The aim of the study was to evaluate the effect of rosuvastatin and atorvastatin on endothelial dysfunction, lipid peroxidation, tissue cholesterol and plasma lipids in dyslipidemic rabbits.
MethodsForty male New Zealand white rabbits were divided into four groups (n=10): mixed dyslipidemia (GH), normal cholesterol (GN), rosuvastatin (GHR) and atorvastatin (GHA). The animals were fed a cholesterol diet supplemented with 0.5% fat and 10% coconut oil for 45 days. On the 15th day, blood samples were collected by puncture of the marginal ear vein for a total plasma cholesterol determination before starting treatment and distribution of animals in groups with similar blood cholesterol levels. Diet plus rosuvastatin and atorvastatin was administered by gavage in daily doses of 2.5mg and 10mg respectively. At the end of the experiment, after 45 days, the blood sample was collected by cardiac puncture was measured for cholesterol, HDL-C, LDL-C, TG and isolation of LDL. The animals were sacrificed by dislocation of cervical spine, and the aorta was removed for the study of endothelial function, measurement of tissue cholesterol, LDL and MDA. The results were compared by nonparametric statistical methods.
ResultsThere was a significant increase in all parameters studied in GH compared to GN. There was a significant reduction in all parameters when comparing GHR and GHA to GH. As for effectiveness in reducing CT, TG, LDL-C and LDLox, GHA was shown to be more efficient than the GHR. However, for tissue cholesterol, MDA and endothelial dysfunction, there were no statistically differences between both groups.
ConclusionsRosuvastatin and atorvastatin were similar in improving endothelial dysfunction, reduction in tissue cholesterol and lipid peroxidation.
Detectar el efecto de rosuvastatina y atorvastatina en disfunción endotelial, peroxidación lipídica, colesterol y lípidos en tejidos en conejos dislipémicos.
MétodosConejos machos, asignados al azar: dislipemia mixta (GH), no hipercolesterolémicos (GN), rosuvastatina (GHR) y atorvastatina (GHA) (n=10). Con dieta suplementada con grasa de coco al 10% y colesterol al 0,5% w/w por 45 días; 15 días después, con punción venosa en la vena marginal de la oreja se recogieron muestras de sangre para determinar el colesterol total plasmático con la finalidad de iniciar el tratamiento y distribuir a los animales en los grupos con grados semejantes de colesterolemia. Se administró dieta + rosuvastatina 2,5mg y atorvastatina 10mg por día por animal de GHR y GHA. Después de 45 días se recolectaron muestras de sangre por punción cardíaca para determinación de colesterol, triglicéridos (TG), colesterol de las lipoproteínas de alta densidad (cHDL) y colesterol de las lipoproteínas de baja densidad (cLDL). Los conejos fueron sacrificados por desplazamiento de la columna cervical. Mediante toracotomía se retiró la aorta para estudio de función endotelial, medida del colesterol en tejidos, malondialdehído (MDA) de pared de aorta y cLDL. Los resultados se compararon por métodos estadísticos no paramétricos.
ResultadosSe demostró el aumento de los parámetros estudiados en GH en relación con GN. En GHR y GHA hubo reducción significativa de parámetros en relación con GH. Hubo diferencia significativa en resultados entre GHA, que fue más eficiente en la disminución de CT, TG y cLDL, en relación con GHR. Sin embargo, en relación con el colesterol en tejido, MDA y disfunción endotelial no hubo diferencias significativas entre GHR y GHA.
ConclusionesLos resultados demostraron que rosuvastatina y atorvastatina son eficientes en la mejora de la disfunción endotelial, al reducir la susceptibilidad del cLDL para sufrir peroxidación y el colesterol en los tejidos.
Pioneering epidemiological studies lasting over 40 years and carried out in the city of Framingham (USA), demonstrated that coronary atherosclerosis is related to hypercholesterolemia, seeing that, the risks increased1 proportionally to higher levels of cholesterol. It can lead to an endothelial cells dysfunction, which is correlated to atherosclerosis2,3. The decrease of clinical coronary events, observed in studies of hypercholesterolemia interventions, was associated with an improvement in the endothelial dysfunction and this seems to be critical in the stabilization of the atherosclerotic plaque, together with the improvement of the inflammatory process4,5.
