Ultrasonography as a diagnostic and therapeutic tool has greatly impacted the anesthesiologist's routine in multiple practical applications. However, only recently there have been some reports published in the literature on the use of ultrasonography for the management of the airway in the surgical and ICU patients. Being a portable, easy to use, non-invasive tool that does not require any ionizing energy, ultrasonography becomes highly attractive when the anesthesiologist faces practical issues in a difficult airway. The purpose of this review was precisely to show the potential uses of ultrasonography for difficult airway management, from the literature perspective.
There is enough trials-based evidence so far to recommend the use of ultrasonography for the following situations: identification of anatomical airway structures, static detection of a failed or esophageal intubation, dynamic airway measurements, and size determination of endotracheal tubes; identification of predictors of a difficult airway in patients with challenging necks, and trans-tracheal techniques to secure the airway.
Nevertheless, further studies with strong methodological quality are required to show the potential of ultrasonography to impact the difficult airway management and the morbidity and mortality associated with this condition.
La ecografía como herramienta diagnóstica y terapéutica ha tenido un gran impacto en el quehacer rutinario del anestesiólogo en múltiples áreas de aplicación práctica. Sin embargo, es hasta hace poco en donde han aparecido en la literatura reportes de su uso en situaciones que involucra el manejo de la vía área del paciente en cirugía y unidades de cuidados intensivos. Al ser esta una herramienta portable, fácil de usar, no invasiva y sin necesidad de energía ionizante, la hace altamente atractiva al momento de resolver preguntas prácticas del anestesiólogo que se ve enfrentado a una vía área difícil. Justamente el objetivo de esta revisión fue mostrar desde la literatura cuales son los potenciales usos de los ecografía en el manejo de la vía área.
Hasta el momento los estudios muestran suficientes elementos para recomendar su uso en los siguientes situaciones: identificación de estructuras anatómicas en la vía área; detección estática de intubación fallida o esofágica; mediciones dinámicas de la vía área y determinación del tamaño de tubos endotraqueales; predictores de vía área difícil en pacientes con cuello desfavorable; y técnicas transtraqueales para aseguramiento de la vía área.
A pesar de ello, aún se requieren mayores estudios con suficiente calidad metodológica en donde se demuestre que el uso de la ecografía si puede llegar a impactar en el manejo de la vía área difícil y en la morbimortalidad generada por esta entidad.
Airway management is one of the critical skills of the anesthesiologist. Close to 64% of the anesthesia-associated deaths are the result of airway management complications, both during induction and securing of the airway.1 Ultrasound is a portable, easy to use, noninvasive tool with high sensitivity rates than can be used in combination with other devises for proper perioperative airway management.2–4
This review discusses the role of ultrasound as an additional complementary tool in the management of the airway in different situations, including the identification of structures, detection of esophageal intubation, positioning of the endotracheal tube, proper size selection of the conventional and double-lumen endotracheal tube, determination of adequate face mask or supraglottic device ventilation, difficult airway predictors, predictors of risk of postextubation stridor, and ultrasound-guided translaryngeal techniques, including translaryngeal blocks, retrograde intubation and percutaneous tracheostomy.
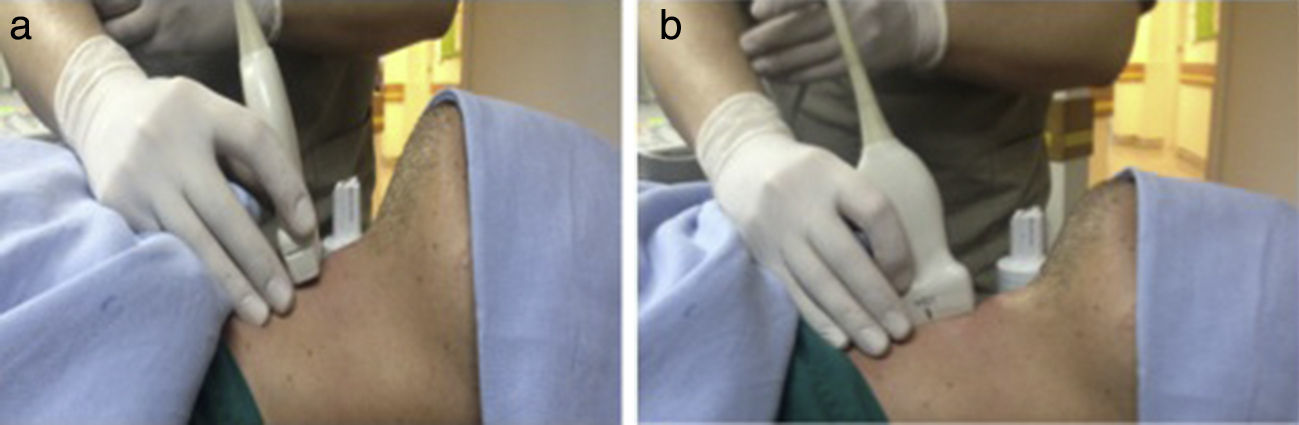
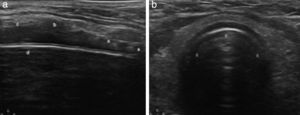
PreparationAdequate evaluation and ultrasound visualization of the airway requires the patient to be in a centered sniffing position.5 Since the structures to be visualized are superficial, most of the airway windows may be obtained using a 7.5-Mhz high-frequency lineal transducer. Remember to use a proper hydrosoluble gel for image optimization, eliminating the air interface, adjusting the equipment settings for superficial soft tissues, adjusting the depth to 3–4cm and the focus 1cm posterior to the structure to be visualized. If the target for visualization is the hyoid bone, an enhanced visualization may be achieved using the 5-Mhz convex transducer.
