A substantial body of epidemiological and experimental evidence suggests the significance of serum uric acid as an important and independent risk factor of cardio vascular and renal diseases especially in patients with diabetes mellitus, hypertension. Hyperuricemia is a risk factor of coronary heart disease. Several studies showed positive association between hyperuricemia and CHD risk factors.
ObjectiveTo analyze the serum uric acid levels in patients with diabetes and hypertension, which helps in understanding its role as prognostic marker of coronary heart disease.
MethodThe study was conducted in population of Wadi-Al Dawasir (K.S.A.) aged 20–80 years through random sampling from October 2012 to June 2013. It included 250 samples and the cases were categorized into diabetic and hypertensive. In the cases, purely hypertensive were 52, diabetic were 57 and mixed group included both diabetic and hypertensive patients 65. Fasting blood was collected to analyze lipid profile which included (total cholesterol, triglycerides, high density lipoprotein, low density lipoprotein) and serum uric acid in association with age and heredity was also studied. Patient demographics were recorded.
ResultsThe study revealed significant association of serum uric acid (p<0.014*) and total cholesterol (p<0.007**) triglycerides (p<0.009**) low density lipoprotein (p<0.044*) in hypertensive group.
Serum uric acid levels in the mixed group patients with diabetes and hypertension reported serum uric acid (p<0.0037), total cholesterol (p<0.089+) proved to have increased risk of coronary heart disease. When compared to controls (non-diabetic p<0.529) and (non-hypertensive p<0.021*) with respect to serum uric acid levels show the magnitude of risk to coronary heart disease. With progressing age the association of lipid profile and serum uric acid reported (p<0.001**) in diabetics.
ConclusionSignificant correlations were found between serum uric acid and risk factors for CHD. This is first study of its kind in this region of K.S.A., which helps the community to understand the role of serum uric acid in coronary heart disease, justifies the objective of research in taking preventive measures to combat the deleterious effect of coronary heart disease. Prevention and early detection of elevated uric acid in both hypertensive and diabetic patients could serve as effective investigative tool in reducing coronary heart disease.
Una cantidad sustancial de pruebas epidemiológicas y experimentales sugieren la significación del ácido úrico sanguíneo como importante e independiente factor de riesgo cardiovascular y renal, sobre todo en pacientes con diabetes mellitus e hipertensión. La hiperuricemia es un factor de riesgo de enfermedades coronarias. Varios estudios muestran una asociación positiva entre la hiperuricemia y los factores de riesgo de cardiopatía coronaria (CC).
ObjetivoAnalizar los niveles de ácido úrico sanguíneo en pacientes diabéticos e hipertensos, lo que permitirá comprender el papel que desempeña como marcador pronóstico de las cardiopatías.
MetodologíaEl estudio se llevó a cabo en la ciudad de Wadi-Al Dawasir (Arabia Saudita) con participantes de 20–80 años mediante muestra aleatorizada, entre octubre de 2012 y junio de 2013. Se incluyeron 250 muestras; los casos se clasificaron en diabéticos e hipertensos. De ellos, 52 participantes eran solo hipertensos, 57 diabéticos, y existió un grupo mixto formado por 65 pacientes que eran a la vez diabéticos e hipertensos. Se tomaron muestras de sangre en ayunas para analizar el perfil lipídico (que incluía colesterol total, triglicéridos, HDL, LDL), y se estudió también la asociación del nivel de ácido úrico con la edad y la herencia. Se registraron las características sociodemográficas de los pacientes.
ResultadosEl estudio demostró una asociación significativa entre el ácido úrico sanguíneo (p<0,014*), el colesterol total (p<0,007**), los triglicéridos (p<0,009**) y la lipoproteína de baja densidad (p<0,044*) en el grupo con hipertensión.
En el grupo mixto, los pacientes con diabetes e hipertensión registraron ácido úrico sanguíneo (p<0,037). Se demostró que el colesterol total aumentaba el riesgo de cardiopatías (p<0,089+) en comparación con los grupos de control (no diabéticos p<0,0529, y no hipertensos p<0,021*). Al comparar los niveles de ácido úrico se muestra la magnitud del riesgo de cardiopatía coronaria. Con la edad, se ha descrito la asociación del perfil lipídico y el ácido úrico en pacientes diabéticos (p<0,001**).
ConclusiónExiste una correlación significativa entre el ácido úrico y los factores de riesgo de las CC. Se trata del primer estudio de este tipo en la región de Arabia Saudita que permite que la comunidad comprenda el papel que desempeña el ácido úrico en las cardiopatías coronarias. Justifica el objetivo de la investigación de tomar medidas preventivas para combatir el efecto dañino de las cardiopatías coronarias. La prevención y la detección precoz del ácido úrico elevado tanto en pacientes hipertensos como diabéticos podrían servir como herramienta útil de investigación para reducir las cardiopatías coronarias.
