We present a study whose objective is to determine whether stimulating the defunctionalized segment of an ileostomy (efferent limb) with a short-chain fatty acid solution prior to reconstruction could improve postoperative results, specifically by decreasing the duration of postoperative paralytic ileus (defined as the time between surgery and the first stool).
Protective ileostomy is a surgical procedure used in colorectal surgery to protect high-risk pelvic anastomoses, not so much from the anastomotic dehiscence itself, but above all from the catastrophic consequences of pelvic sepsis.1
Ileostomies have significant associated morbidity (18%–40% of complications) that sometimes requires readmission due to dehydration and renal failure. Although the effects of their closure are less known, these procedures also present high morbidity (20%) and mortality (2%) rates.2 The most common complication (40% of cases) is postoperative paralytic ileus, which causes delayed initiation of oral intake, abdominal distension, prolonged hospital stay and greater patient discomfort.3 This is explained by the loss of activity of the defunctionalized intestinal segment causing structural changes (villous atrophy, with the consequent loss of intestinal absorptive capacity) and an absence of contractility, causing atrophy of the intestinal muscles that can take up to 6 months to recover.4
This is why all efforts and actions aimed at improving the absorptive and muscular functionality of the intestine excluded before ileostomy reversal should improve postoperative results.
Abriqueta et al.5 present a study in which the morbidity associated with the closure of the ileostomy could be attenuated by previously stimulating the efferent loop with serum and thickener, which reduced postoperative paralytic ileus from 20% to 3%. This point was recently proven in a multicenter randomized study.6
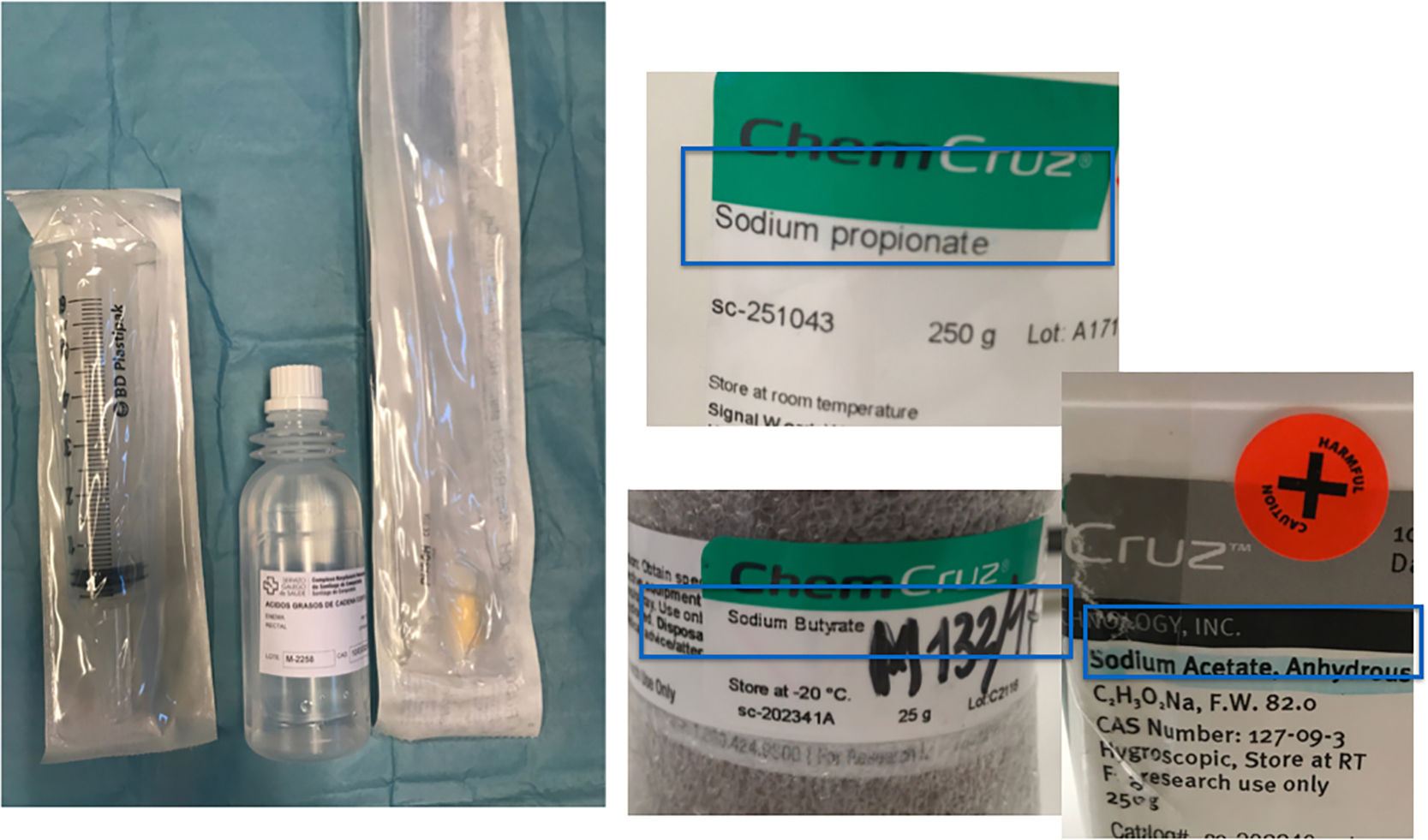
Short-chain fatty acids (SCFA) are known to be the main source of energy for colonocytes. These include acetate, propionate and, most importantly, butyrate: a short-chain fatty acid that favors homeostasis of the colon mucosa by its antioxidant and anti-inflammatory effects, promoting the absorption of sodium and potassium with important antidiarrheal properties7 (Fig. 1).
Given these data, we decided to initiate a study to assess the effects of stimulating the efferent ileostomy loop with SCFA prior to closure. The criterion for patient inclusion in the study was having been ileostomized for rectal cancer; patients with ileostomies for other indications were excluded. All patients who participated followed the same preoperative protocol and signed informed consent for the study (which was requested simultaneously when consent for the ileostomy reversal was given).