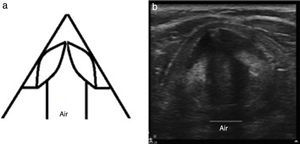
Ultrasound identification of airway structuresAir prevents the passage of ultrasound waves, generating hyper or hypo-echoic reverberation artifacts that hinder the visualization of deep structures but allows for easy identification of the airway since it is the only structure that produces comet tails, reverberations and acoustic shadowing.
The bone presents as a hyperechoic structure that produces an anechoic shadow; the main bone structure in the airway is the hyoid bone, but in over fifty percent of the patients it cannot be fully visualized.6
The tracheal cartilages are hyperechoic, as well as the cricothyroid membrane and the vocal cords.6
Furthermore, it is important to keep in mind that the mucosa/air interface looks hyperechoic, as for instance the interface below the cricothyroid membrane.
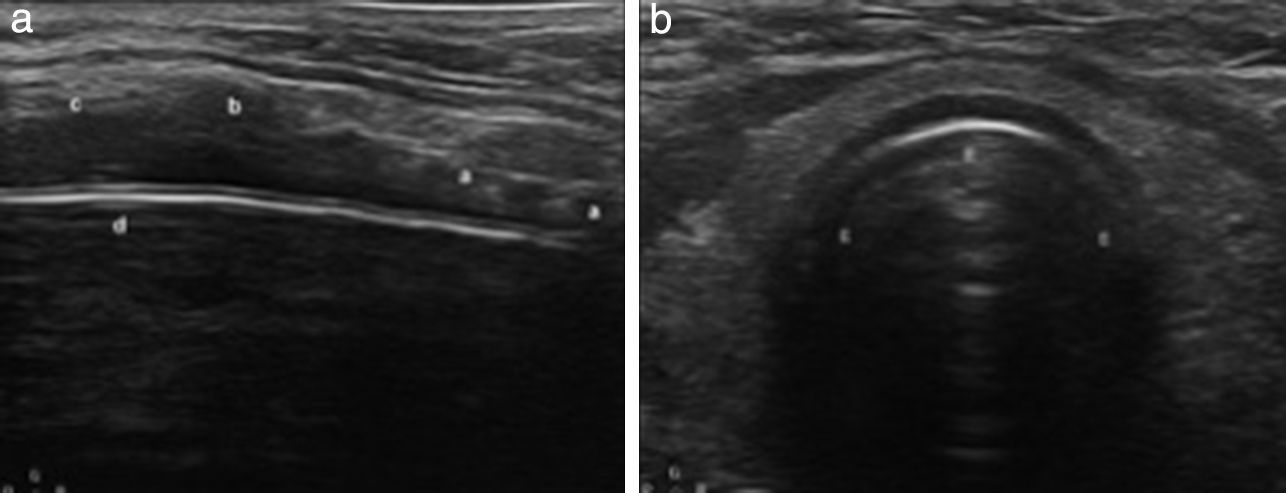
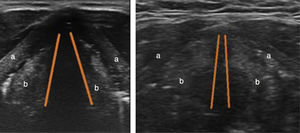
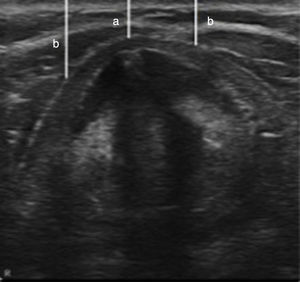
There are two ultrasonography approaches for the airway: the axial or short axis and the longitudinal or long axis (Fig. 1).Hyoid bone
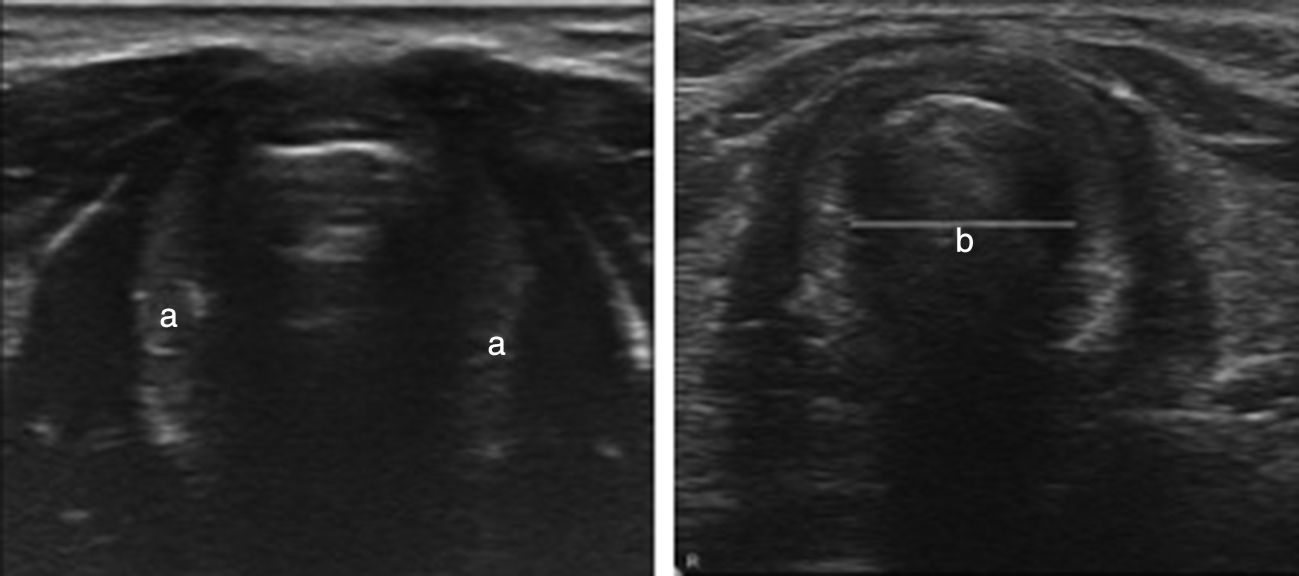
