Ovarian cancer is the fifth deadliest cancer among women. There is no effective screening method. It has been suggested that ovarian cancer originates from precursor lesions in the fimbriae of the fallopian tubes.
ObjectiveThe aim of this study was to determine the level of knowledge of opportunistic bilateral salpingectomy by gynecologists.
MethodsA cross-sectional study was carried out and a survey was sent electronically to gynecologists and gynecology residents. Demographic characteristics as well as questions of interest related to clinical practice and indication for surgery were included.
Results52 subjects were included, 21 women and 31 men, with a mean age of 40.7 years. Thirty-five board certified gynecologists, as well as 17 gynecology residents, were included as part of the total survey group. Thirty-six individuals (69.2%) reported performing elective salpingectomy. The motivation they had to perform salpingectomy as a method of sterilization was: “reduction in the risk of ovarian cancer in the future” (55.6%). The indication for elective salpingectomy while performing other procedures was: “to prevent ovarian cancer” (61.1%). Certified gynecologists (42.9%) as well as residents (41.1%) considered “transvaginal ultrasound screening” as the best primary prevention method for ovarian cancer in low-risk women.
ConclusionsOpportunistic bilateral salpingectomy is safe and cost-effective. However, when gynecologists are interviewed to find out their level of knowledge, there is poor acceptance of opportunistic bilateral salpingectomy in Mexico. A training strategy should be designed in the gynecology residency in order to motivate ovarian cancer prevention.
El cáncer de ovario es el quinto cáncer más mortal entre las mujeres. No existe un método de detección eficaz. Se ha sugerido que el cáncer de ovario se origina a partir de lesiones precursoras en las fimbrias de las trompas de Falopio.
ObjetivoDeterminar el nivel de conocimiento de los ginecólogos sobre la salpingectomía bilateral oportunista.
MétodosSe envió una encuesta por vía electrónica a médicos ginecólogos y residentes de Ginecología. Se incluyeron características demográficas, así como preguntas de interés relacionadas con la práctica clínica y la indicación de cirugía.
ResultadosSe incluyeron 52 sujetos, 21 mujeres y 31 hombres, con una edad media de 40,7 años. Treinta y cinco ginecólogos certificados, así como 17 residentes de ginecología, se incluyeron como parte del grupo total. Treinta y seis individuos (69,2%) informaron haber realizado salpingectomía electiva. La motivación que tuvieron para realizar la salpingectomía como método de esterilización fue: «reducción del riesgo de cáncer de ovario en el futuro» (55,6%). La indicación de salpingectomía electiva mientras se realizaban otros procedimientos fue: «para prevenir el cáncer de ovario» (61,1%). Los ginecólogos certificados (42,9%) y los residentes (41,1%) consideraron la «detección con ultrasonido transvaginal» como el mejor método de prevención primaria para el cáncer de ovario en mujeres de bajo riesgo.
ConclusionesCuando entrevistamos a los ginecólogos detectamos poca aceptación de la salpingectomía bilateral oportunista en México. Se debe diseñar una estrategia de formación en la residencia de Ginecología para motivar la prevención del cáncer de ovario.
In the United States, ovarian cancer (OCa) ranks as the fifth deadliest cancer among women, with 21,410 deaths per year1; OCa has the highest proportion of deaths, even surpassing lung cancer.1 Stage I OCa 5-year survival rate is >90%; however, most of patients (∼75%) present with advanced stage (III/IV) tumors, for which the 5-year survival rate is 30%.1
Its high mortality is mainly attributed to a difficult early diagnosis. There is no effective screening method, which explains the lack of recommendations in low-risk patients. The proposed methods include annual measurement of CA-125 in plasma and/or transvaginal ultrasound, with inconclusive results and unnecessary surgical interventions.2 Oral contraceptives, bimanual palpation during pelvic examination, etc. have been used.
