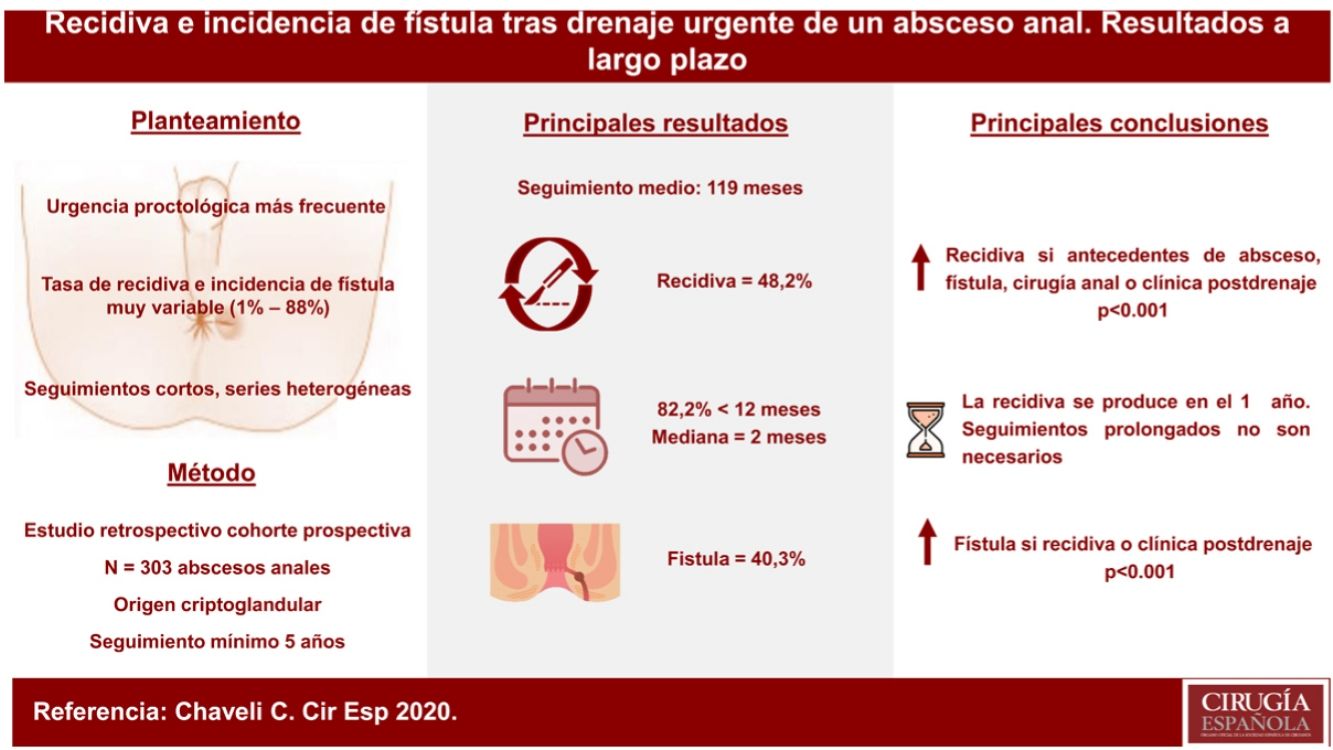
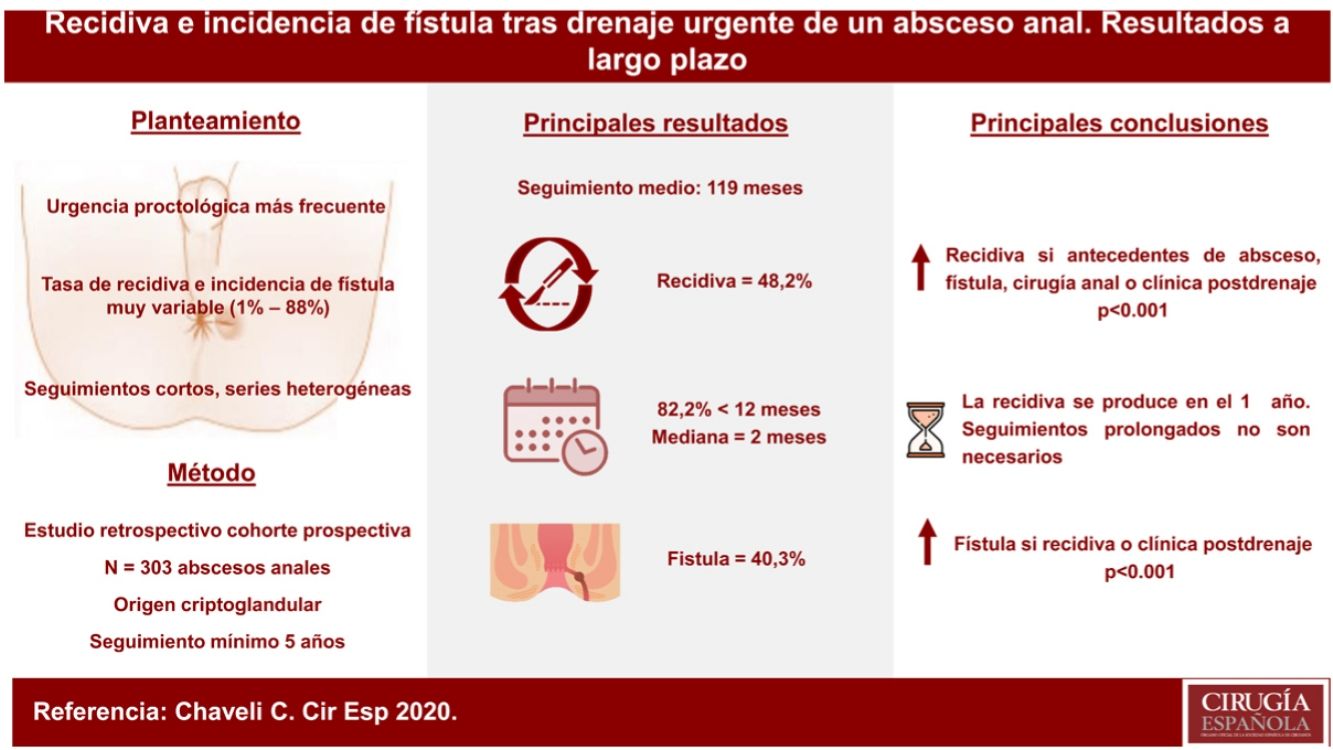
Anal abscess is the most frequent urgent proctological problem. The recurrence rate and reported incidence of fistula after drainage and debridement of an anal abscess is widely variable. The objective of this study is to analyse the long-term recurrence rate and the incidence of fistula after drainage and urgent debridement of an anal abscess.
MethodsRetrospective observational study of a prospective cohort with anal abscess of cryptoglandular origin. All patients (n = 303) were evaluated two months and one year after the intervention. At the 5th year, all the medical records were reviewed and a telephone call or appointment was made for an assessment if necessary. Specific antecedents of anal pathology, abscess characteristics, time and type of recurrence, presence of symptoms in the first revision and presence of clinical and/or ultrasound fistula were recorded.
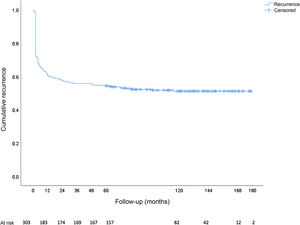
ResultsMean follow-up 119.7 months. Recurrence rate 48.2% (82.2% in the first year). Two hundred twenty-two ultrasounds performed. Incidence of ultrasound fistula: 70% symptomatic vs. 2.4% asymptomatic (p < 0.001). Global incidence of fistula 40.3%. The history of anal pathology and the presence of symptoms in the postoperative review significantly increase the possibility of recurrence (p < 0.001). The fistula is statistically more frequent if the abscess recurs (p < 0.001).
ConclusionAfter drainage and debridement of an anal abscess, half of the patients relapse and 40% develop fistula especially in the first year, so longer follow-ups are not necessary. Endoanal ultrasound for the evaluation of the presence of fistula is highly questionable in the absence of signs or symptoms.
El absceso anal es el problema proctológico urgente más frecuente. La tasa de recidiva y la incidencia de fístula publicada tras el drenaje y desbridamiento de un absceso anal es ampliamente variable. El presente estudio tiene como objetivo analizar la tasa de recurrencia y la incidencia de fístula a largo plazo tras el drenaje y desbridamiento urgente de un absceso anal.
MétodosEstudio observacional retrospectivo de una cohorte prospectiva con absceso anal de origen criptoglandular. Todos los pacientes (n = 303) fueron evaluados a los dos meses y al año de la intervención. Al quinto año se revisaron todas las historias clínicas y se llamó telefónicamente o se citó en consulta para valoración. Se registraron los antecedentes específicos de patología anal, características del absceso, momento y tipo de la recidiva, presencia de sintomatología en la primera revisión y presencia de fístula clínica y/o ecográfica.