Cardiovascular diseases are considered to be of major public health concerns throughout the world including K.S.A. For several decades traditional risk factors are analyzed taking in to consideration of worldwide guide lines driving medical approach to solve the issues of cardiovascular disease, leading to the important reduction of mortality of patients.1 Despite the numerous efforts and encouraging achieved results we still observe residual cardiovascular risk that we need to address.2 Serum uric acid is implicated as one of the potential risk factors underlying the development of cardiovascular disease. Elevated serum uric acid is highly predictive of mortality in patients with coronary heart disease.3 Hyperuricemia is a pathological condition associated with increase in serum uric acid levels. The normal serum concentration of uric acid lies between 2 and 6mg/dl and in hyperuricemia the levels go beyond 7mg/dl in men and 6.5mg/dl in women.
Uric acid is an organic compound comprised of carbon, nitrogen, oxygen and hydrogen with scientific formula of C5H4N4O3. Hyperuricemia is becoming an increasing problem all over the world with a steady increase in its prevalence.4 Uric acid is the final product of purine metabolism. Recent epidemiological and clinical evidence suggests that hyperuricemia might be a risk factor for CHD, where oxidative stress plays an important role. Increased serum uric acid levels were caused by hereditary reasons. High levels of serum uric acid have been reported in diabetic and hypertensive.5 There is renewed concern about hyperuricemia and its associated disorders such as hypertension and diabetes.6
In the factors for CHD, oxidative stress plays an important pathophysiological role. Increased incidence of hyperuricemia in patients with CHD has been studied by.7 Serum uric acid serves as a useful biomarker, an indicator of prognosis in cardiovascular diseases.8,9 The assessment of independent prognostic value of serum uric acid is clinically relevant in essential hypertension, in which hyperuricemia is frequent and cardiovascular risk stratification is of utmost important.10 Hyperuricemia has been shown to increase the risk of CHD and related events like myocardial infarction leading to higher rates of mortality. The increase in serum uric acid in hypertension may be due to the decrease in renal blood flow that accompanies the hypertensive state, since low renal blood flow that accompanies the hypertensive state, which will stimulate urate reabsorption. Hypertension also results in micro vascular disease and this can lead to local tissue ischemia.11 Serum uric acid causes constriction of vessels by activation of rennin angiotensin system and decreased circulating nitric oxide which in turn causes the vascular smooth muscle cell to proliferate and promotes sodium sensitive elevated blood pressure.12 Diabetes mellitus is known to be associated with hyperuricemia. Hyperinsulinemia is seen in diabetes which results in decreased renal excretion of sodium and uric acid and causes hyperuricemia.13
A recent meta-analysis conducted14,15 that there is12% increase in mortality with extra 1mg/dl of uric acid in a person with CHD. Elevated serum uric acid level was associated with cardio vascular disease.16 There is direct relationship between hyperuricemia and hypertension.17 Uric acid has been suggested to play a role in pathogenesis of early onset of hypertension.18 The prevalence of hyperuricemia is 8.4% in Saudi Arabia.19
The presence of hyperuricemia increases the risk of CHD by approximately 70% in women, not in men.20 Uric acid measurement improves prediction of cardiovascular mortality.21 The study was carried out to investigate the prognostic role of serum uric acid as marker of CHD in population of Wadi Al Dawasir to signify its risk in both hypertensive and diabetics who are at major risk for coronary heart disease and compared with controls. Though studies on other risk factors were carried out in the past, this investigation is novel in its approach in studying the role of serum uric acid and the extent of risk on CHD in K.S.A. for the first time.
Materials and methodsThis study was hospital-based case control study conducted in patients attending private multispecialty Hospital Wadi Al-Dawasir (K.S.A.) from October 2012 to June 2013. After procuring the written consent from authorities, informed consent to subjects. The total sample size is 250 (which include 174 cases and 76 controls) Blood was collected after an overnight fasting. Blood was centrifuged for 30min at room temperature and clear serum was collected and stored at −20°C, until analyzed. The following variables were collected from patient include (age, gender, blood pressure, food, exercise, family history, etc.). Serum uric acid in association with age and heredity was considered (lipid profile which includes total cholesterol, low density lipoprotein, Triglycerides, High density lipoprotein), blood glucose. Estimation of biochemical parameters was done on STADFAX auto analyzer, using diagnostic kits as per the manufacturer instructions.
Inclusion criteriaHypertensive subjects, diabetic patients aged 20–80 years of both gender were taken. The cut off limit for hypertensive subjects was systolic blood pressure ≥140mmHg and diastolic ≥90mmHg.22 In the case of diabetics the fasting blood glucose cut off value is taken as 126mg/dl was considered.23
Exclusion criteriaThe following patients were excluded from the study were patients having history of chronic infections like tuberculosis, abnormal kidney function, pregnancy, endocrine disease, history of myocardial infarction within 6 months, patients on treatment with drugs (thiazides, loop diuretics, pyrazinamide and allopurinol, statins) were excluded from the study.