The HMG-CoA reductase inhibitor, a key substance in the synthesis of cholesterol by the liver, represents the main strategy for reduction of coronary events in the hypercholesterolemic patients. It is directly related to the decrease of plasmatic cholesterol levels. Although rosuvastatin has been the most used statin at present as cholesterol reductor, it has not been fully studied yet. Thus, its effects on endothelium function, lipidic peroxidation, tissue cholesterol and plasmatic lipids was evaluated and compared to those of atorvastatin which hipolipemic action and pleiotropic effects are well-studied.
MethodsThe experiments were performed in accordance to the guidelines suggested by the US National Institutes of Health for the care and use of laboratory animals (NIH publication N 85-23 revision). The paper was certified by the protocol number 619–1 of Institutional Committee for Ethical Principles for Animal Research (State University of Campinas – Unicamp).
Forty male New Zealand white rabbits, 12 week-old, weighing 3.0-3.5kg were used in the study. The animals were randomly distributed in four groups, with 10 animals each: mixed dyslipidemia (GH), normocolesterolemic (GN), rosuvastatin (GHR) and atorvastatin (GHA). The standard diet was enriched with cholesterol 0.5% and coconut oil fat 10% and administered to rabbits in groups GH, GHR and GHA for 45 days. The rabbits in group GN received standard diet for 45 days. The animals were identified and kept in individual cages with controlled temperature.
Rosuvastatin and atorvastatin were commercially acquired and they were administrated by gavage, after dilution in distilled water in a single dosage of 2.5mg and 10mg, respectively, per animal. The administration of lipidic diet continued at the final experiment in the GH, GHR and GHA groups. Total cholesterol, triglycerides, HDL-c plasmatic were dosed at the beginning and the end of the experiment using enzymatic kits and measured by spectrophotometer (500nm). Blood samples were collected by puncture of the marginal ear vein and cardiac puncture at the beginning and end of the experiment respectively. Friedwald formula was used for LDL-c plasmatic measurement. Low density lipoprorotein was measurement yet by sequential ultracentrifugation of plasma according to the method of Havel et al8. Thus, plasma was centrifuged at 40 000rpm for 18h at 4°C in a TI50 rotor (Beckman, L8, Palo Alto, CA) and the very low-density liprotein (VLDL) layer (d < 1.006g/ml) was removed. The remaining supernatant was adjusted to a density of 1.063g/ml using KBr and was centrifuged at 40 000rpm for 20h. The isolated LDL was dialyzed with 0.01M phosphate buffered saline (PBS), pH 7.4, at 8°C for 24h, with frequent buffer changes. LDL (100μg of protein) was incubated for 24h at 37°C with 5μmol of copper sulfate.
Tissue cholesterol was determined according to the method of Naito et al9. The specimens were dried and homogenized at 4°C in 5ml of 0.013M Tris–HCl (pH 7.4), containing 0.01 NaN3. Total lipids were extracted from the homogenates in 10 vol. of chloroform-methanol (2:1, v/v) containing 0.001% butylated hydroxytoluene as an antioxidant. The total cholesterol content was measured by a specific enzymatic assay and the results expressed in mg/g dry tissue.
Lipid peroxidation was performed in aorta vessel and it was assessed by measuring the content of malondialdehyde (MDA) according to the method of Bueg et al10, specified as follows. Aortic segments were homogenized in ice-cold 10% (w/v) trichloroacetic acid (100mg of tissue per 5ml of TCA). After centrifugation, a portion of the supernatant was added to an equal volume of 0.6% (v/v) thiobarbituric acid and the mixture heated at 100°C for 20min. The resulting MDA concentration was calculated from the absorption at 532nm using a molar extinction coefficient of 1.49 × 10-5 and was expressed in nmol/ mg tissue ×10-7.