ResultadosSeguimiento medio de 119,7 meses. Tasa de recidiva 48,2% (82,2% en 1er año). Doscientas veintidós ecografías realizadas. Incidencia de fístula ecográfica: 70% sintomáticos vs. 2,4% asintomáticos (p < 0,001). Incidencia global de fístula 40,3%. Los antecedentes de patología anal y la presencia de clínica en la revisión postoperatoria aumentan significativamente la posibilidad de recidiva (p < 0,001). La fístula es estadísticamente más frecuente si el absceso presenta recurrencia (p < 0,001).
ConclusionesTras el drenaje y desbridamiento de un absceso anal la mitad de los pacientes recidivan y un 40% desarrollan fístula. Seguimientos mayores de un año no son necesarios. La ecografía endoanal para la evaluación de la presencia de fístula es muy cuestionable en ausencia de signos o síntomas.
Anal abscess is one of the most frequent reasons for urgent consultation for surgeons, while it is also the proctological problem that most commonly requires urgent surgical treatment1. In general, the treatment of anal abscess is surgical2, with drainage and debridement (DD) being the most widespread technique3.
After DD, the published incidence of recurrence is quite varied (1.6%-88%)4, although the overall rate is around 50%, which may be in the form of a new abscess or chronic suppuration.
Insufficient drainage and the undiagnosed presence of an underlying fistula have been proposed as the main causes of recurrence5,6. Other risk factors include age younger than 40 years, male sex, non-cryptoglandular origin, obesity, history of previous abscess, and intersphincteric or ischiorectal abscesses.