This was further analyzed and subjected to relevant statistical test by using SPSS package version 15.
Statistical methodsAll the study findings were analyzed statistically using the Statistical software, SPSS 15.0 (Student t test (two tailed, independent)) has been used to find the significance of study parameters on continuous scale between two groups (inter group analysis) on metric parameters. Chi-square/Fisher exact test has been used to find the significance of study parameters on categorical scale between two or more groups. Pearson correlation was used to analyze serum uric acid with lipid parameters with age.
Significant figuresAny result showing p value of p<0.001 was considered to be statistically significant.
ResultsAmong the 250 subjects 174 were patients and 76 were controls. Cases were taken in to consideration (diabetic, hypertensive) with age and heredity was analyzed.
Personal data from clinical proformaDemographics of the patient included in the study. The subjects of the study were 250. Cases were 174 (29.88%) of them were pure hypertensive; (32.75%) were pure diabetic and (37.35%) were mixed group (hypertensive and diabetic). Controls were 76 (100%) non-hypertensive and non-diabetic.
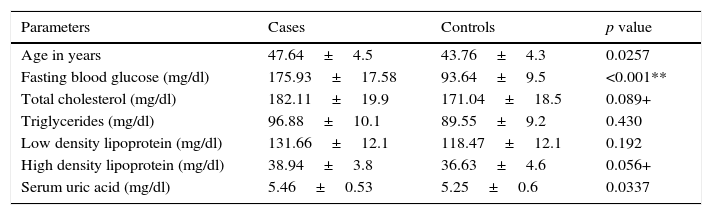
Table 1 depicts the analysis of blood glucose, lipid profile and serum uric acid. The comparison is made in cases (diabetics and hypertensive) with control groups. The fasting blood glucose values were found to be increased by 1-fold compared to controls. The cases showed mean±standard deviation 175.93±17.58 compared to controls 93.64±9.5 with significant (p value<0.001**). In total cholesterol the levels were found to be slightly elevated in cases compared to controls with (p<0.089+) significance. In case of triglycerides there was 10mg/dl units high in cases compared to controls with the HDL showed significant value of p<0.056+. Serum uric acid displayed 5.46±0.6 in cases compared to 5.25±0.6 in controls.
Comparison of study variables in two groups studied
| Parameters | Cases | Controls | p value |
|---|---|---|---|
| Age in years | 47.64±4.5 | 43.76±4.3 | 0.0257 |
| Fasting blood glucose (mg/dl) | 175.93±17.58 | 93.64±9.5 | <0.001** |
| Total cholesterol (mg/dl) | 182.11±19.9 | 171.04±18.5 | 0.089+ |
| Triglycerides (mg/dl) | 96.88±10.1 | 89.55±9.2 | 0.430 |
| Low density lipoprotein (mg/dl) | 131.66±12.1 | 118.47±12.1 | 0.192 |
| High density lipoprotein (mg/dl) | 38.94±3.8 | 36.63±4.6 | 0.056+ |
| Serum uric acid (mg/dl) | 5.46±0.53 | 5.25±0.6 | 0.0337 |
Fasting blood glucose <0.001**, total cholesterol=0.089+, high density lipoprotein=0.056+.
+ Suggestive significance, ** strongly significant (p value: p≤0.01), mg/dl=milligram/deciliter.
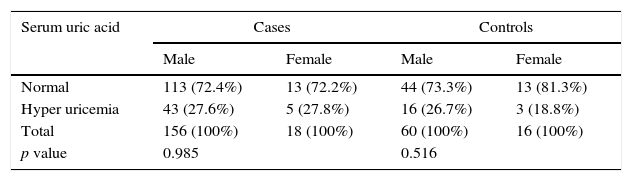
Table 2 summarizes the prevalence of hyperuricemia according to gender in cases and controls. Serum uric acid was analyzed both in male and female subjects. In males 27.86% exhibited hyperuricemia and in females 27.8% with (p<0.985) in cases compared to controls.