The identification of the hyoid bone may be from a transverse or longitudinal approach; it is a hyperechoic structure with a hypoechoic U-shape halo (Fig. 2); although there is no standard technique, successful cases have been reported of ultrasound-guided superior laryngeal nerve block at the horn of the hyoid bone.7Epiglottis
The epiglottis cross-section may be visualized with the high-frequency lineal transducer at the thyroid–hyoid space. It is characterized by a hypoechoic U-shape image preceded at its anterior margin by the pre-epiglottic space that is hyperechoic and relates posteriorly with the hyperechoic interface between the mucosa and the air7 (Fig. 3).Thyroid cartilage
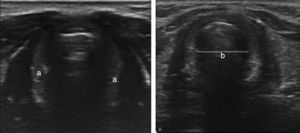
Is one of the best visualized structures described at the transverse axis as a hypoechoic structure with respect to the vocal cords, followed by an acoustic shadow corresponding to the airway (Fig. 4); on the sagittal plane, the thyroid–hyoid space and the acoustic shadow in the hyoid bone can be evaluated (Fig. 2).7,8 At this level, the vocal cords can be seen as hypoechoic structures. Pathological conditions such as the unilateral paralysis of the vocal cords may be identified at this level, when the patient is asked to emit a sound to see the vibration of the vocal cords – adduction and abduction of the vocal cords (Fig. 4).Cricoid cartilage
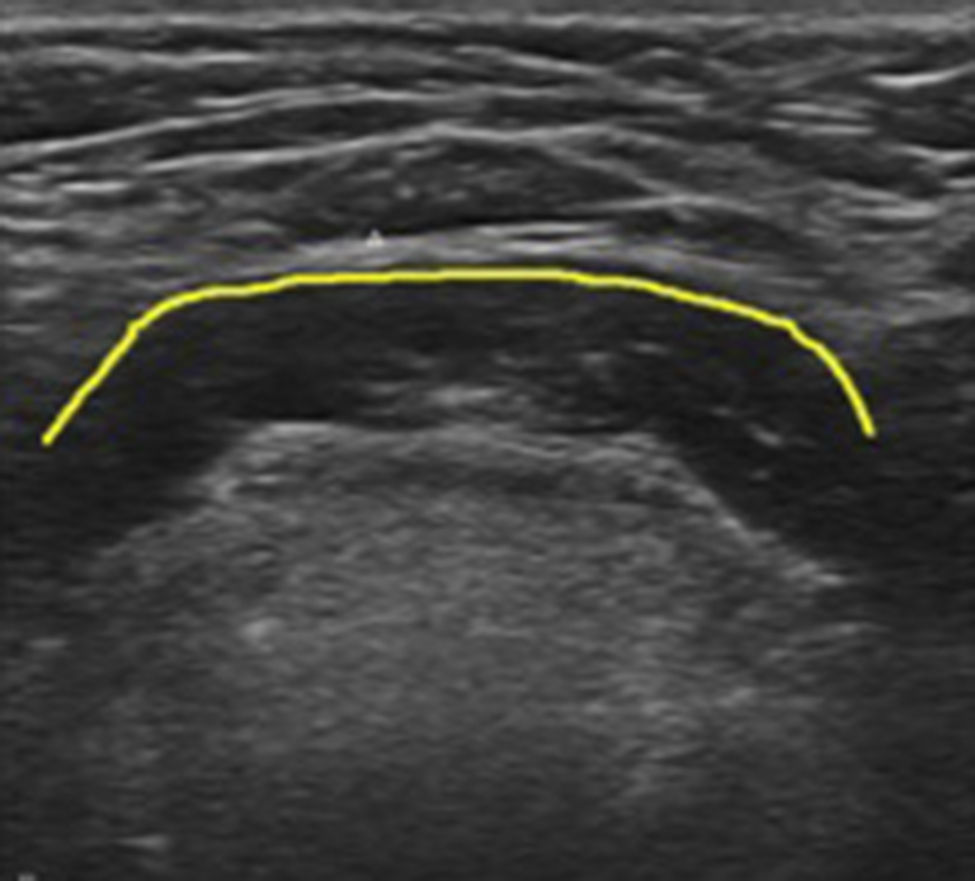
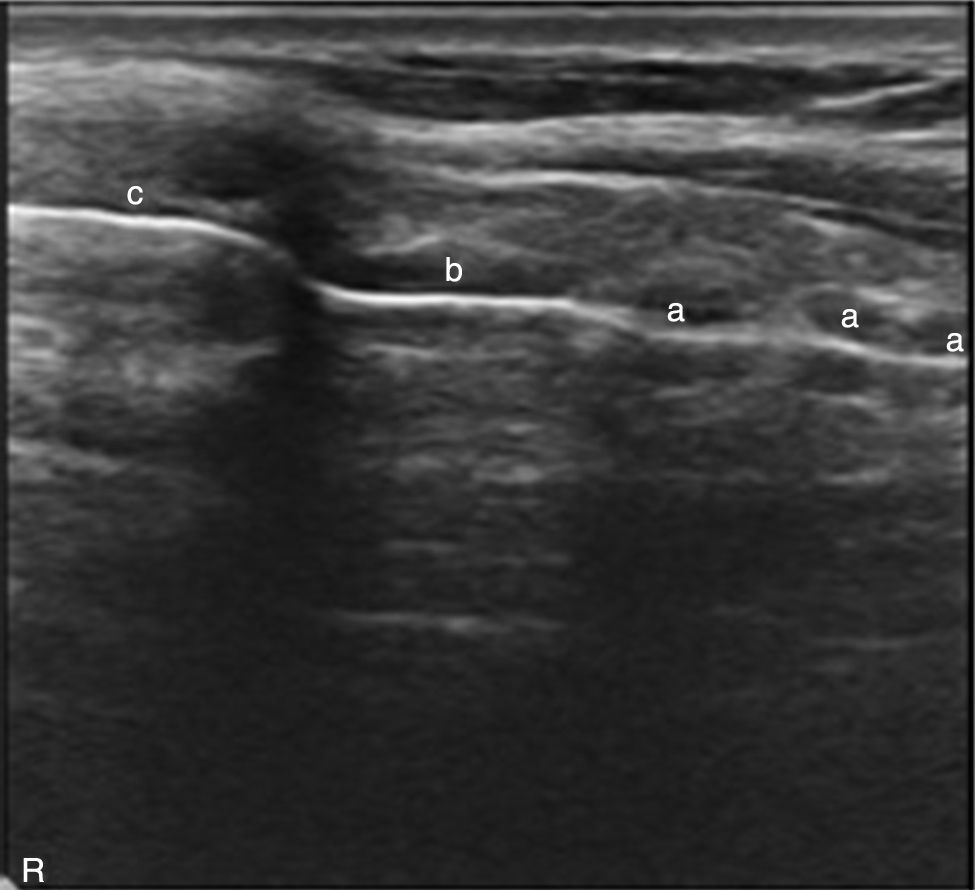
The cricoid cartilage is a hypoechoic, inverted U structure inferior to the thyroid cartilage; the posterior acoustic shadow corresponds to the airway Fig. 5. The window is more important to take transverse measurements and to select the size of the endotracheal tube.Cricothyroid membrane
A hypoechoic structure between the thyroid and the cricoid cartilages can be observed through a longitudinal section along the larynx (Fig. 6). Using color Doppler the blood vessels over the laryngeal and tracheal structures can be identified, to avoid the risk of puncturing the vessels when a trans laryngeal puncture is made.Tracheal rings
Semicircular hypoechoic structures can be seen at the longitudinal axis (Fig. 6). The puncture sites are located between the tracheal spaces for percutaneous tracheostomy.