The diagnosis of anal fistula is eminently clinical, but the first-line complementary examination is endoanal ultrasound7. Currently, there are no clear recommendations on the follow-up time and the need to study the possible underlying fistula after urgent drainage of an anal abscess.
There are few series published on fistula development and recurrence that only include patients with anal abscess of cryptoglandular origin, treated with DD alone. The have few patients, short follow-up times and disparate recurrence rates8–12.
This study analyzes the long-term results in terms of recurrence and incidence of fistula after urgent DD of anal abscess.
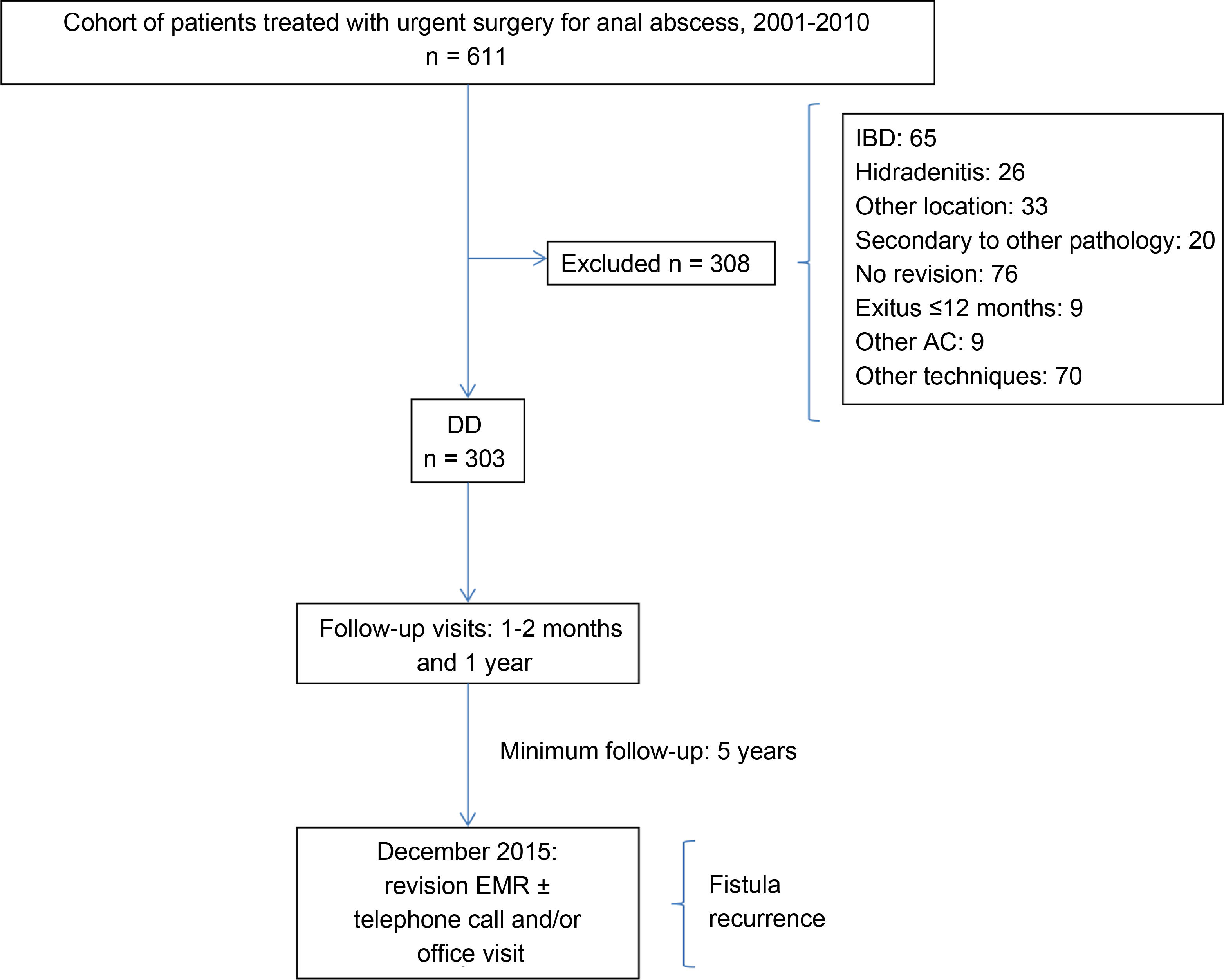
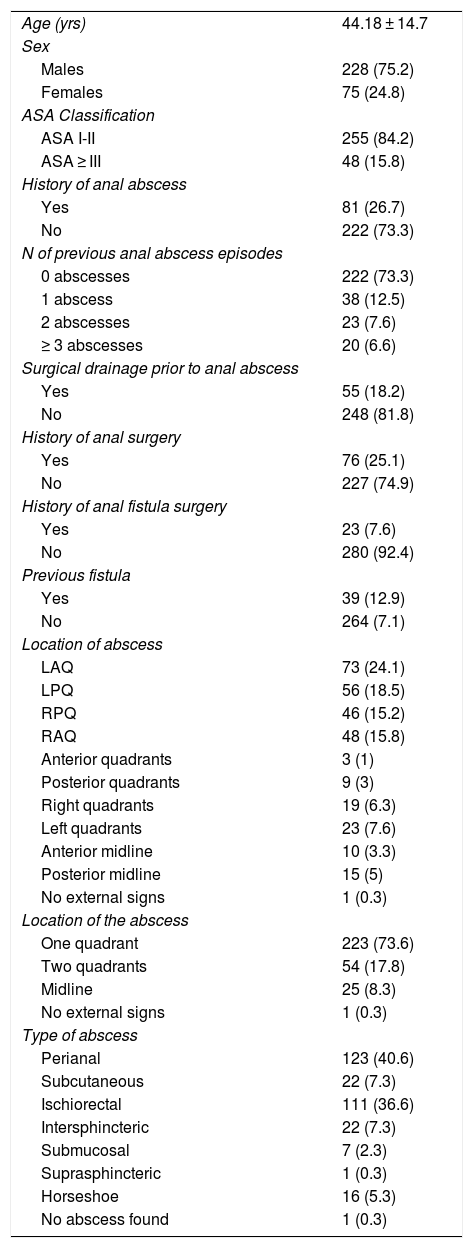
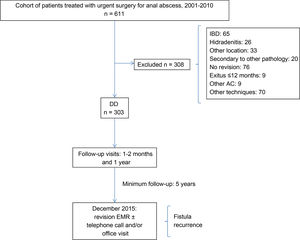
MethodsThis is a retrospective study of a consecutive, prospective cohort. Between January 2001 and December 2010, 611 patients underwent anal abscess surgery at our hospital. All patients older than 15 years of age who underwent urgent surgery for anal abscess of cryptoglandular origin and who underwent DD exclusively in the operating room were included in the study. We excluded: patients with a previous diagnosis or during follow-up of inflammatory bowel disease (IBD) or hidradenitis; those with abscesses secondary to other pathologies; gluteal or pilonidal location; patients who did not attend the postoperative check-ups in the outpatient clinic; patients who died during the first year of follow-up; patients from other Autonomous Communities of Spain (due to the difficult follow-up); and those who underwent other anal procedures during urgent DD. Thus, 50.4% (308 patients) were excluded, resulting in a final study cohort of 303 patients (75.2% male) with a mean age of 44.1 ± 14.7 years. The characteristics of the cohort are shown in Table 1.