Prevalence of hyperuricemia according to gender in cases and controls
| Serum uric acid | Cases | Controls | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Normal | 113 (72.4%) | 13 (72.2%) | 44 (73.3%) | 13 (81.3%) |
| Hyper uricemia | 43 (27.6%) | 5 (27.8%) | 16 (26.7%) | 3 (18.8%) |
| Total | 156 (100%) | 18 (100%) | 60 (100%) | 16 (100%) |
| p value | 0.985 | 0.516 | ||
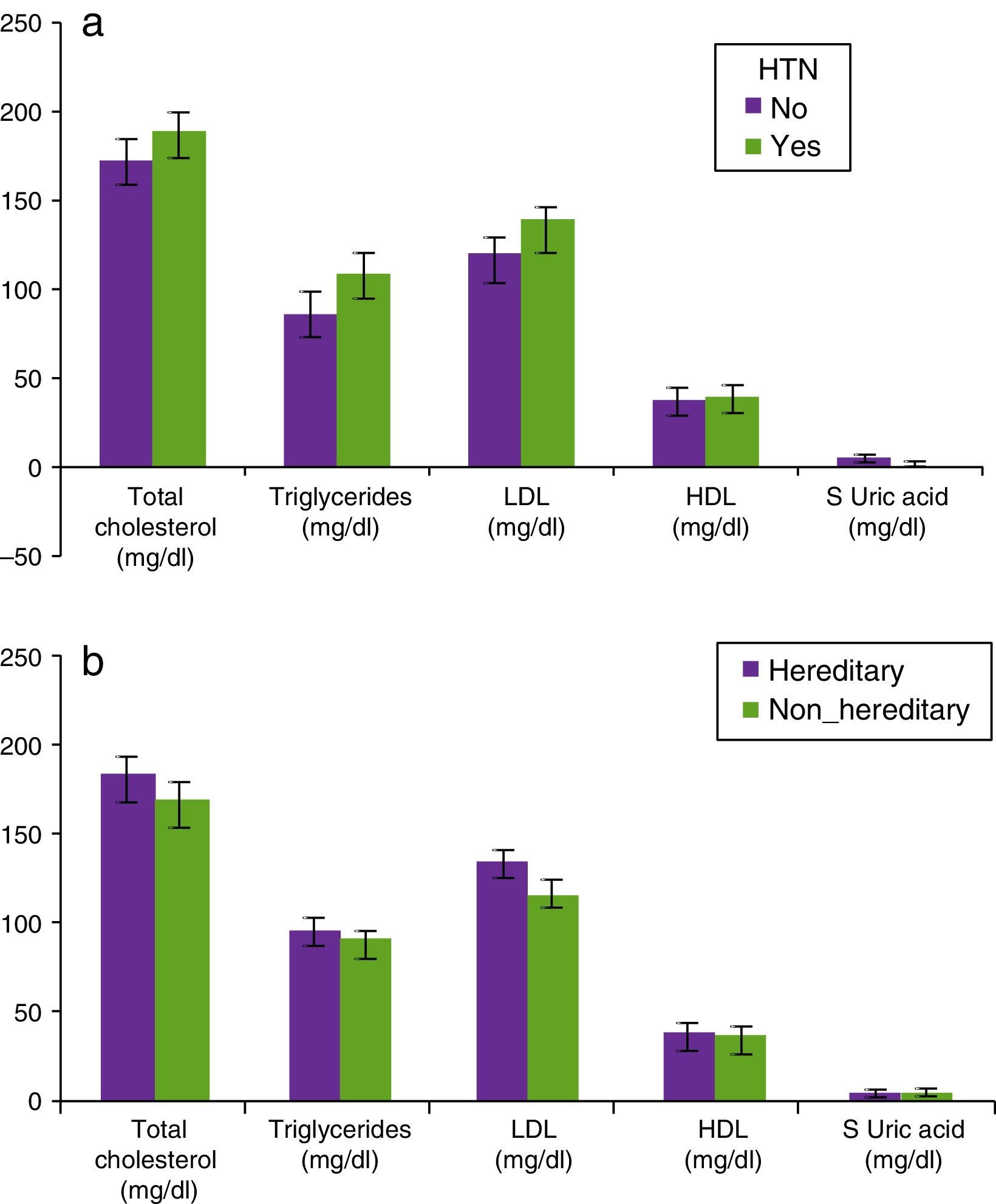
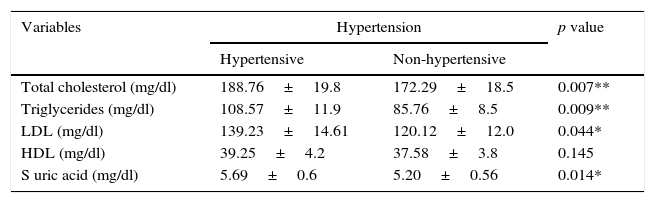
Table 3 describes the analysis of lipid parameters and serum uric acid in hypertensive and hereditary cases compared to controls. The total cholesterol in hypertensive cases was increased compared to controls with (p<0.007**). The triglycerides showed remarkable significance of (p<0.009**) in cases compared to controls. The LDL (low density lipoprotein) in cases with hypertension and positive hereditary background was increased compared to controls. There was no significant association in high density lipoprotein on contrary significant association was observed in cases for serum uric acid (p<0.014*) compared to controls (Fig. 1a and b).