With the discovery of serous tubal intraepithelial carcinoma (STIC), it has been suggested that OCa originates from this precursor lesion in the fimbriae of the fallopian tubes (FT).3,4 Opportunistic bilateral salpingectomy (OBS) has been described, but there is no consensus regarding this approach.5,6 Therefore, the evaluation of the gynecologists’ position regarding OBS is interesting. In Mexico, this trend has not yet been evaluated, and the objective of this study was to determine the level of knowledge of OBS by gynecologists and the limitations for its implementation.
MethodsA cross-sectional study was carried out and for this purpose a survey7 was sent electronically to gynecologists and residents in gynecology in May 2022 (100 surveys sent and 10 hospitals have been included). The survey was sent on five different occasions, with an interval of 5 days between them. No physical surveys were conducted due to the effects of the Covid-19 pandemic. Under informed consent, respondents answered the survey anonymously. Gynecologists who did not wish to participate were excluded.
Prophylactic bilateral salpingectomy (with delayed oophorectomy) as risk-reducing surgery, is a preventative surgical technique that involves the removal of the FT, performed on patients who are at higher risk of having OCa, such as individuals who may have pathogenic variants of BRCA1/2 genes.8 Prophylactic bilateral salpingectomy is expected to be associated with reductions in the risks of ovarian, fallopian tube, and breast carcinoma.9
Opportunistic salpingectomy consists of the removal of the FT with ovarian preservation during benign gynecological procedures, once the desire for parity has been completed, i.e.: during hysterectomy or instead of tubal ligation (TL), in low-risk patients, in order to reduce the incidence of OCa, particularly serous Oca.10
Demographic characteristics as well as questions of interest related to clinical practice and indication for surgery were included. The qualitative variables were analyzed with absolute and relative frequencies, and quantitative variables with measures of central tendency such as mean and median, and measures of dispersion such as range and standard deviation.
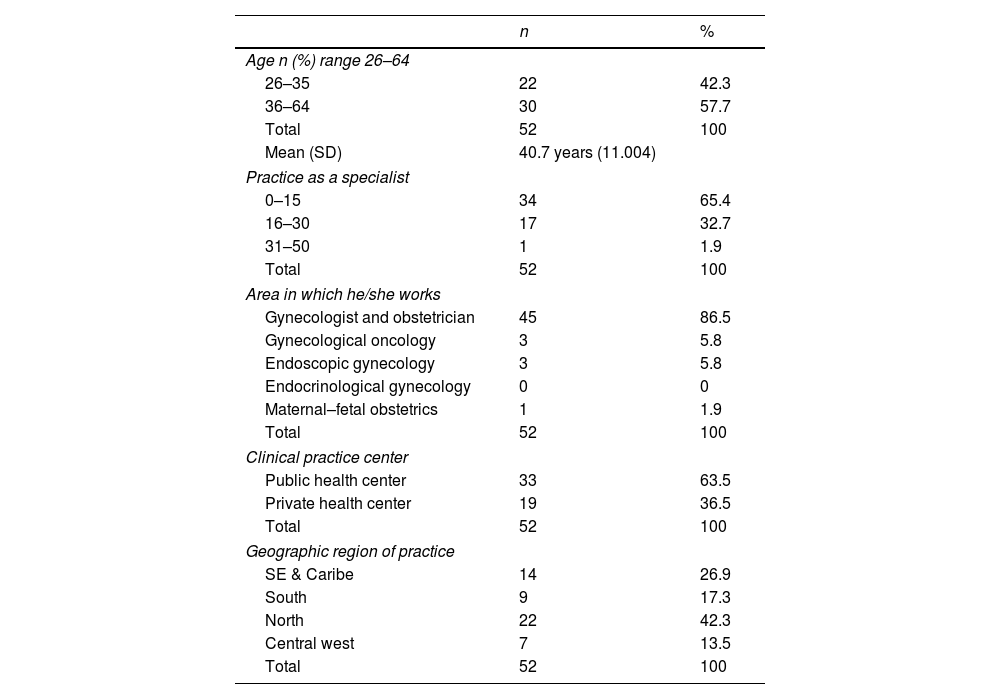
ResultsThe survey was answered by 52 physicians, 21 women (40.4%) and 31 men (59.6%), with a mean age of 40.7 (SD 11.007, range 26–64 years), which constitute the subject of this report. Thirty-five board certified gynecologists, 23 male and 12 female, as well as 17 gynecology residents, 9 female and 8 male, were included as part of the total survey group.
