Achalasia is an uncommon oesophageal motor disorder, with a controversial therapeutic management.
AimThe aim of our study was to analyse our experience in the management of achalasia, assessing the impact of minimally invasive surgery, its complications, and its outcomes in the short and medium term.
MethodsA retrospective and descriptive study was designed, including all patients operated on between 1999 and 2010 with the diagnosis of achalasia. Previous diagnostic tests, duration of symptoms, previous non-surgical treatment, surgical approach, associated antireflux intervention, surgical time, and perioperative complications were analysed.
ResultsA total of 50 patients, 24 males, and 26 females, with a mean age of 47 years underwent laparoscopic surgery. The mean duration of the disease was 2 years. Eleven (22%) patients had received endoscopic treatment (1–4 sessions) prior to the surgery, with 100% of symptomatic recurrence. The surgery was accompanied by a Dor fundoplication in 48 patients, and Toupet fundoplication in the remaining 2. The mean surgical time was 123min. There were 9intraoperative complications (5 gastric mucosal perforations, 2 bleeding, 1 liver injury, and 1 aspiration); 4 postoperative complications (3 scapular pain and 1 sub-phrenic collection) were reported. The long-term subjective symptomatic response was excellent/good in 84% of patients, intermediate in 12%, and poor in 4%. The mean follow-up was 28 months.
ConclusionsHeller cardiomyotomy should be the treatment of choice in selected Achalasia patients, because of its short and long term outcomes, and its low morbidity.
La achalasia es un trastorno motor esofágico infrecuente, con un manejo terapéutico controvertido.
ObjetivoAnalizar nuestra experiencia en el manejo de la achalasia, valorando la repercusión de la cirugía mínimamente invasiva, sus complicaciones y resultados a corto y medio plazo.
MétodosEstudio descriptivo reprospectivo incluyendo los pacientes intervenidos desde 1999 a 2010 con diagnóstico de achalasia. Analizamos las pruebas diagnósticas previas, la duración de la sintomatología previa al diagnóstico, las terapéuticas no quirúrgicas previas, la vía de abordaje quirúrgico, el tipo de intervención antirreflujo, la duración y las complicaciones perioperatorias.
ResultadosFueron intervenidos 50 pacientes por vía laparoscópica, 24 varones y 26 mujeres. La edad media fue de 47 años. La media del tiempo de evolución de la enfermedad fue de 2 años. Un 22% de los pacientes habían recibido entre 1 y 4 sesiones de tratamiento endoscópico previo a la cirugía con recidiva sintomática. En 48 se asoció una funduplicatura tipo Dor y en 2, tipo Toupet. La media de tiempo quirúrgico fue de 123 minutos. Se produjeron 9 complicaciones intraoperatorias (5 perforaciones gástricas mucosas, 2 hemorragias, 1 laceración hepática y 1 broncoaspiración) y 4 complicaciones postoperatorias (3 cuadros de dolor escapular y 1 colección subfrénica). El seguimiento medio fue de 28 meses. En el 84% de los pacientes el resultado fue bueno o excelente a largo plazo, en el 12%, regular y en el 4%, malo.
ConclusionesDado el éxito a corto y largo plazo con una mínima morbilidad, la miotomía de Heller laparoscópica es el tratamiento de elección en los pacientes seleccionados para cirugía.
Achalasia is an oesophageal motor disorder whose aetiology is unknown.1 Several hypotheses have been ventured from a physiopathological standpoint; degeneration of inhibitory neurons within the oesophageal myenteric plexus being currently accepted as the origin of the disorder.2
Its incidence is 1–2 cases per 100000individuals/year, it affects both sexes equally and can appear at any age, although it is most common between the third and fifth decades of life. It is characterised by lower oesophageal sphincter (LOS) relaxation failure during swallowing and absence of wavelike contractions along the oesophagus. Histological studies have confirmed absence, atrophy, or disintegration of ganglion cells of the oesophageal myenteric plexus and a decrease in the number of motor nerve fibres at distal oesophagus level.1–3 The main symptom is dysphagia for both solids and liquids, frequently associated with regurgitation (60%–80%) and occasionally with chest pain or weight loss.1,3 Oesophageal manometry is the main diagnostic test for achalasia.3 Treatment is subject to controversy, as there is no consensus as to the indications for each of the treatment options, or to the moment when treatments should be applied.1,4
The current surgical treatment of choice for this condition is laparoscopic Heller cardiomyotomy. This type of approach offers advantages to both the surgeon (better access and visualisation of the cardial area) and to the patient, who receives the benefits of a minimally invasive procedure (less postoperative pain, decrease in postoperative complications especially those involving the surgical wound, and shorter hospital stay and time off work).