Comparison of lipid parameters and serum uric acid based on incidence of hypertension and heredity in patients studied (n=250)
| Variables | Hypertension | p value | |
|---|---|---|---|
| Hypertensive | Non-hypertensive | ||
| Total cholesterol (mg/dl) | 188.76±19.8 | 172.29±18.5 | 0.007** |
| Triglycerides (mg/dl) | 108.57±11.9 | 85.76±8.5 | 0.009** |
| LDL (mg/dl) | 139.23±14.61 | 120.12±12.0 | 0.044* |
| HDL (mg/dl) | 39.25±4.2 | 37.58±3.8 | 0.145 |
| S uric acid (mg/dl) | 5.69±0.6 | 5.20±0.56 | 0.014* |
| Variables | Heredity | p value | |
|---|---|---|---|
| Hereditary | Non-hereditary | ||
| Total cholesterol (mg/dl) | 184.55±18.5 | 170.17±18.1 | 0.018* |
| Triglycerides (mg/dl) | 96.17±9.8 | 92.37±9.6 | 0.663 |
| LDL (mg/dl) | 135.62±14.2 | 115.9±12.1 | 0.037* |
| HDL (mg/dl) | 38.89±3.9 | 37.25±3.9 | 0.149 |
| S uric acid (mg/dl) | 5.41±0.61 | 5.37±0.68 | 0.841 |
Hypertensive-total cholesterol=0.007**, triglycerides=0.009**, low density lipoprotein=0.044*, serum uric acid=0.014*, mg/dl=milligram per deciliter.
Heredity-total cholesterol=0.018*, low density lipoprotein=0.037*.
* Moderately significant, ** strongly significant + suggestive significance.
(a) Comparison of lipid parameters and serum uric acid according to incidence of HTN in patients studied (n=250). Hypertensive-total cholesterol=0.007**, triglycerides=0.009**, low density lipoprotein=0.044*, serum uric acid=0.014*, mg/dl=milligram per deciliter. *Moderately significant. **Strongly significant. +Suggestive significance. (b) Comparison of lipid parameters and Serum Uric acid according to incidence of hereditary/non-hereditary in patients studied (n=250). Heredity-total cholesterol=0.018*, low density lipoprotein=0.037*. *Moderately significant.
The comparative analysis in cases with respect to heredity background reflected significant increase in total cholesterol compared to controls with p<0.018*. Triglycerides and high density lipoprotein, serum uric acid had not shown significant association. Low density lipoprotein displayed significant association of p<0.037*.
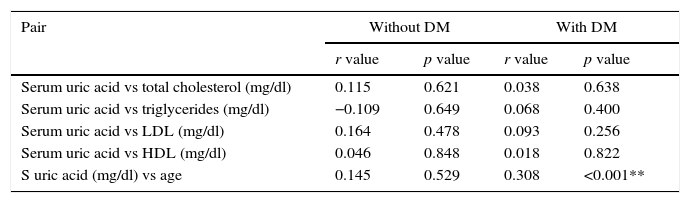
Table 4 shows correlation between Age, lipid parameters with serum uric acid in diabetes cases compared with non-diabetic suggest r=0.0308. Serum uric acid showed significant p value<0.001**.
Correlation between age, lipid parameters with serum uric acid with presence of DM (cases)
| Pair | Without DM | With DM | ||
|---|---|---|---|---|
| r value | p value | r value | p value | |
| Serum uric acid vs total cholesterol (mg/dl) | 0.115 | 0.621 | 0.038 | 0.638 |
| Serum uric acid vs triglycerides (mg/dl) | −0.109 | 0.649 | 0.068 | 0.400 |
| Serum uric acid vs LDL (mg/dl) | 0.164 | 0.478 | 0.093 | 0.256 |
| Serum uric acid vs HDL (mg/dl) | 0.046 | 0.848 | 0.018 | 0.822 |
| S uric acid (mg/dl) vs age | 0.145 | 0.529 | 0.308 | <0.001** |
r=0.308 moderate correlation p≤0.001**, **=strongly significant.
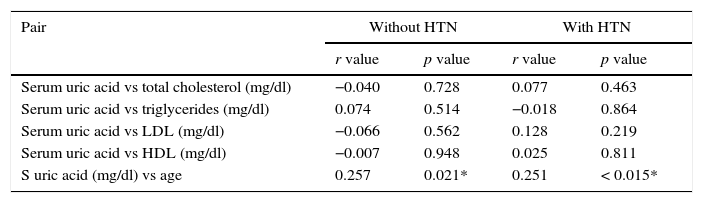
Table 5 depicts the correlation between lipid parameters and serum uric acid in hypertensive cases as p<0.014* moderately significant compared to controls p<0.021* in serum uric acid vs age.