Participants reported an average of 11.5 years of gynecological practice (SD 9.614, range 0–32 years). The specialty area was mostly General Gynecologist Obstetrician (N=45), 33 of them (63.5%) worked in public health and 19 (36.6%) only in the private clinical practice. Their geographical region of the country was as follows: 14 in the Southeast and the Caribbean, 9 in the South, 22 in the Northwest and 7 in the Center of the country (Table 1). The number of hysterectomies for benign pathology performed per month was 4.8 on average (SD 6.814, range 0–42); surgical sterilizations performed per month on average were 7.3 (SD 9.757, range 0–60); the preferred technique for surgical sterilizations was “partial tubal section and ligation” (N=31) and only 16 preferred total salpingectomy. The type of primary prevention preferably performed by this group of gynecologists was “screening with transvaginal ultrasound” (N=22, 42.3%).
Socio-demographic characteristics of the gynecologists surveyed.
| n | % | |
|---|---|---|
| Age n (%) range 26–64 | ||
| 26–35 | 22 | 42.3 |
| 36–64 | 30 | 57.7 |
| Total | 52 | 100 |
| Mean (SD) | 40.7 years (11.004) | |
| Practice as a specialist | ||
| 0–15 | 34 | 65.4 |
| 16–30 | 17 | 32.7 |
| 31–50 | 1 | 1.9 |
| Total | 52 | 100 |
| Area in which he/she works | ||
| Gynecologist and obstetrician | 45 | 86.5 |
| Gynecological oncology | 3 | 5.8 |
| Endoscopic gynecology | 3 | 5.8 |
| Endocrinological gynecology | 0 | 0 |
| Maternal–fetal obstetrics | 1 | 1.9 |
| Total | 52 | 100 |
| Clinical practice center | ||
| Public health center | 33 | 63.5 |
| Private health center | 19 | 36.5 |
| Total | 52 | 100 |
| Geographic region of practice | ||
| SE & Caribe | 14 | 26.9 |
| South | 9 | 17.3 |
| North | 22 | 42.3 |
| Central west | 7 | 13.5 |
| Total | 52 | 100 |
Thirty-six gynecologists (69.2%) reported performing elective salpingectomy. The remaining 16 (30.8%) did not; the reasons for not performing it were the following: “it is not a protective factor for OCa” (31.3%, N=5), “it increases the risk of intraoperative bleeding” (25%, N=4), “it increases the operative time” (18.7%, N=3), “increases the risk of early ovarian failure” (12.5%, N=2) and “other reasons” (12.5%, N=2).
On the other hand, the motivation they had to perform Salpingectomy as a method of sterilization was: “reduction in the risk of OCa in the future” (55.6%, N=20), “the surgical method considered safer” (22.2%, N=8) and “decrease in the rate of re-intervention associated with adnexal pathology” (16.7%, N=6); one did not answer and one more answered “another”.
The indication for elective salpingectomy while performing other procedures was: “to prevent OCa” (61.1%, N=22), that “the tubes have no function after hysterectomy” (22.2%, N=8), “prevention of hydrosalpinx” (8.3%, N=3) and “decrease the risk of pelvic pain in the future” (5.6%, N=2); one participant did not answer.
The most frequent type of approach for elective salpingectomy was laparotomy (83.3%, N=30), followed by laparoscopy (11.1%, N=4); the vaginal route was only performed by two of them (5.6%).
