children in the same age group, loss of acquired skills and the onset of an autistic condition including automatisms, seizures and mental retardation. Other common characteristics to this etiology are the presence of choreoathetosis, myoclonus, stereotypes, scoliosis, hyperventilation in the awake state – apnea episodes, decreased food intake with secondary muscle mass loss and sudden death.2,3
This is a challenging group of patients for the anesthesiologist because they may be faced with a difficult airway and/or spontaneous and anesthesia-triggered episodes of apnea and hypoxemia,2,4 such as the clinical case herein reported. The case describes the low threshold to certain drugs such as low-dose I.V. midazolam among this group of patients.
Clinical case26-year-old woman was diagnosed with Rett Syndrome who was admitted to the trauma unit of the Ramón y Cajal University Hospital in Madrid, Spain. The patient presented with a displaced fracture of the distal third of the right humerus. After a failed orthopedic reduction in the ER the patient was scheduled for open reduction and surgical fixation. The patient's history included: epileptic crises while receiving carbamazepine treatment until 2005 and surgical correction of dorso-lumbar scoliosis in 1998, with no prior record of anesthetic complications.
The following difficult airway predictors were identified during the pre-anesthetic evaluation5: Mallampati III, micrognatia, class III bite test and limited cervical flexion – extension. Complementary testing showed first grade atrial-ventricular block.
The patient came to the OR awake with BP 125/80mmHg, HR 85lpm, RR 15bpm and SpO2 96% with FiO2 21%. The patient was pre-medicated with 1mg of midazolam I.V. in addition to complementary oxygen. We then performed a neurostimulator-guided infraclavicular sub-coracoid brachial plexus block with 40ml of 1.5% mepivacaine. The surgical procedure consisted of reduction and Kirschner wires osteosynthesis.
During the intraoperative period 1mg of midazolam I.V. was administered for agitation, with subsequent respiratory depression down to SpO2 60%, which rose quickly with positive pressure ventilation with facemask, with no new episodes of respiratory depression and/or oxygen desaturation. The postoperative continued to evolve uneventfully at the Intensive Care Unit (ICU).
DiscussionAlthough RS prevalence is low, we must become familiar with any issues that may arise in the operating theater or the ICU with these patients, considering the neurological, respiratory, cardiovascular and metabolic characteristics of this disorder as we shall discuss in this paper.
These patients come for neuroimaging studies and surgical procedures such as gastrostomy or scoliosis correction (present in 50% of these cases) and may experience problems as Jung T. Kim had with a girl undergoing scoliosis surgery and despite having a BIS score within the optimum range, being normocapnic, with normal glycemic levels, normal temperature and hemodynamically stable, had a slow awakening and was extubated in the ICU 4h after the completion of surgery; this confirms one of the problems experienced by these patients, i.e. excessive sensitivity to volatile anesthetic agents and sedatives.6
Another important point and which is closely linked to an increased sensitivity to anesthetic drugs is pain control. It is difficult to determine the requirements for analgesia in this group of patients because they have an increased pain threshold from the high levels of β-endorphins found in the cerebrospinal fluid.2,4,7 As an example we could mention the case published by Konarzewski W.H. of a 3-year-old girl, premedicated with trimeprazine and ketamine for strabismus correction under general anesthesia with halothane and nitrous oxide. The patient had a delayed recovery of consciousness at the end of anesthesia4 that according to Dearlove O.R. was due to the interaction between ketamine and the endogenous morphine components.2
Konen A.A. described another case of elevated pain threshold in an adolescent girl undergoing scoliosis surgery.7 The first postoperative day she was administered a combination of epidural bupivacaine 0.1% plus hydromorphone 20mcg/ml at 4ml/h; however, the analgesia had to be stopped and replaced by perfused naloxone on the second day after surgery because the patient developed bradypnea and oxygen desaturation. The authors recommend using local anesthetic agents only and avoid opioids in this population.8
In addition to the increased sensitivity to anesthetic drugs and the increased pain threshold, several authors have found other issues in our anesthesiology practice: Dearlove O.R. in a series of 3 cases of scoliosis corrective surgery found that the patients had increased muscle tone and poor distal perfusion; one patient developed seizures that were difficult to control and another one experienced difficulties in removing the mechanical ventilation because of carbon dioxide retention and sputum. In yet another case, it was difficult to obtain a venous and arterial access.4
Maguirre D. described that during spinal fusion for scoliosis correction, the patient developed a temperature of 33.5°C, despite all the measures adopted to warm her up.8 The author recommends the adoption of aggressive measures for temperature control in these patients.