A segment of the thoracic aorta in its proximal region was used for evaluation of the endothelium function measured according to the standardized technique by Furchgott et al11. This segment, free from the conjunctive tissue and with special care to preserve the complete endothelium, was suspended in a bath of 10ml of volume containing solution of Krebs-Henseleit of pH 7.4, being the composition in mmol/l: NaCl 113; CaCl2 21.9; NaHCO3 25; MgSO4 0.44; KH2PO4 1.18; EDTA 0.03; glucose 11.
The relaxation curves were compared by co-variance analysis and the values of the plasmatic and tissue cholesterol were expressed on average and standard shunting line and submitted to test t of Student for non-parametric values. The resulting averages were compared by the Student-Neuman-Keuls test. The values of plasmatic and tissue cholesterol and the magnitude of the reversion of the endothelial dysfunction were correlated by variance analysis and the test of Tukey. Significant values were those with p < 0.05.
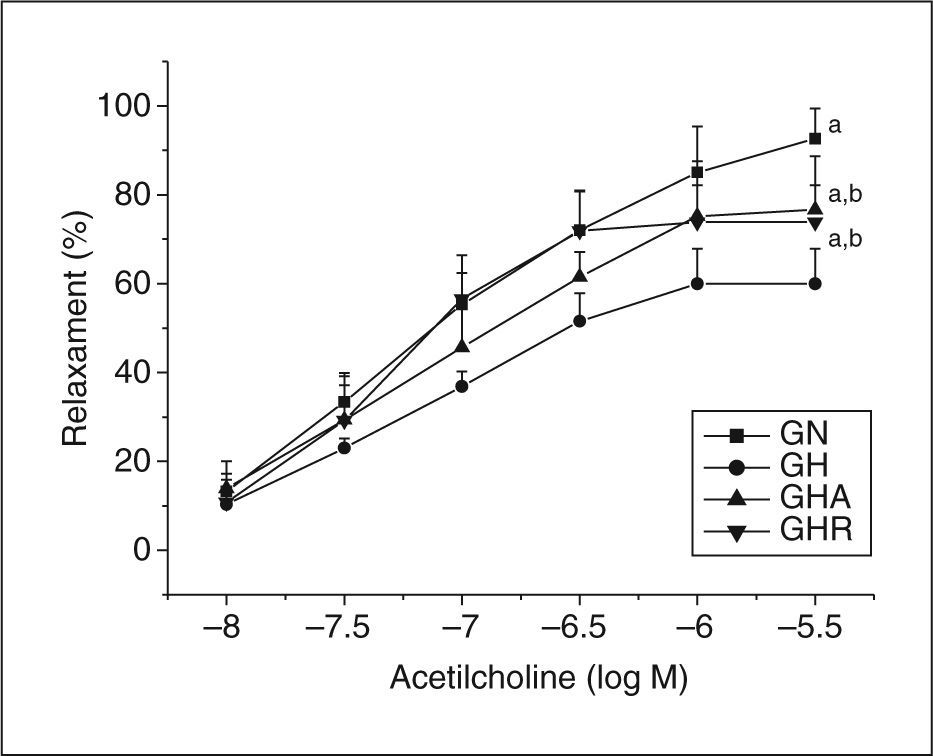
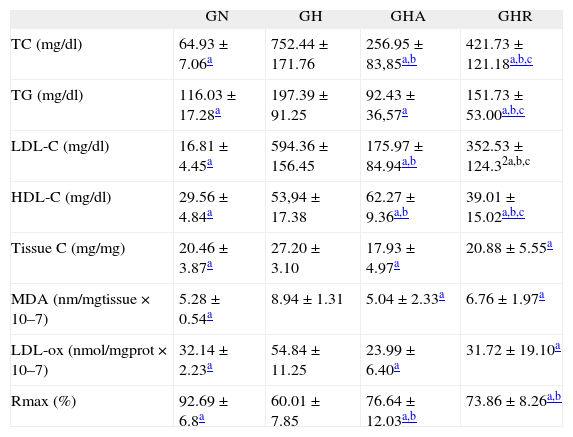
ResultsPlasmatic cholesterol, triglycerides, LDL-C, HDL-C, and LDL-ox as well as tissue cholesterol and MDA increased significantly in GH when compared to GN. When groups GHA and GHR were observed there was a significant reduction of plasmatic cholesterol, triglycerides and LDL-C in relation to GH. However, in GHA there was a greater reduction of these parameters. For HDL-C, there was a significant increase in GHA in relation to GHR. In groups GHR and GHA it was observed a significant reduction in relation to GH in tissue cholesterol content and lipid peroxidation. Figure 1 shows the results of the endothelial function in which a significant dysfunction of relaxation occurred in the GH in relation to the GN and this dysfunction improved significantly in the groups GHR and GHA. There was no significant difference between GHR and GHA in relation to this issue. All numerical results are expressed in Table 1.
