Bronchogenic cysts develop between the third and seventh weeks of intrauterine life and are due to abnormalities in the embryological development of the primitive intestine and the tracheobronchial tree. Their typical location is mediastinal, while retroperitoneal cysts are very infrequent and the retrorectal location is exceptional.1
We present the case of a 32-year-old patient who was admitted for hypogastric abdominal pain and right iliac fossa pain over the past 6 months, whose intensity had increased in the last month. There was no associated fever or any other symptoms. Upon examination, the patient presented discomfort in the hypogastrium and right iliac fossa, with no peritoneal irritation or palpated masses.
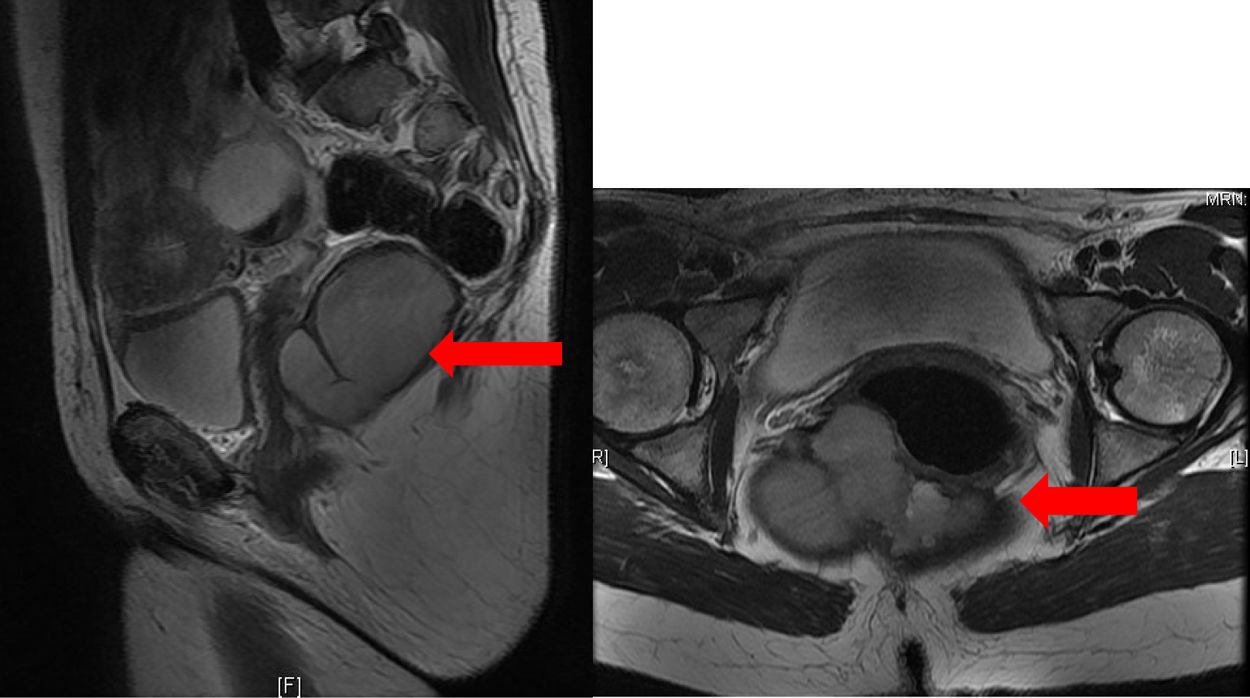
Lab work showed no findings of interest. Abdominal tomography revealed a right pararectal septated cystic mass measuring 10×6cm. In view of the findings, the patient was admitted to hospital and the study was completed with an MRI, which showed a multiloculated presacral cystic mass measuring 10.3×7.8×5.7cm in diameter, suggestive of retrorectal cystic hamartoma or tailgut cyst (Fig. 1).
Given the possible complication of this lesion, the possibility of degeneration and the patient’s symptoms, laparoscopic surgery was performed in which a large cystic mass was observed that extended retrorectally from the mid-rectum to the levator ani muscles without depending on them. We conducted a difficult dissection of the entire lesion, during which an incidental lesion of the rectum measuring 1.5cm occurred, which was sutured endoanally. Finally, the cystic lesion was removed and a protective ileostomy was performed.
The anatomic pathology study revealed a cavitary lesion lined by respiratory-type epithelium (cylindrical pseudostratified ciliated with goblet cells), which was compatible with a bronchogenic cyst.
The patient was discharged on the sixth postoperative day and is currently awaiting stoma closure.
Bronchogenic cysts are caused by an abnormal development of the ventral diverticulum of the tracheobronchial tree and are usually located in the lung parenchyma or mediastinum.2
When they are totally separated from the tracheobronchial tree, they can migrate to atypical locations, specifically to the retroperitoneum in 0.03%2 of cases. At this level, the peripancreatic location is the most frequent (28% of cases3), while the retrorectal location is very unusual.
The incidence of bronchogenic cysts is similar in both sexes. Mean patient age is around 40 years, and mean cyst size is 6cm.4
Most cases are diagnosed incidentally.1 However, these cysts can bleed, perforate, compress adjacent structures due to their growth, and even become malignant.5
Tomography and magnetic resonance imaging will be the fundamental tests used for diagnosis, but if these lesions are found at the biliary or pancreatic level, it is advisable to carry out endoscopic ultrasound and fine-needle aspiration of the lesion.3
The differential diagnosis should include a variety of entities, such as cystic hamartomas, sacrococcygeal teratoma, anterior sacral meningocele, rectal duplication cysts, and rectal leiomyosarcomas.6
Treatment is surgical to control symptoms and avoid the risk of malignization.3 The recommended surgical approaches are sacrococcygeal for lesions located below S4, transanal in those smaller than 4cm, or abdominal in large lesions and above S3.7 Although the first 2 are the most popular, the laparoscopic abdominal approach has also been described.3,8
Histological analysis will show cartilage and bronchial glands with seromucosal content.9
In the present case, the initial imaging diagnosis was cystic hamartoma, a very rare benign tumor. To avoid the risk of dissemination in the case of malignant disease, we decided not to perform ultrasound-guided needle aspiration of the lesion. Although it is true that the laparoscopic approach has not been widely described in the literature, we chose this as it was a large lesion located above the levator ani muscles in a young patient in whom we did not want to alter the perineal muscles.
We believe that information about a rare disease, in an exceptional location, with risk of malignization, and the experience of its laparoscopic treatment is important for colorectal surgeons.
Please cite this article as: García-Romera Á, Tuñón-Féquant C, Díaz-Pérez B, Bravo-Gutiérrez A, Alarcó-Hernández A. Quiste broncogénico retrorrectal. Cir Esp. 2021;99:157–159.