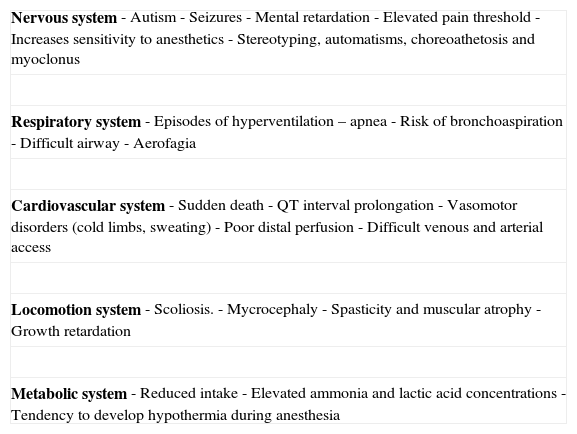
Other characteristics of these patients that are relevant for our professional practice are listed in Table 1: growth retardation, microcephaly,7 seizures, mental retardation, aerofagia, vasomotor disorders 3,8 (cold limbs or profuse sweating), QT interval prolongation2 (this may be one of the causes for sudden death), increased serum potassium with the administration of succinilcoline,8 difficulty to position the patient in the operating table because of atrophy and spasticity, risk of recurrent bronchoaspiration and functional respiratory impairment due to muscle weakness and thoracic deformity, abnormal respiratory pattern (regular and stable breathing while sleeping but with episodes of hyperventilation and apnea while being awake) that may lead to permanent hypoxic damage and contribute to a progressive cerebral impairment.7,8 Other findings of interest to this group are the existing metabolic disorders including elevated concentrations of ammonia and lactic acid and reduced dopamine, serotonin and norepinephrine levels.8
Important characteristics of Rett syndrome for the anesthesiologist.
| Nervous system- Autism- Seizures- Mental retardation- Elevated pain threshold- Increases sensitivity to anesthetics- Stereotyping, automatisms, choreoathetosis and myoclonus |
| Respiratory system- Episodes of hyperventilation – apnea- Risk of bronchoaspiration- Difficult airway- Aerofagia |
| Cardiovascular system- Sudden death- QT interval prolongation- Vasomotor disorders (cold limbs, sweating)- Poor distal perfusion- Difficult venous and arterial access |
| Locomotion system- Scoliosis.- Mycrocephaly- Spasticity and muscular atrophy- Growth retardation |
| Metabolic system- Reduced intake- Elevated ammonia and lactic acid concentrations- Tendency to develop hypothermia during anesthesia |
In our review we only found one published article of increased sensitivity to midazolam. In this case, 0.5mg/kg of oral midazolam were administered as premedication to a pediatric patient who was not operated on the day scheduled for surgery and who remained highly sedated to enable discharge 8h following the administration of benzodiazepine.9 In our case, premedication with 1mg of midazolam I.V. and the subsequent intraoperative administration of another 1mg I.V. (total accumulated dose of 2mg of I.V. midazolam) as complementary sedation to the nerve block resulted in respiratory depression and hypoxemia that required assisted ventilation.
Our experience with this particular case leads us to conclude and suggest that benzodiazepines should be avoided in these patients and unless there are any contraindications, regional anesthesia is the technique of choice. Likewise, we recommend that regardless of how simple the surgical intervention, postoperative follow-up should be implemented at the intermediate or critical care unit.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-Moreno JC, Nájera-Losada DC, Domínguez-Pérez F. Manejo anestésico de un paciente con síndrome de Rett y fractura distal de húmero: reporte de un caso y revisión de la literatura. Rev Colomb Anestesiol. 2014;42:57–59.