The first laparoscopic Heller myotomy was described by Cuschieri in 1991. Since then, the technique has come to be standard, and has undergone changes as technological advances have arrived on the scene. However, since this surgical procedure is not very prevalent, some technical aspects of the surgery are controversial, and there are still disagreements between proponents of different techniques.
ObjectiveThe objective of this study is to examine our hospital's experiences with surgical treatment of achalasia and analyse the effects, complications, and short and long-term results of minimally invasive surgery.
Material and MethodWe designed a descriptive and retrospective study, including all patients diagnosed with achalasia who underwent surgery in our hospital between 1999 and December 2010. The main variable was post-treatment symptom response, with other factors analysed as secondary variables: duration of symptoms prior to diagnosis, prior non-surgical treatments, surgical approach, technical details, length of surgery, and surgical complications.
Statistical AnalysisContinuous quantitative variables are expressed as mean and typical deviation. Discrete quantitative variables are expressed as median and range.
Statistical analysis was performed using the software suite SPSS 11.5.1.
Surgical TechniqueAll patients included in the study underwent laparoscopic surgery performed according to the same surgical technique (with slight variations): Heller myotomy with partial fundoplication.
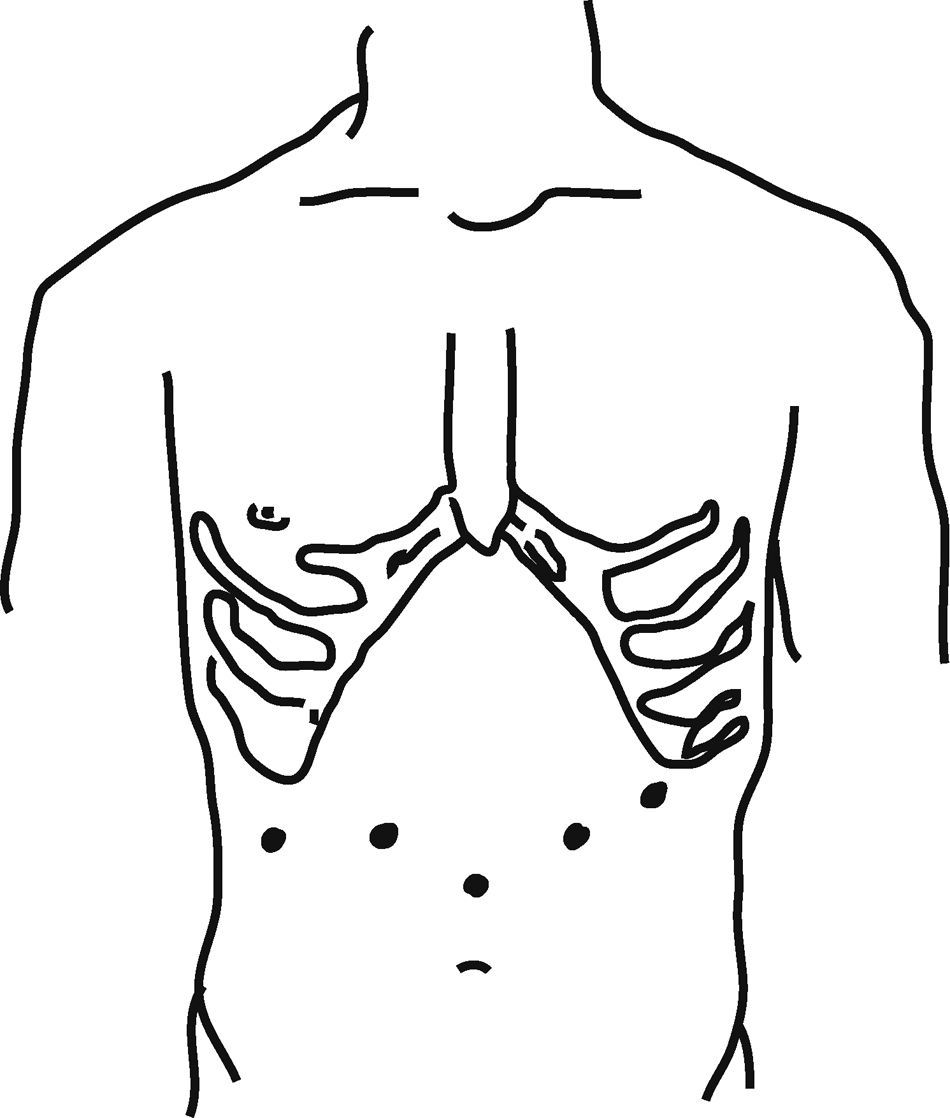
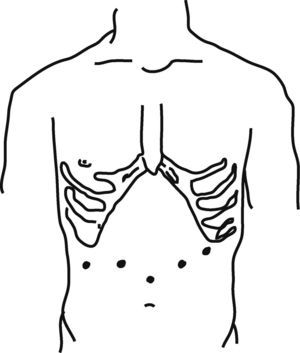
We used modified lithotomy position with reverse Trendelenburg and the legs abducted. Pneumoperitoneum was established using an open technique. The rest of the trocars were placed under direct vision as showed in Fig. 1. A 30° optic was used in all cases.
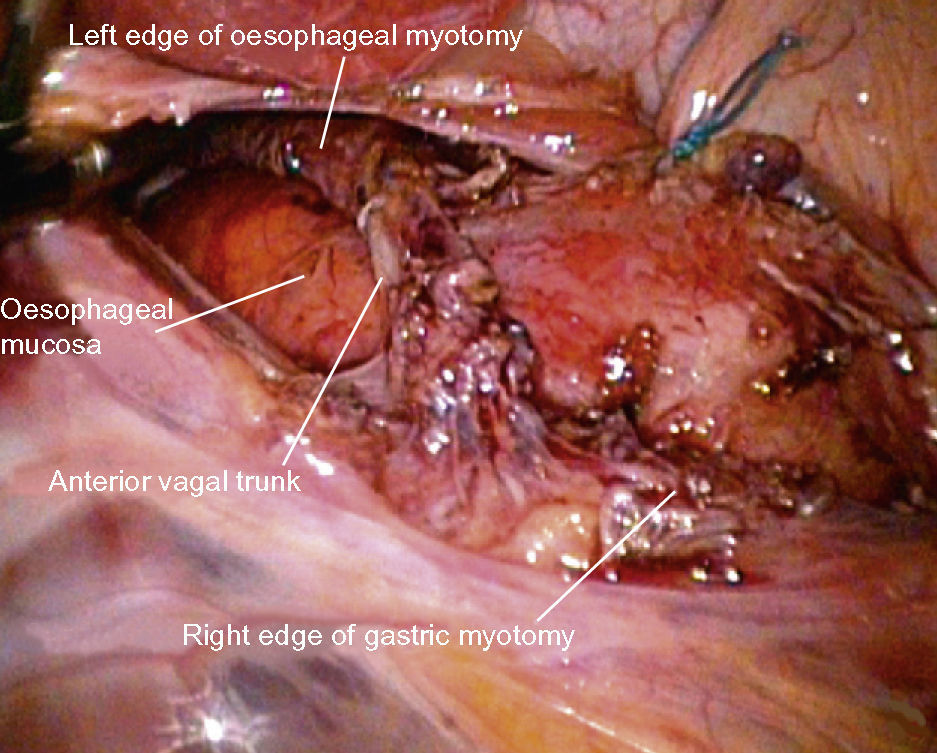
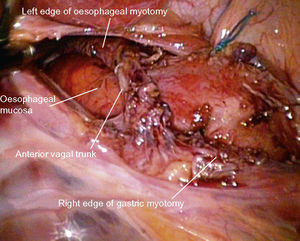
After exposing the anterior face of the oesophagus, we dissected the oesophagogastric junction along 6–8cm in preparation for the myotomy, identifying and respecting the anterior vagal trunk so as to avoid gastroparesis which could lead to postoperative gastro-oesophageal reflux disease (GORD) (Fig. 2).