Twelve participants (33.3%) considered the vaginal approach as a limitation to perform the salpingectomy (it was not for 17, 47.2%; 7 did not respond, 19.4%).
Twenty participants (55.6%) consider that elective salpingectomy reduces the risk of OCa due to “support of the current available literature”, 16.7% (N=6) due to “recommendation of the American College of Gynecology”, due to “suggestion of colleagues with training in gynecological cancer” in 11.1% (N=4), and by “institutional protocol” 5.6% (N=2); three gynecologists did not answer and one considered “other” answer.
Of the total number of respondents, 67.3% (N=35) were board certified specialists, 12 females (34.3%) and 23 males (65.7%), with an average age of 46.1 years (44.8 years for females and 46.7 years for males).
Fifteen participants (42.9%) considered “transvaginal ultrasound screening” as the best primary prevention method for OCa, while 31.4% (N=11) considered “ultrasound combined with CA-125 determination”. Four participants (11.4%) considered that there was no good primary prevention method for OCa. Only 8.6% of them (N=3) considered “Elective Salpingectomy” and 5.7% (N=2) considered “Salpingo-oophorectomy in people older than 50 years” (Table 2).
Behavior of the gynecologist according to the medical subspecialty.
| Gynecologist behavior | n | General gynecologistn (%) | Endoscopist gynecologistn (%) | Gynecologist oncologistn (%) |
|---|---|---|---|---|
| Primary prevention of ovarian cancer by screening with vaginal ultrasound | 22 | 21 (95.5%) | 1 (4.5%) | 0 |
| Primary prevention of ovarian cancer by performing salpingo-oophorectomy in people over 50 years of age | 2 | 2 (100%) | 0 | 0 |
| Primary prevention of ovarian cancer performing opportunistic salpingectomy | 5 | 4 (80%) | 0 | 1 (20%) |
| There is no primary prevention method to reduce the incidence of ovarian cancer | 9 | 7 (77.8%) | 0 | 1 (11.1%) |
| Performing Salpingectomy as a method of sterilization to reduce the risk of ovarian cancer in the future | 19 | 17 (89.5%) | 1 (5.3%) | 1 (5.3%) |
| Performing salpingectomy as a method of sterilization as it is considered the safest one | 8 | 8 (100%) | 0 | 0 |
| Salpingectomy as a method of sterilization to prevent hydrosalpingitis | 0 | 0 | 0 | 0 |
Percentages are not 100% because other gynecologists were not included for this analysis.
Twenty-five gynecologists (71.4%) reported performing elective salpingectomy. The remaining ten participants (28.6%) did not; the reasons for not performing it were the following: “it is not a protective factor for OCa” (40%, N=4), “it increases the operative time” (30%, N=3), “it increases the risk of intraoperative bleeding” (20%, N=2), and “increases the risk of early ovarian failure” (10%, N=1).
Fifteen respondents (42.9%) consider that elective salpingectomy reduces the risk of OCa due to “support of the current available literature”, 11.4% (N=4) due to “recommendation of the American College of Gynecology”, and four gynecologists did not answer.
The remaining 32.7% of the respondents (N=17) were gynecology and obstetrics resident physicians, nine (52.9%) females and eight (47.1%) males, with an average age of 29.6 years.
They believed that the primary prevention method to reduce the incidence of OCa in low-risk women, which offers greater benefits and fewer sequelae, was “screening with transvaginal ultrasound” in 41.1% (N=7), followed by “elective salpingectomy” (11.8%, N=2) or “Ultrasound and CA-125” (11.8%, N=2); however, five of them (29.4%) believed that “there is none”.
Eleven residents (64.7%) reported performing “elective salpingectomy”. The remaining six (35.3%) did not, because “it increases the risk of intraoperative bleeding” (N=2, 33.3%).