Verification of endotracheal tube placementSeveral ultrasound techniques have been reported to detect proper intubation. These techniques may be direct with transverse or longitudinal visualization through the neck, or indirectly visualizing the pulmonary ventilation and the movement of the diaphragm; these may be assessed either at the time of intubation or after placing the endotracheal tube.9–13
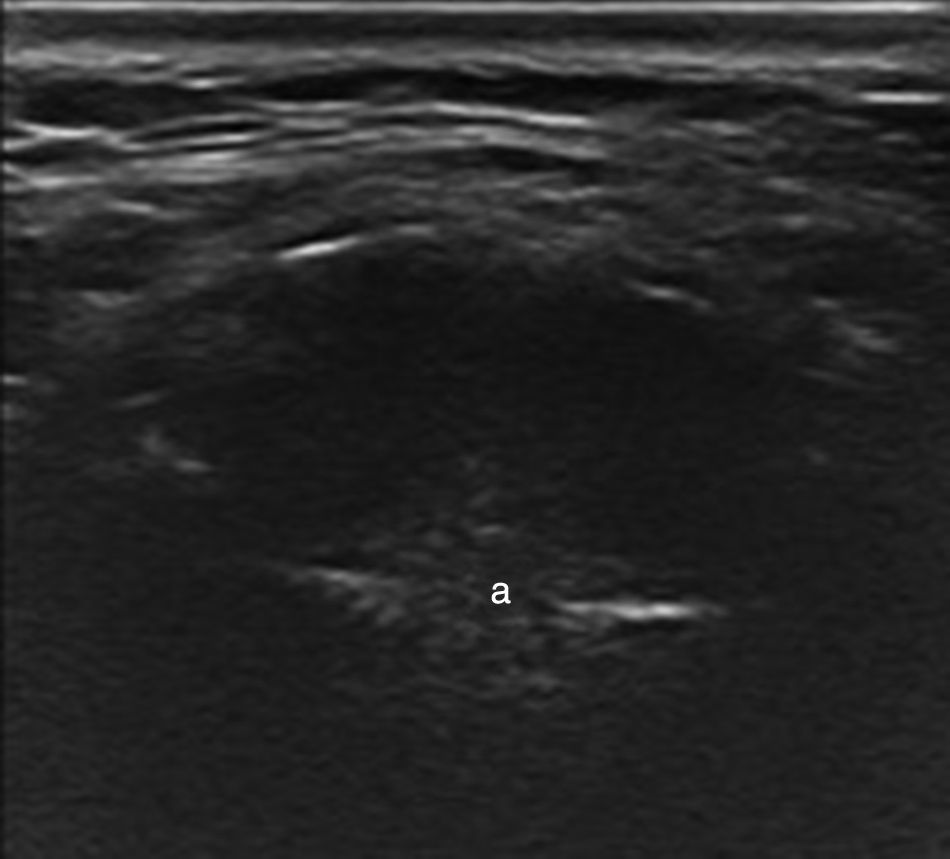
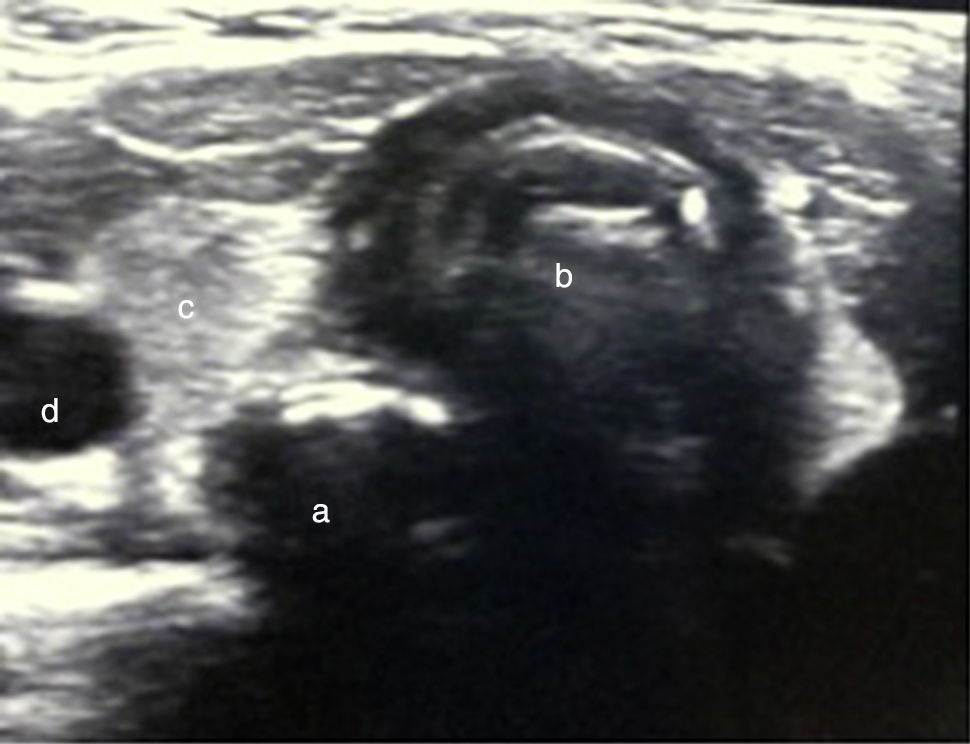
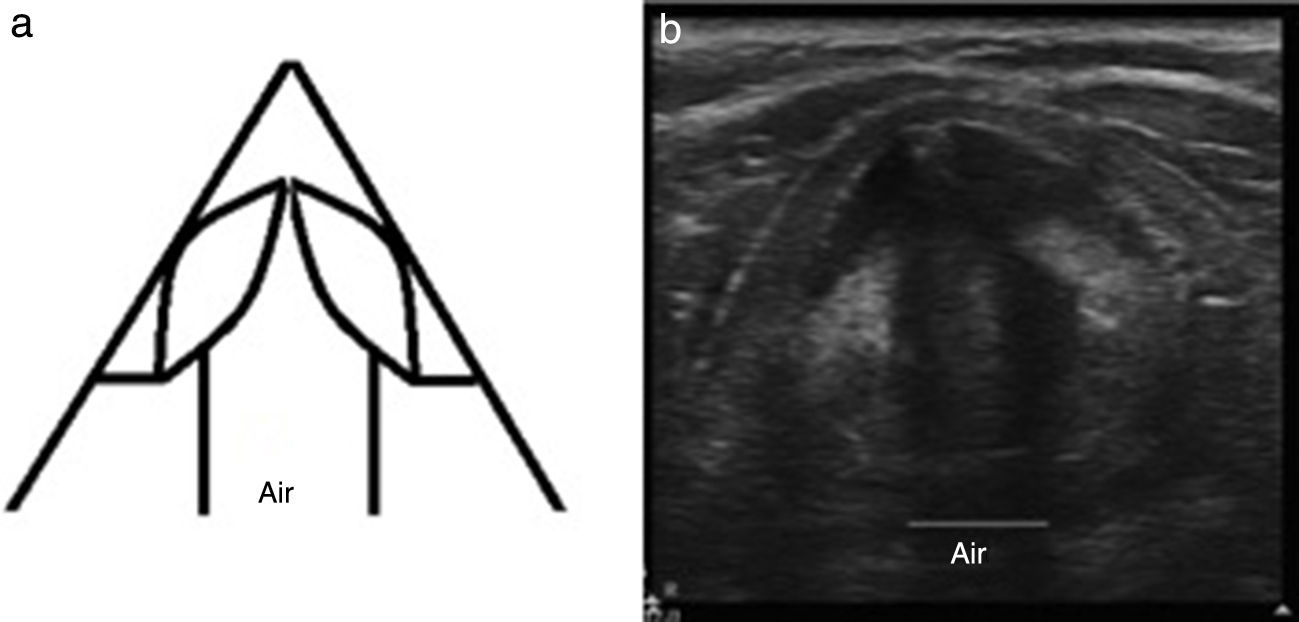
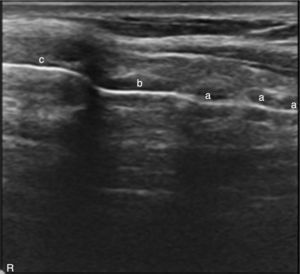
In order to obtain a proper transverse neck window for the detection of endotracheal intubation, the lineal transducer is used at the level of the cricoid cartilage, making sure that the esophagus is visualized. The successful endotracheal intubation may be confirmed in real time with the artifacts generated when the tube is introduced inside the trachea; if intubation fails, a new circular structure can be seen with artifacts generated by the presence of the tube inside the esophagus.13 This technique is similar with a longitudinal window, parallel to the left side of the trachea to visualize the esophagus; however, it is technically easier with a transverse window. In a tracheal intubation the movements of the tracheal rings are made visible and occasionally the endotracheal tube; if the intubation fails, a new air-filled structure deeper than the trachea will be identified (Fig. 7). The sensitivity of this strategy to detect esophageal intubation in real time with the intubation maneuver is 97 a 100%9,14 after just 5min of training15; furthermore, there is no need to ventilate and this represents one additional advantage of ultrasound versus the classical measures for checking tracheal intubation, particularly in patients with low cardiac output or cardiac arrest.14