The oesophagus was circumferentially dissected and the short vessels were divided only in those cases in which we used a Toupet fundoplication. The myotomy was performed using a combination of monopolar scalpel and ultrasonic scalpel, and extended 2–3cm toward the stomach and at least 5cm toward the oesophagus. Where accidental perforation of the mucosa occurred, it was sutured with absorbable monofiliment sutures. Once the myotomy was completed, we always performed a partial fundoplication.
During the study period, 50 patients diagnosed with achalasia underwent surgery in our hospital, all through a laparoscopic approach, which supposes a mean of 4–5 patients per year.
Of these 50 patients, 24 were males and 26 females, and the mean age at the time of surgery was 47 years (range 19–84). The disease duration varied between 4 and 273 months (median: 24 months). A total of 11 patients (22%), all included in the early years of this study, received between 1 and 4 sessions of endoscopic treatment prior to surgery. There were 4 cases of pneumatic dilatation, 5 cases of botulinum toxin injections, and 2 patients received a combination of both treatments; all of these patients experienced symptomatic relapse following the endoscopic treatment.
All patients underwent upper endoscopy, a barium swallow study, and oesophageal manometry prior to the surgery, except for 3 patients who refused this last procedure. One patient with a history of Hodgkin's lymphoma also had a thoraco-abdominal CT and an endoscopic ultrasound study to rule out secondary achalasia. Based on these studies, 37 cases were classified as classic achalasia and 13 as vigourous achalasia.
ResultsWe shall analyse different technical aspects of the surgery. The median length of the myotomy was 6cm at oesophageal level (range 5–8cm) and 2cm at gastric level (range 1.5–3cm). Proper completion of the myotomy and absence of complications were demonstrated in 46 cases. This was done by administering a methylene blue solution by nasogastric tube in 41 patients, and by intraoperative upper endoscopy in 5 patients.
Fundoplication was associated in all cases: 48 patients received an anterior partial fundoplication (Dor) and 2 patients with associated hiatal hernia received a posterior 270° fundopliction (Toupet).
The mean duration of the surgical procedure was 123min. Nine intraoperative complications, all of which were mild, occurred in 6 patients: 5 mucosal perforations that were resolved by suturing the lesions laparoscopically; 2 haemorrhages due to paracardial vein injury; 1 hepatic laceration; and 1 episode of bronchoaspiration during intubation. During the immediate postoperative period, 3 patients complained of scapular pain which lengthened the hospital stay with no major repercussions, and 1 presented fever associated with a left pleural effusion and a small left subphrenic fluid collection which resolved with intravenous antibiotic treatment. There were no associated mortalities during the study period.
All of the procedures were completed laparoscopically with no conversions to laparotomy.
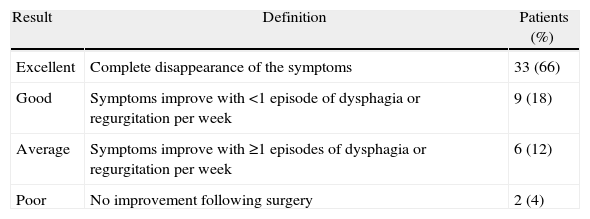
The mean follow-up period after surgery was 28 months. It must be stated that our follow-up appointments were discontinued for most of the patients who remained asymptomatic during the second year after the surgery, after which they were monitored by their primary care centres. With regard to post-treatment symptomatic response, 33 patients had excellent results (defined as total disappearance of symptoms); 9 patients had good results (clinical improvement with dysphagia or regurgitation episodes no more than once per week); 6 patients (12%) had average results (symptoms improved, but dysphagia or regurgitation were present more than once a week); and only 2 patients experienced a poor result. Both patients presented classic achalasia: one patient whose symptoms persisted after the procedure underwent 2 endoscopic dilatations; in the other case, symptoms reappeared 2 years after surgery, and the patient is currently being evaluated for a possible redo procedure (Table 1).