Means values and standard deviation for the variables measured in each of the experimental groups
| GN | GH | GHA | GHR | |
| TC (mg/dl) | 64.93 ± 7.06a | 752.44 ± 171.76 | 256.95 ± 83,85a,b | 421.73 ± 121.18a,b,c |
| TG (mg/dl) | 116.03 ± 17.28a | 197.39 ± 91.25 | 92.43 ± 36,57a | 151.73 ± 53.00a,b,c |
| LDL-C (mg/dl) | 16.81 ± 4.45a | 594.36 ± 156.45 | 175.97 ± 84.94a,b | 352.53 ± 124.32a,b,c |
| HDL-C (mg/dl) | 29.56 ± 4.84a | 53,94 ± 17.38 | 62.27 ± 9.36a,b | 39.01 ± 15.02a,b,c |
| Tissue C (mg/mg) | 20.46 ± 3.87a | 27.20 ± 3.10 | 17.93 ± 4.97a | 20.88 ± 5.55a |
| MDA (nm/mgtissue × 10–7) | 5.28 ± 0.54a | 8.94 ± 1.31 | 5.04 ± 2.33a | 6.76 ± 1.97a |
| LDL-ox (nmol/mgprot × 10–7) | 32.14 ± 2.23a | 54.84 ± 11.25 | 23.99 ± 6.40a | 31.72 ± 19.10a |
| Rmax (%) | 92.69 ± 6.8a | 60.01 ± 7.85 | 76.64 ± 12.03a,b | 73.86 ± 8.26a,b |
HDL: high density lipoprotein plasmatic; LDL-C: low density lipoprotein plasmatic; MDA-a: aortic malondialdhyde; LDL-ox: low density lipoprotein plasmatic oxidate; Rmax: maximum relaxament; TC: plasma total cholesterol; TG: triglycerides.
There was no difference among groups GN, GH, GHR and GHA either concerning the curves of concentration-effect with nitroprusside sodium or in the tension of contraction with norepinephrine between all groups.
DiscussionThe cholesterol levels in clinical trials confirmed the correlation between the concentrations of total cholesterol and mortality from coronary heart disease. These tests also showed that the acute coronary event can be prevented and mortality decrease with effective reductions in cholesterol and low density lipoprotein10,11. Thus, many strategies have been used to reduce the levels of lipids and use of statins, inhibitors of HMG-CoA reductase, is the most effective management.
Rosuvastatin has been the most widely used statin as cholesterol lowering, but has not yet been fully evaluated. Based on previous studies with other statins in experimental hypercholesterolemia model12–16, the effects of rosuvastatin according to the endothelium, lipid peroxidation, tissue and plasma cholesterol was measured and compared with the effects of atorvastatin, another well studied statin.
Did not find in literature studies on rosuvastatin in hypercholesterolemic rabbits, which made the creation of an ideal dose difficult. So, being well tolerated, a dose of 2.5mg/day was standardized for each animal. For atorvastatin, the dose was the one already used in another study and is the same as in humans, has proven effective in reducing plasma cholesterol in rabbits13–15. Given the differences between species, especially weight, would be supposed that this dose should be very high for rabbits. However, other statins, experiments have shown that rabbits require the same doses as humans for an equal reduction of plasma cholesterol17–20. Probable differences in metabolism may explain the reason why these high doses are not toxic or lethal to animals.