A specific nursing protocol was designed for SCFA administration because it must be stored in a refrigerator, then taken out and warmed 30min before use (otherwise, it may cause pain and colic spasms). One week before surgery, the stoma nurse trained the patient or a family member; for this purpose, an instruction sheet was designed and validated, which patients also received at the consultation. Enema vials were also given to the patients at this time to be administered at home the 7 days before the ileostomy was closed.
An 18-Fr Foley catheter was inserted into the efferent loop of the ileostomy, which was then infused with 300mL of SCFA solution (propionate, butyrate and acetate) (Fig. 2).
In all cases, antibiotic prophylaxis was administered and the procedures were performed by a surgeon of the coloproctology unit under general anesthesia. The surgical technique consisted of a peristomal incision and restoration of intestinal continuity with side-to-side mechanical ileo-ileal anastomosis.
In the postoperative period, the stoma therapy nurse/therapist recorded the hours of postoperative ileus, the presence or absence of diarrhea, the need for rescue analgesia, the day on which enteral nutrition was initiated and the length of hospital stay.
At the time of this writing, 16 patients had been included in the stimulation study. The mean time of postoperative paralytic ileus, defined as the number of hours that elapsed until the patient's first stool, was 17h, and the introduction of oral intake was one or two days. The patients were hospitalized for an average of 4 days (compared to 10 for the control subjects in the retrospective series).
Despite the obvious advantages of SCFA in the homeostasis of the intestinal mucosa, especially colonocytes, its clinical oral use is limited due both to its short half-life, as it is metabolized very rapidly, and to its side effects, especially headache, nausea and vomiting. Rectal administration in the form of enemas is better accepted, and in patients with ulcerative proctitis there have been conflicting results, since high doses of butyrate are necessary for prolonged periods of time to maintain its efficacy.8
With the limited sample size of the study, it is not possible to infer statistical studies or scientifically valid conclusions, but there was less need for analgesia and shorter hospital stay than in the retrospective series. Patients who were stimulated and presented a somewhat longer postoperative ileus had undergone ileostomy more than 8 months before reversal. In terms of safety, we have observed no adverse effects either with the technique itself or with the administration of AGCC enemas through the efferent loop.
The functional stimulation of the efferent loop before ileostomy reversal is an easily understood concept, free of adverse effects and associated with benefits in patient recovery. Similar to preparatory and antithrombotic prophylaxis, efferent loop stimulation could be included as part of the protocols for bowel reconstruction.
Please cite this article as: Fernández López F, González López J, Paz Novo M, Ladra González MJ, Paredes Cotoré J. Estimulación preoperatoria del asa eferente de la ileostomía con ácidos grasos de cadena corta. Cir Esp. 2019;97:59–61.