Long-Term Results Following Laparoscopic Heller Myotomy.
| Result | Definition | Patients (%) |
| Excellent | Complete disappearance of the symptoms | 33 (66) |
| Good | Symptoms improve with <1 episode of dysphagia or regurgitation per week | 9 (18) |
| Average | Symptoms improve with ≥1 episodes of dysphagia or regurgitation per week | 6 (12) |
| Poor | No improvement following surgery | 2 (4) |
We did not employ any protocols requiring manometric or other types of studies during the follow-up period.
DiscussionAchalasia is the best-known and best-described primary oesophageal motor disorder. Given that none of its current treatments are capable of producing normal oesophageal function, therapy is palliative and intended to decrease lower oesophageal sphincter pressure.
Drugs, principally calcium channel blockers or long-acting nitrates, are administered to decrease the pressure of the LOS.5 However, their real usefulness in clinical practice is limited; if they do produce any effect, it is transitory and incomplete. At present, they are generally not accepted as an isolated means of treatment; rather, they are used as adjunct treatments or employed prior to another type of therapy.6 In our experience, nearly all of the patients were prescribed some sort of drug to be taken as a palliative measure during the waiting period prior to surgery. We did not analyse the effects of pharmacological treatment since it was not considered as a therapeutic measure by itself.
Injection of botulinum toxin is effective (initial efficacy of 60%–85%) and safe, but the main drawback is that its effect is quite temporary.6,7 For this reason, it is reserved for patients for whom other types of treatment present excessive risks. In our study, 7 patients had received botulinum toxin injections prior to surgery. Although all of them initially reported that their symptoms, particularly dysphagia, had improved, symptoms relapsed a few months later in all cases, and 5 patients had to undergo multiple sessions of endoscopic treatment with the toxin. We found it subjectively more difficult to perform cardiomyotomy on these patients, due to the fibrotic reaction that made it hard to identify the tissue planes of the oesophageal wall at this level. Nevertheless, this perception was in no way reflected by the results.
Another treatment option is pneumatic dilatation, which initially produces excellent or good results in 40%–50% of patients, depending on the study. However, the results obtained in subsequent sessions are not as good, and the procedure is less effective in young patients. Its main short-term complication is perforation, and in the medium to long term, GORD.6,7 Some authors consider it to be the first-line treatment for the condition, preferring it to surgery.
Of the 50 patients included in our study, only 6 had undergone endoscopic pneumatic dilatations. In all of our cases, the symptoms, especially dysphagia, relapsed within a year. However, these data cannot be used to evaluate the efficacy or failure of this endoscopic technique, since our study includes only those patients who underwent a surgical procedure. The logical conclusion is that patients who responded well to endoscopic treatment were not referred for surgery.
However, there are many articles which compare endoscopic dilatation to surgical cardiomyotomy, and they are often difficult to interpret due to patient heterogeneity and the use of different surgical techniques. A recent systematic review by Campos et al.4 compares endoscopic injection of botulinum toxin, endoscopic dilatation, and minimally invasive surgery. It concludes that cardiomyotomy appears to be the most effective technique, with good immediate results (success rates of 80%–90%) and medium to long term results, as it provides more relief from symptoms and has a low complications index. On the other hand, the recently published randomised study by Boeckxstaens et al.8 comparing endoscopic dilatation with laparoscopic Heller myotomy does not show significant differences with regard to therapeutic success for a 2-year follow-up period.