The indirect tracheal intubation measures include the use of the lineal or curved transducer for checking ventilation throughout the pulmonary fields, visualizing the pleural shift between two ribs, with up to 100% rates to confirm both the tracheal intubation and the proper face mask ventilation or any other supraglottic device in patients with apnea.16 In addition to the confirmation of the bi-pulmonary ventilation, it is also possible to check the tracheal placement of the endotracheal tube instead of the principal bronchi and this approach has been successful in ICU pediatric patients to reduce the amount of X-ray radiation. Another option is the use of the curved transducer at the right and left costal-phrenic angles to visualize the diaphragm moving consistently with the mechanical ventilation to enable proper identification of the tracheal intubation in patients with pneumothorax.11
Measurement of the subglottic diameterNumerous successful cases have been reported since 2007 measuring the transverse subglottic diameter at the level of the cricoid cartilage for selecting the right external diameter of the endotracheal tube. This tool is particularly useful in pediatric >12 month-old patients when performing histopathological analyses.17–19
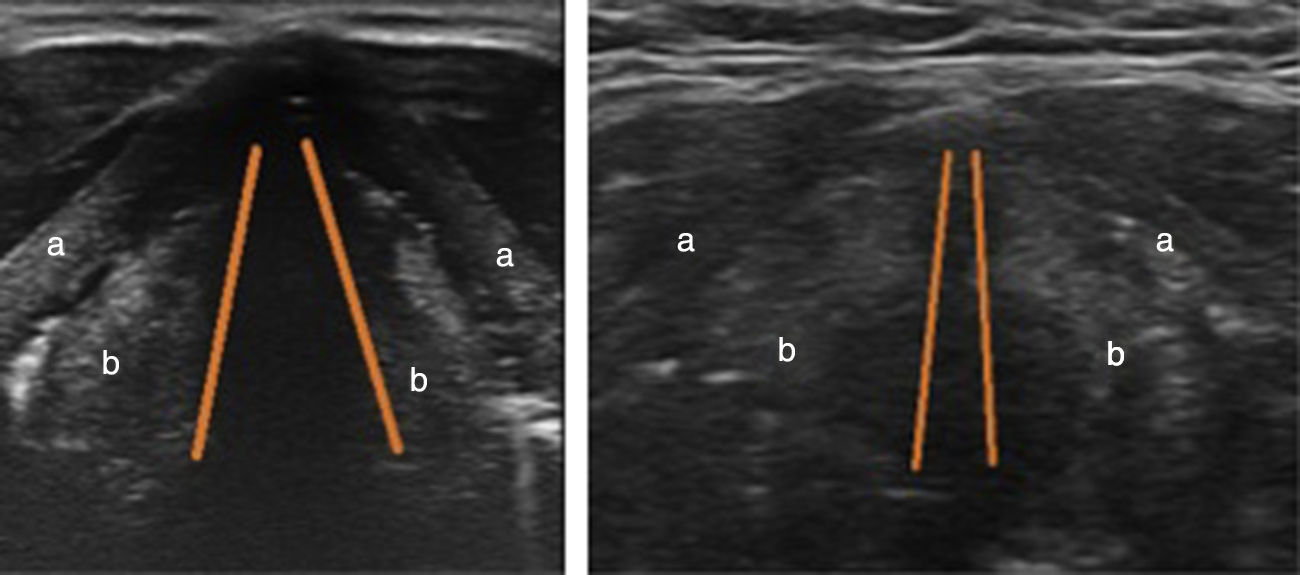
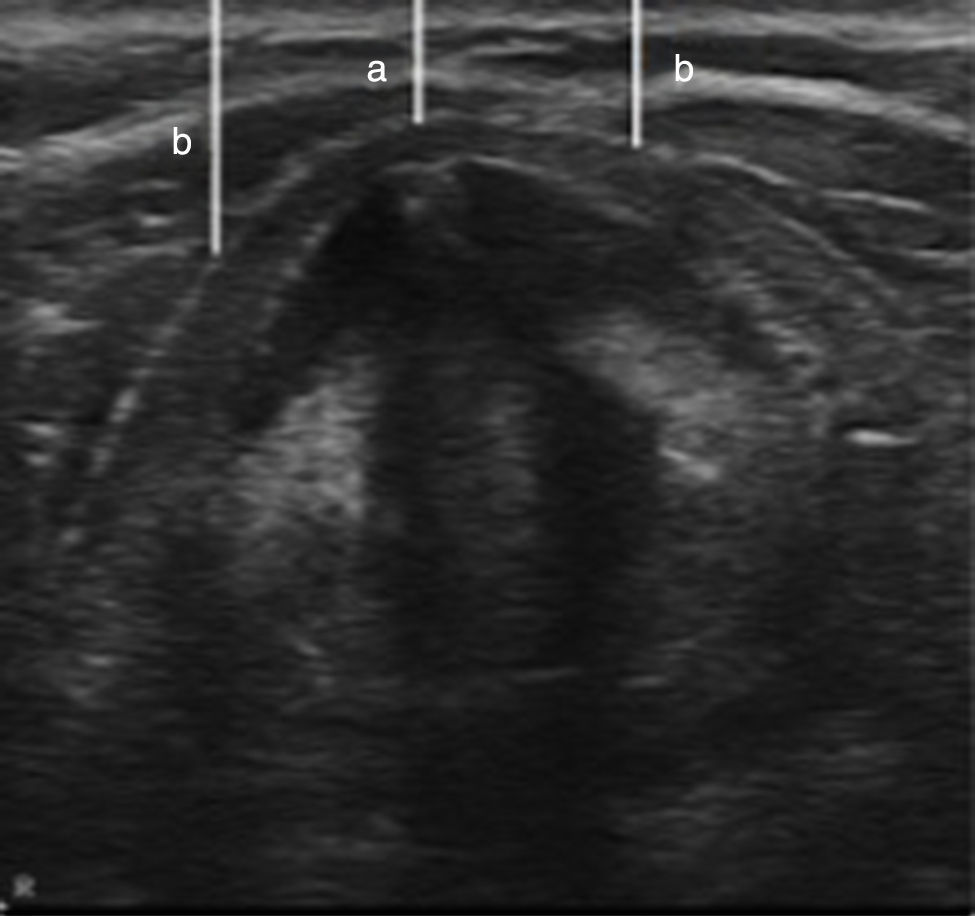
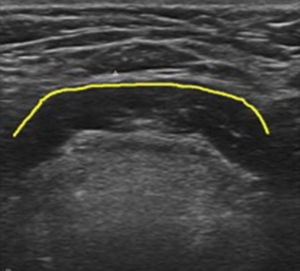
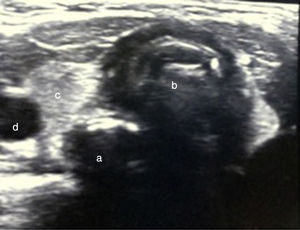