Five of them (29.4%) consider that elective salpingectomy reduces the risk of OCa due to “support of the current available literature”, due to “suggestion of colleagues with training in gynecological cancer” 17.6% (N=3), 11.8% (N=2) by “recommendation of the American College of Gynecology”, and by “institutional protocol” 5.9% (N=1).
DiscussionA 55.6% of the respondents reported as motivation for performing salpingectomy the possibility of favoring a decreased risk of future ovarian cancer and an additional 16.7% of the respondents to be supported by the recommendation of the American College of Gynecology. However, 30.8% stated that they did not perform opportunistic salpingectomy in low-risk patients.
It has already been demonstrated that a substantial percentage (60–88%) of ovarian high-grade serous carcinomas (HGSC) originate in FT.11 As early as 1999, Dubeau suggested that the ovarian surface epithelium (OSE) might not be the tissue of origin for Oca.12 In 2001, Pieck et al. drew attention to this issue when they revealed a high incidence (50%) of epithelial dysplasia on examination of FT from patients with BRCA mutations (BRCAm+).3 They reported that the dysplastic regions exhibited a switch toward the secretory phenotype (loss of hair cells and proliferative activity with Ki67 immunoreactivity). Shortly thereafter, other groups found occult FT cancers in BRCAm+ women, with incidence rates ranging from 0.9% to 17%.4
Medeiros et al., using a specific protocol for extensive examination, the so called SEE-FIM (Sectioning and Extensively Examining the Fimbriated End) protocol, discovered serous tubal intraepithelial carcinomas (STIC) in 38% of cases in the FT but not in the ovaries.13 Eighty percent of these STICs appeared exclusively at the fimbrial tip (Fig. 1). The same group later found seven early carcinomas among 122 BRCAm+ women, all originated from the fimbrial/ampullary region.14 A third study from this group documented STIC in 55 consecutive cases of serous pelvic cancer (ovarian, tubal, or peritoneal) not selected for BRCA status.15 In 42 cases designated “ovarian serous carcinoma”, 71% involved the FT and 48% of these contained STICs, which were located predominantly (93%) in the fimbrial region.15 These results suggest that many HGSC may actually be of tubal origin, arising from the distal region of the FT, and then rapidly spreading to the nearby ovary (Fig. 1).
Diagram of a fimbrial plica showing the attachment of an ovarian fimbria (right) to the ovary (left). The fallopian tube epithelium (FTE) is composed of a single layer of secretory and ciliated cells; “genetic hits” allow cells to acquire a proliferative capacity, leading to clonal expansion of normal-appearing FTE cells with a secretory phenotype, giving rise to serous tubal intraepithelial carcinoma (STIC). As STIC progresses to invasive serous carcinoma, malignant cells exfoliate from the fimbria and rapidly spread to the surface of the peritoneum and/or ovary. Exfoliation may occur prior to fimbrial invasion. Note the continuity of the epithelium of the fimbria and the ovarian surface epithelium; these structures become separated in the course of embryonic development, except for a remnant of this connection that persists in the adult, the ovarian fimbriae, which form a narrow isthmus extending from the oviduct onto the ovary.
The OSE retains a more primitive, multipotential state (lack of appropriate inductive influences during embryonic development).16 Importantly, the OSE and the FT remain connected by a narrow epithelial isthmus extending onto the ovary from the ovarian fimbriae.17 While the extraovarian peritoneum and the oviductal ampulla seem terminally differentiated, the intermediate distal fimbriae at the junction with the OSE may represent transitional epithelia with susceptibility to neoplastic progression linked to their plasticity and incomplete commitment to a differentiated state.16 Thus, CE-derived peritoneum, OSE, and tubal epithelium could be considered as a unit, with an area of increased susceptibility to neoplastic progression encompassing the OSE and the distal fimbriae [ovarian zone of transition (OZT) for epithelial neoplastic progression]16 (Fig. 1).