The use of minimally invasive surgical techniques has certainly contributed to the good result rate of the surgery; beyond any debate, laparoscopy has come to be the approach of choice for treating achalasia, above open surgery and thoracoscopy. Thorascopic Heller myotomy is a viable option, but it is associated with a longer hospital stay, increased short-term discomfort and increased GORD in the medium to long term.9 We have no experience with this type of approach in our hospital.
From both the patient's and the surgeon's point of view, laparoscopic Heller myotomy offers obvious advantages when compared to a laparotomic approach. On the one hand, hiatal dissection is simpler if performed by laparoscopy due to offering better access and exposure of the operating field than would be the case with classic laparotomy. On the other hand, the laparoscopic Heller myotomy grants patients all of the advantages associated with minimally invasive surgery: less postoperative discomfort, shorter hospital stay, and near elimination of complications related to incisions in the abdominal wall.
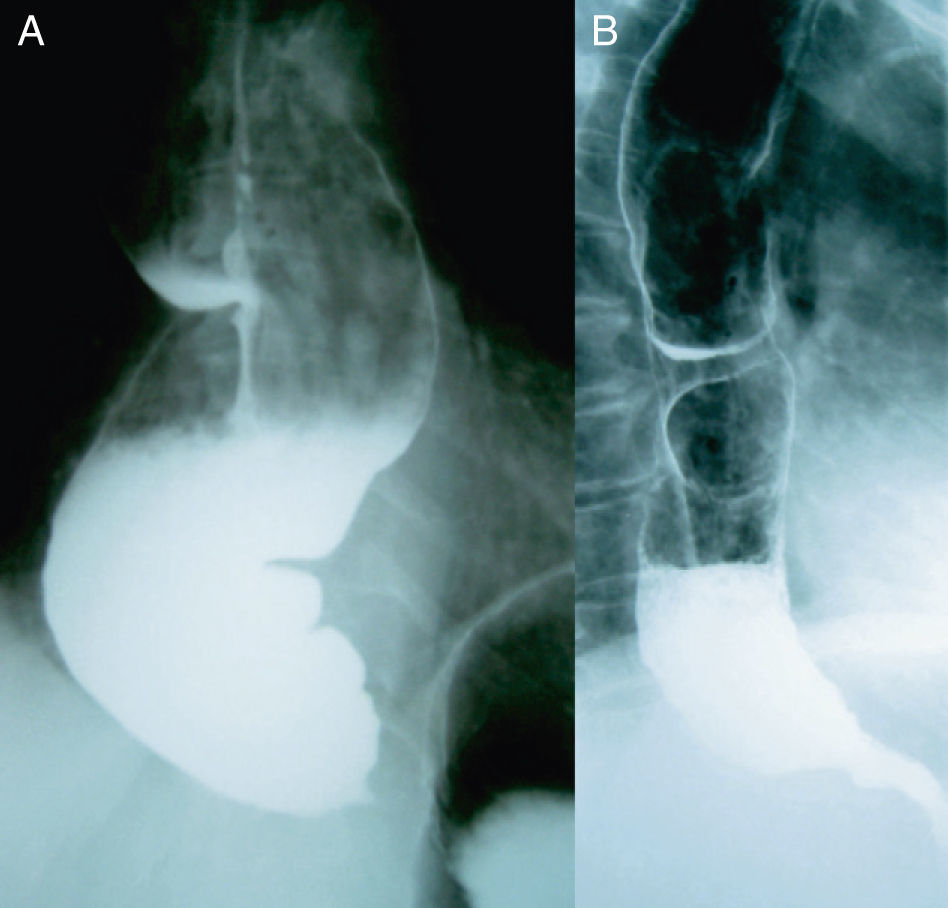
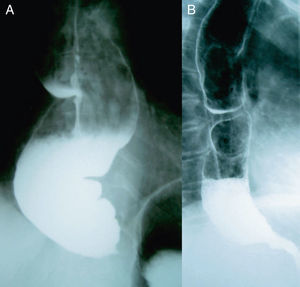
It seems that the success of a Heller myotomy may be compromised in cases with a long disease duration and oesophageal dilation of more than 4cm; here, some authors even point to oesophagectomy as the first treatment option. However, in our experience, patients with sigmoid oesophagus have obtained good results from cardiomyotomy (Fig. 3). Considering the significant morbidity and mortality associated with oesophagectomy, we believe that the Heller procedure is the treatment of choice, regardless of the degree of oesophageal dilation.