Correlation between age, lipid parameters with Serum Uric Acid in HTN (cases)
| Pair | Without HTN | With HTN | ||
|---|---|---|---|---|
| r value | p value | r value | p value | |
| Serum uric acid vs total cholesterol (mg/dl) | −0.040 | 0.728 | 0.077 | 0.463 |
| Serum uric acid vs triglycerides (mg/dl) | 0.074 | 0.514 | −0.018 | 0.864 |
| Serum uric acid vs LDL (mg/dl) | −0.066 | 0.562 | 0.128 | 0.219 |
| Serum uric acid vs HDL (mg/dl) | −0.007 | 0.948 | 0.025 | 0.811 |
| S uric acid (mg/dl) vs age | 0.257 | 0.021* | 0.251 | < 0.015* |
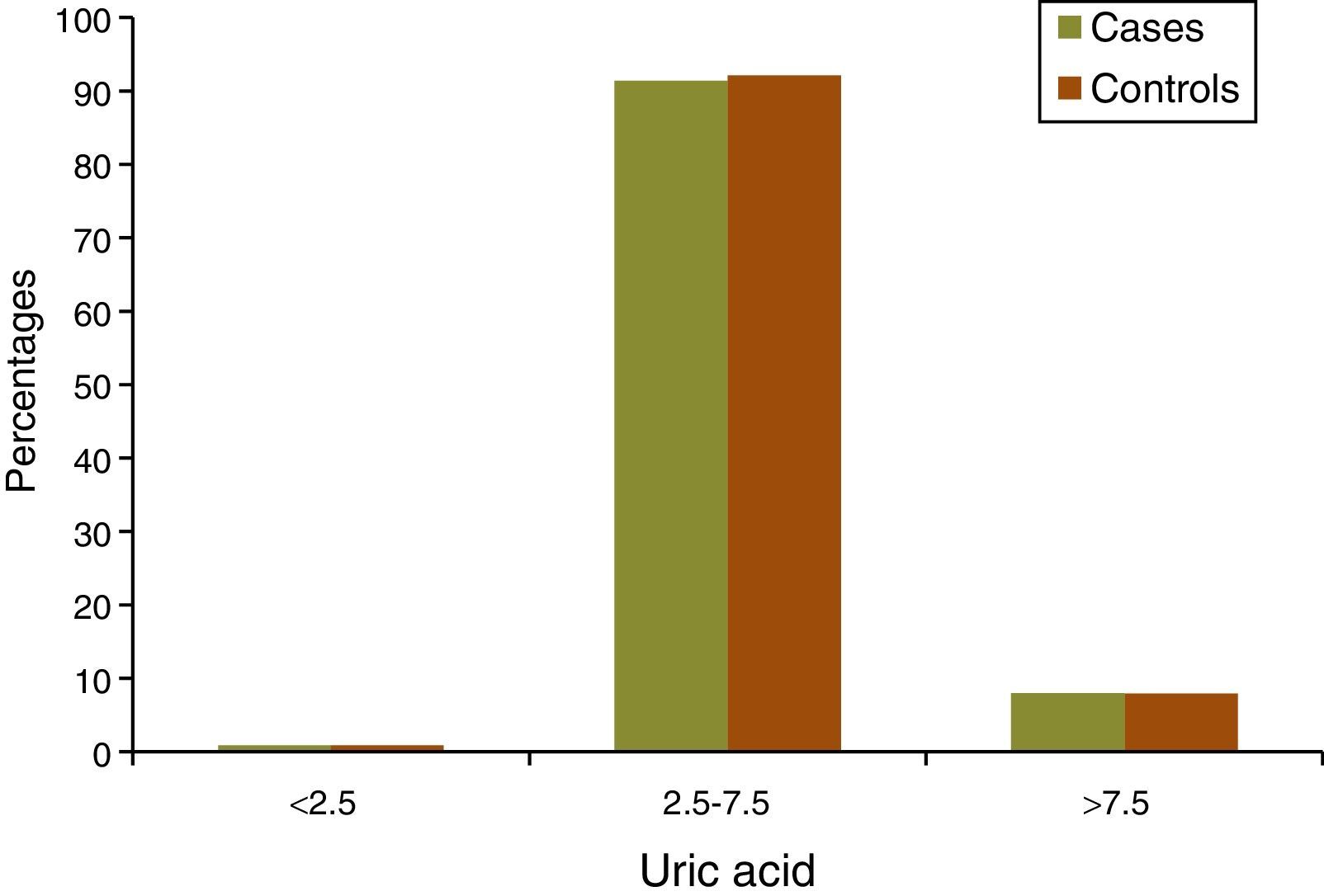
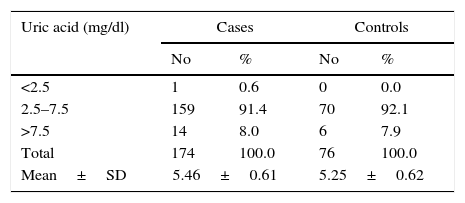
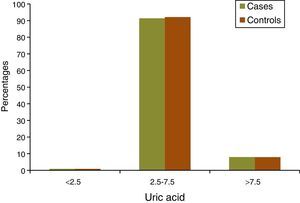
Serum uric acid both in cases and controls was compared. Total of 8% subjects reported hyperuricemia with serum uric acid level> 7.5mg/dl, which is similar to controls 7.9mg/dl (Fig. 2; Table 6).