Cost-analysis modeling has showed that performing salpingectomy during hysterectomy represented a cost-effective measure for reduction of OCa risk, saving 23.9 million dollars.18 OBS with hysterectomy was less costly and more effective than hysterectomy alone; it also reduced the number of cases of OCa and prolonged average life expectancy. On the other hand, OBS for sterilization was considered more costly than TL because of longer operating time and higher complication risk; however, OBS was more effective in reducing the risk of developing OCa. The number needed to treat to prevent the diagnosis of OCa was acceptable for both scenarios.19 OBS is feasible, safe and cost-effective at the time of gynecological surgery.
Communities of physicians in several countries have accepted the recommendation of performing OBS for reduction of OCa risk. Seventy-five percent of women in Canada who underwent hysterectomy had OBS compared with just 8% in 2008.20 For surgical sterilization procedures, by 2013 almost half (48%) of tubal procedures performed were bilateral salpingectomies.20
In Canada, gynecologists have been asked since 2010 to discuss OBS with their patients as an OCa prevention strategy. Several gynecological societies have published recommendations to this effect that salpingectomy should be considered at the time of pelvic surgery in appropriate women. OBS at the time of gynecological surgery is now widely and routinely performed in many areas of the world.
However, when gynecologists are interviewed to find out their level of knowledge of the problem, there is little participation; a response rate of 25% was obtained in Canada.5 The study with the second largest number of participants had a response rate of only 20%.7
What has been most impressive is the poor acceptance of OBS in Mexico and Latin America. To our knowledge, there is no government or national association strategy in Latin America that motivates such OCa prevention. A training strategy should be designed in the gynecology and obstetrics residency in Mexico in order to motivate OCa prevention. It is already ethically questionable not to inform our patients about the possibility of a new preventive strategy based on opportunistic salpingectomy at the time of surgery for benign gynecological pathologies.
It is now indisputable that a substantial percentage of HGSC originates from the fallopian tube epithelium (FTE). However, whether the OSE gives rise to HGSC has been less clear. It is possible that some HGSC originate from the OSE or from endosalpingiosis.21
Since 2012, the same group that proposed the use of the SEE-FIM protocol13 to identify the cell of origin of ovarian serous carcinoma reported that in 50% of cases of ovarian HGSC, no lesions were found in the FT when using such a protocol.22 STIC is not universally detected in ovarian HGSC. In addition, some subsets of serous tubal intraepithelial neoplasias, including STIC, are actually HGSC metastases, rather than HGSC precursors, or intraepithelial metastases from a contralateral serous tubal intraepithelial neoplasia.23
After ovulation, the OSE may invaginate to form clefts and inclusion cysts. Entrapment of exfoliated FTE cells or OSE cells may be an early event in ovarian carcinogenesis. The estrogen-rich microenvironment of the ovarian stroma constantly stimulates the proliferation of these cells and can cause malignant proliferation.
A review of the literature on microscopic tumors of the ovary, FT, and peritoneum in BRCA1/2 mutation carriers showed that 60.5% were confined to the FT alone, where as 21.1% and 2.6% affected only the ovary or the peritoneum, respectively.11
LimitationsThe limitation of the study design is the reliance on remotely recorded information for data collection. This is particularly important for the collection of confounding variables. Another potential limitation of this study is that it was conducted nationwide but limited to known contacts, resulting in a convenience sample that could potentially underrepresent all groups, with possible overrepresentation of the third level. This limitation, however, is overcome by the fact that the problem is national and is of relevance, regardless of location and status.
ConclusionsApparently the real origin of HGSC in most cases originates from FTE and the putative OZT. Gynecologists must be updated in the prevention of these neoplasms. Education of staff gynecologists is recommended so that, in turn, they can teach gynecology residents in training.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Patient consentNA.
FundingNone declared.
Conflict of interestsThe authors declare that there are no conflicts of interest in relation to this study.
Eduardo Palacios Sanchez M.D., Mexican Social Security Institute (IMSS, acronym in Spanish), HGZ#16, Torreon, Coahuila, Mexico.