Difficult airway predictorsThere is growing academic interest in the use of ultrasound to identify the difficult airway predictors; though still under discussion, there are increasing numbers of papers on the topic, particularly to measure the pre-tracheal fat in obese patients. A transverse window at the level of the vocal cords is used for proper measurement, and then the anteroposterior diameter is measured at the midline from the skin of the trachea to 15mm of the right and left sides. If the sum of these three measurements exceeds 28mm in a patient with a neck circumference larger than 50cm and a BMI>35kg/m2, is predictive of a difficult laryngoscopy – Cormark visualization 3 or 4, in 70% of the cases (Fig. 8). According to Ezri et al.,20 all patients with difficult laryngoscopy were positively correlated with increased pre tracheal fat at the level of the vocal cords.20,21
Ultrasound guided trans laryngeal techniquesThough only few cases have been reported, there is a growing use of ultrasonography to guide trans laryngeal blocks to theoretically prevent airway bruising by selecting an avascular site for the puncture. Similarly, the use of ultrasound has also been described to guide the puncture for successful retrograde intubation and percutaneous tracheostomy, in patients in whom the identification of the structures is difficult such as in obese patients, patients with masses that distort the airway or trauma. In these cases, ultrasound helps with the correct identification of the airway and the cricothyroid membrane, and facilitates an emergency trans laryngeal approach if needed.5,22–25 Ultrasound is also helpful for the safe removal of the endotracheal tube in ICU patients that are intubated and require percutaneous tracheostomy (Fig. 9). However, there is no evidence of the superiority of ultrasound versus fibroscopy for guiding percutaneous tracheostomy.