The main idea behind this research is to understand the role of serum uric acid as prognostic marker of coronary heart disease. In this process the sample size of 250 cases were taken. The cases included 174 which were considered based on diabetes and hypertension. The controls were 76 who were non-diabetic and non-hypertensive.
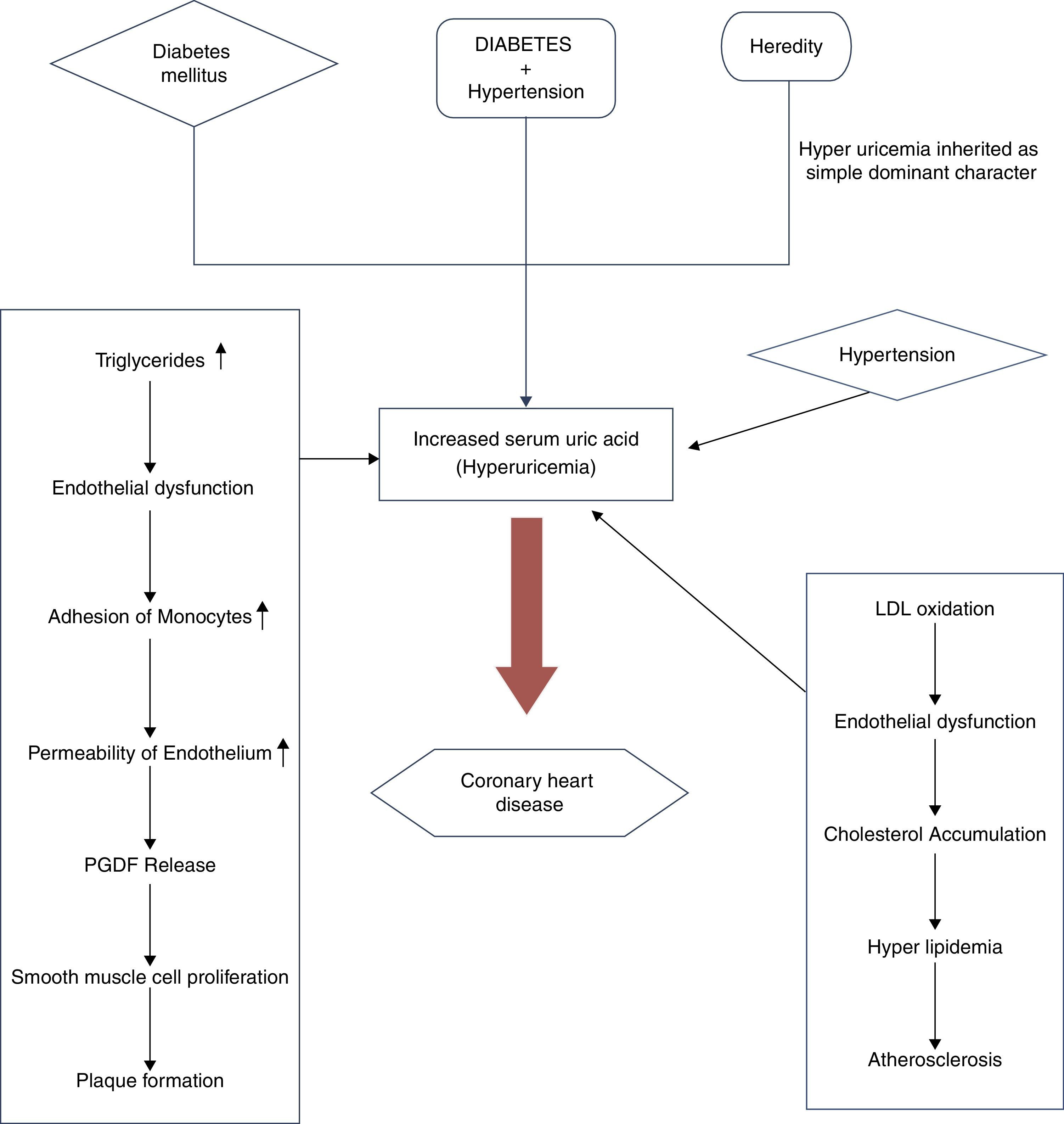
Hyperuricemia has been shown to increase the risk of coronary heart disease, leads to higher rates of mortality. Extra 1mg/dl of uric acid in a person with CHD leads to 12% increase in mortality, correlating elevated serum uric acid association with cardiovascular disease.16
There is a direct relationship between hyperuricemia and hypertension.17 Uric acid has been suggested to play a role in the pathogenesis of early onset of hypertension.18 The prevalence of hyperuricemia is 8.4% in Saudi Arabia. Our study revealed hyperuricemia in cases to controls by 27.58%. Significant association between hypertension and serum uric acid was observed with (p<0.014*). The risk of CHD is explained interns of hyperuricemia, essential dyslipidaemia,24 and serum uric acid levels are associated to atherosclerosis25,26 with risk of hypertension.27–29
In the present study, there were marked LDL values (p=0.044*) in hypertensive cases and (p=0.037*) in hereditary cases which explain hyperuricemia which in turn aids in the promotion of oxidation of LDL serves as key factor for the progression of atherosclerotic lesion and hall mark of CHD.30
Urate also impairs endothelial function through LDL oxidation and contributes to atherosclerotic risk.31 In the current study, the increased serum uric acid levels in hypertensive cases carry elevated risk to progression of CHD function; supported by studies.32–35
Increased triglycerides (0.009**) and total cholesterol (p<0.007**) in hypertensive are explained in terms of hyperlipidemia altering the endothelial function, the adhesion of monocyte causing the increased permeability of endothelium resulting in adhesion of platelets and PGDF, and facilitate smooth muscle cell proliferation24 causing atheromatous plaque.