Both statins determine a significant change in the values of lipid profile, as other study had shown21–23. However, a higher dose of atorvastatin may be responsible for statistically significant differences found in GH, GHR and GHA groups.
Due to high concentrations of LDL remains longer in circulation and can suffer oxidation, LDL-ox is cytotoxic and is involved in endothelial dysfunction24. Therefore, the use of an LDL-C reductor, as statins, is important to reverse the endothelial dysfunction and thus decrease the associated pathological events, particularly atherosclerosis2. The results are interesting when it is observed in the aortic wall. To examine and compare the relationship between the concentrations of cholesterol in the aorta seen in Table 1 may be noted that GH had a significantly greater concentration when compared to GN, GHR and GHA. In groups GHR and GHA was significantly reduced the contents of MDA in the aortic wall and LDL-ox, when compared to GH (Table 1). The same was observed between the concentrations of cholesterol in the aorta tissue. There was no significant difference between groups GHR and GHA on these issues. It was shown that the drugs have a similar effect to reduce the oxidation of LDL-c and cholesterol on the wall of the aorta in these respective doses. Moreover, the effectiveness of statins in reducing lipid peroxidation is known to be related to the reduction of the amount of expression of NADPH oxidase, a real peroxide-generating25.
In rabbits, the process of atherogenesis can be verified after only one week of exposure to the hypercholesterolemic diet with monocytes adhered to the endothelial surface, later, reach the arterial intimae26. Furthermore, it demonstrated the association of hypercholesterolemia with endothelial dysfunction27,28. Statins studies provide solid evidence of benefit in cases of endothelial dysfunction in experimental hypercholesterolemia15,16, by to improve it, and this benefit was attributed to their hypocholesterolemic action. This improvement occurred in rabbits treated with fluvastatin and pravastatin, with the reduction of lipid peroxidation, although there was no reduction in the levels of CT to normal12,14. Thus, in recent years, much attention has been given to so-called pleiotropic effects of statins13. The progress of research in this area has led to the discovery of an important cellular signaling pathway mediated by protein isoprenile, especially geranylgeranylpyrophophate (GGPP), with direct implications for some properties of endothelial cells, including inhibition of eNOS. The expression of GGPP and Rho-dependent system are produced by statins and origin an increased expression of tissue factor28, factor29 of cell proliferation and COX-230. Thus, the clinical benefits in primary and secondary prevention of atherosclerotic disease seem to extend beyond that expected by simple change of lipid profile, suggesting that the experimental and clinical evidence of these pleiotropics effects may be important in stabilizing the atherosclerotic plaque, reduction of oxidative stress, inflammation and recovery of some properties of endothelial cells. Regarding the endothelial function, GH animals were observed to present a significant dysfunction and, in this study, both statins improved almost equally a relaxing close to normal, as shown in figure 1. This shows that significant dyslipidemia causes endothelial dysfunction, which is reversed by statins. This should be related mainly to the reduced levels of CT and particularly LDL-c, which determines the reduction of oxidative stress, reversing endothelial dysfunction in hypercholesterolemic rabbits.
In figure 1, the results of groups GHR and GHA on the GN show that the animals still retain some endothelial dysfunction. This fact indicates that even with the use of drugs is not possible to reach an endothelial function equivalent to GN and this may be related to the values of CT and LDL-c which are still higher than those of GN. However, the results observed in tissue cholesterol, MDA and lipid peroxidation are very close to or lower than those of GN, which generates some controversy, since the reduction of these parameters shall remain responsible for the reversal of endothelial dysfunction and this should reverse itself completely. Therefore, it is possible to suggest that the reversal of endothelial dysfunction is due to changes in arterial tissue than the reduction of CT and LDL-c plasmatic itself. As for the improvement of endothelial dysfunction, there was no statistically significant difference between the two groups. Therefore, the dose used in this study, rosuvastatin is more similar to that of atorvastatin on the reversal of endothelial dysfunction.