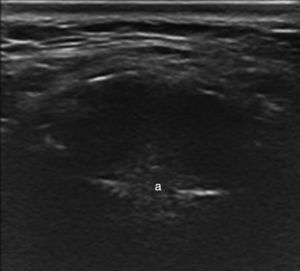
Predicting postextubation stridorThe use of ultrasonography may be a tool to identify patients at risk of stridor following extubation. In this case, the short axis in the thyroid window is evaluated (Fig. 10), measuring the air column in the laterolateral diameter; a measurement less than 4.5mm is considered a risk factor for stridor as compared to the normal 6.4mm value.26
ConclusionPerioperative ultrasound is a useful, easy to use, safe and non-invasive tool, with high sensitivity and specificity that does not require ionizing radiation and hence allows for improved performance, assisting in decision-making for the management of surgical patients, particularly the critically ill patient. Although its use in the airway is just starting to grow, there are clinical trials available showing high effectiveness, particularly in the context of ventilation, endotracheal intubation verification, endotracheal tube placement, and selection of the tube external diameter. However, further research is needed to determine whether the use of this technique may have any real impact on the outcomes of a mismanaged difficult airway.
FundingThe authors did not receive sponsorship to undertake this article.
Conflicts of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Zamudio-Burbano MA, Casas-Arroyabe FD. El uso del ultrasonido en el manejo de la vía aérea. Rev Colomb Anestesiol. 2015;43:307–313.