Serum uric acid levels were significantly increased (p < 0.001**) in diabetics when age and lipid parameters were considered, correlated with findings of.29 The intensity of risk in mixed segment both with diabetes and hypertension would eventually increase, lead to attenuation of CHD.38–44
Diabetes has been recognized to be an independent risk factor for CHD with hyperuricemia.45,46 Elevated serum uric acid 4mg/dl is considered to be red flag in patients with risk for CHD47 that coincides with prospective studies for diabetics.
Hyperuricemia via purine metabolism promotes thrombus formation.20 This was evidenced in the present study with hereditary segment (p<0.841), and total cholesterol (p<0.018*) in positive hereditary cases would offer deleterious effect on cardiovascular health. A multiple risk factor clustering syndrome has been considered to be responsible for increased serum uric acid levels in CHD questioning the role of serum uric acid level as an independent risk factor.36 Hyperuricemia is an independent predictor for early atherosclerosis.37
Hyperuricemia is inherited as simple mendelian dominant character. Genetic predisposition has been considered to be the most significant factor for development of CHD.48
Thus we understand that based on studies the complexity of hyperuricemia and its relationship with inflammation, atherosclerosis, and oxidative stress make it a resilient factor. Serum uric acid screening is recommended which serves as biomarker and indicator of prognosis of cardiovascular disease.8,9 The measurement of uric acid improves the prediction of cardiovascular disease.21
Outcome of researchThe present investigation had led us to the following findings:
*Out of 250 subjects 174 were cases and 76 controls were observed.
*The cases were categorized into (52 purely hypertensive), (57 purely diabetic) and (mixed 65 having both hypertension and diabetes).
*Hyperuricemia was observed in cases of hypertension (p<0.014*) and diabetes mellitus (p<0.001**).
*The lipid profile analyzed showed that total cholesterol, triglycerides, and low density lipoprotein increased in hypertensive group compared to control.
*Patients within mixed group (diabetic and hypertensive) showed significant increase in total cholesterol values compared to controls.
*Fasting blood glucose was found to be significant (p<0.001**) in cases.
*The patients with positive hereditary background showed attenuated levels of total cholesterol (p<0.018*) and LDL (p<0.037*) found to be significant.
*In diseased condition 91.4% of patients exhibited the levels of serum uric acid were between 2.5 and 7.5mg/dl, and remaining 8% of the cases showed >7.5mg/dl.
*Significant correlation was found between serum uric acid and risk factor for CHD.
*Early detection of increased serum uric acid in cases could serve as effective investigative tool which helps in reducing coronary heart disease.
*This is first study of its kind in this region of K.S.A. which helps the community to understand the role of serum uric acid in coronary heart disease, and justifies the objective of research in taking preventive measures to combat the deleterious effect of coronary heart disease.
The epidemic of coronary heart disease in developing countries tends to be inevitable. The cost effective and modifiable serum uric acid elevation in both hypertensive and diabetic patient could serve as an effective investigation tool to promote the search for other cardiovascular risk factors. The study had less number of controls. Future studies would be conducted on large scale to examine hyperuricemia overtime which would help us to evaluate its impact on CHD Counseling at the grass root level with focused health education at the community level, by recommending the diet to reduce uric acid levels and adopting healthy life style.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained informed consent of the patients. The author for correspondence must be in possession of this document.
FundingThe study was supported by Deanship of Scientific Research (Prince Sattam Bin Abdul Aziz University) 18/Sa/33.
Conflict of interestThe authors declare no conflict of Interest.
The authors are grateful to Deanship of Scientific Research. They express their sincere gratitude toward Prince Sattam bin Abdul Aziz University, for rendering financial support to make this research feasible.