Associating an anti-reflux technique has been shown to be effective in preventing postoperative GORD.10,11 Debate still exists over what anti-reflux technique should be employed. While the Nissen fundoplication achieves good control over GORD, it seems to be associated with significantly higher rates of dysphagia recurrence than in the case for partial fundoplications such as the Dor or Toupet procedures.11 The latter two techniques offer superimposable results with respect to reflux control and the reappearance of dysphagia. In our study, the technique applied to 96% of the patients was Dor anterior partial fundoplication. We tend to use this technique rather than other partial fundoplications such as the Toupet because the myotomy area remains covered by the fundus, thereby minimising the consequences of any potential mucosal microperforations, and because it requires a smaller dissection and preserves the natural posterior anchors of the hiatus.
The length of the myotomy has been shown to be directly correlated to the relapse of symptoms, especially dysphagia.12 In 50% of the patients in our study, the myotomy measured 6cm along the oesophageal stretch and 2cm along the gastric stretch, and we obtained good or excellent results in 84% of the cases. Nevertheless, we cannot analyse individually the impact of myotomy length on surgical success since we do not dispose of a control group.
Another fundamental problem when analysing success or failure in these types of procedure is how to define “success”. Different questionnaires have been described, which patients use to evaluate the perceived degree of symptom improvement following myotomy. As a result, and as we see in our study, the results are quite subjective.
Some groups have established postoperative protocols for patients having undergone a myotomy that calls for manometric studies or other tests such as barium swallow tests.13 Although our group does not currently follow a standard procedure for running these types of tests during follow-up, the idea does seem interesting, as it would allow us to analyse the correlation between clinical success and results from the complementary tests. In our opinion, however, technique success or failure should be evaluated on the fundamental basis of the patient's perception. To that end, it would be extremely useful to have the patient complete the same questionnaire before and after surgery in order to provide a more conclusive comparative analysis.
Few studies examine the long-term results of laparoscopic Heller myotomy. In 2006, Csendes et al.13 published a study of 67 patients who were monitored for more than 190 months which showed progressive clinical decline with respect to the good initial results. However, this study does not include patients who underwent surgery using a laparoscopic approach. The prospective study by Chen14 including 125 patients who all underwent laparoscopic surgery, and other recent studies, show very good long-term results (follow-up >5 years). In our experience, although the follow-up period is shorter and the sample size smaller, we have not observed results growing worse with the passage of time.
Studies containing more patients, and covering a longer follow-up time, would be necessary to provide a better description of long-term results and influential factors following a laparoscopic Heller myotomy.
In recent years, new endoscopic techniques have been developed as experimental treatments for achalasia, and one remarkable technique is transoral endoscopic myotomy.15 Based on studies in a porcine model, Perreta et al.16,17 conclude that transoral endoscopic myotomy is a feasible and safe technique, and indicate it as a possible new strategy for treating achalasia in certain patients.
They also describe the technique in association with intraluminal fundoplication17 as a NOTES technique. To conclude, given achalasia's low incidence rate, it should be treated in centres of reference by multidisciplinary teams possessing both the necessary resources and experience for handling such procedures and their possible complications. The most appropriate treatment will depend on multiple factors, such as the patient's surgical risk, age, or symptom intensity. However, considering our own results and those from other studies we have found,18,19 laparoscopic Heller myotomy associated with an anti-reflux technique is the treatment of choice for patients selected for surgery.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Lesquereux Martínez L, et al. Papel del tratamiento quirúrgico por vía laparoscópica de la achalasia de cardias: ana¿lisis de 50 casos. Cir Esp. 2011;89:657–62.