Cohort characteristics.
| Age (yrs) | 44.18 ± 14.7 |
| Sex | |
| Males | 228 (75.2) |
| Females | 75 (24.8) |
| ASA Classification | |
| ASA I-II | 255 (84.2) |
| ASA ≥ III | 48 (15.8) |
| History of anal abscess | |
| Yes | 81 (26.7) |
| No | 222 (73.3) |
| N of previous anal abscess episodes | |
| 0 abscesses | 222 (73.3) |
| 1 abscess | 38 (12.5) |
| 2 abscesses | 23 (7.6) |
| ≥ 3 abscesses | 20 (6.6) |
| Surgical drainage prior to anal abscess | |
| Yes | 55 (18.2) |
| No | 248 (81.8) |
| History of anal surgery | |
| Yes | 76 (25.1) |
| No | 227 (74.9) |
| History of anal fistula surgery | |
| Yes | 23 (7.6) |
| No | 280 (92.4) |
| Previous fistula | |
| Yes | 39 (12.9) |
| No | 264 (7.1) |
| Location of abscess | |
| LAQ | 73 (24.1) |
| LPQ | 56 (18.5) |
| RPQ | 46 (15.2) |
| RAQ | 48 (15.8) |
| Anterior quadrants | 3 (1) |
| Posterior quadrants | 9 (3) |
| Right quadrants | 19 (6.3) |
| Left quadrants | 23 (7.6) |
| Anterior midline | 10 (3.3) |
| Posterior midline | 15 (5) |
| No external signs | 1 (0.3) |
| Location of the abscess | |
| One quadrant | 223 (73.6) |
| Two quadrants | 54 (17.8) |
| Midline | 25 (8.3) |
| No external signs | 1 (0.3) |
| Type of abscess | |
| Perianal | 123 (40.6) |
| Subcutaneous | 22 (7.3) |
| Ischiorectal | 111 (36.6) |
| Intersphincteric | 22 (7.3) |
| Submucosal | 7 (2.3) |
| Suprasphincteric | 1 (0.3) |
| Horseshoe | 16 (5.3) |
| No abscess found | 1 (0.3) |
LAQ: left anterior quadrant; LPQ: left posterior quadrant; RPQ: right posterior quadrant; RAQ: right anterior quadrant.
Age is presented as mean and standard deviation. The rest as frequency and percentage.
Regarding the surgical technique, with the patient in the lithotomy position and preferably under spinal anesthesia, the incision was made at the point of maximum fluctuation, as close as possible to the external anal margin. If the patient presented a spontaneous drainage hole, this was enlarged by blunt dissection. Debridement was performed and the cavity was washed with saline solution and diluted povidone-iodine. According to the preferences of the responsible surgeon. H2O2 was instilled into the cavity to try to identify a possible internal orifice. A drain tube was inserted through the wound and affixed with a suture at the edge of the wound. In large abscesses and those with horseshoe extension, more than one drain was used when necessary, or sometimes a Pezzer catheter was inserted to perform lavage. The drain was removed after the second postoperative day, depending on the evolution of the process. Intersphincteric and suprasphincteric abscesses secondary to cranial extension from the intersphincteric space were drained endoanally or transrectally. The remainder were drained perianally/cutaneously. No mechanical preparation of the rectum with enema was performed. Preoperative antibiotic prophylaxis was established according to the prophylaxis protocol approved by the Infections Commission at our hospital (1.5 g metronidazole and 1 g cefotaxime). At discharge, patients were prescribed oral analgesics (1 g paracetamol every 8 h), laxatives (10 g lactulose in packets), antithrombotic prophylaxis (40 g enoxaparin every 24 hours for 10 days) and warm water sitz baths until completely healed, with no dietary restrictions.
All patients were seen in the outpatient clinic between the first and second postoperative month and one year after surgery to assess the presence of symptoms (suppuration, pain, palpation of the tumor or trajectory, persistence of the fistulous orifice, open drainage wound). Those with some type of symptoms at the first follow-up visit or with recurrence or suspicion or diagnosis of fistula were periodically monitored in the outpatient consultation. In December 2015, with a minimum follow-up of five years, the medical records of all patients were reviewed to detect possible episodes of recurrence or development of fistula. In cases of doubt, patients were contacted by telephone, or an appointment was made for evaluation. The flow chart is shown in Fig. 1.
Recurrence was defined as the presence of abscess or chronic suppuration in the intervention area at any time during follow-up. The definitive diagnosis of fistula was established by physical examination and/or endoanal ultrasound. The clinical diagnosis of anal fistula was determined by suppuration after the second month of follow-up. The ultrasound diagnosis was made when, after instillation of H2O2 through the external orifice of the fistula, the trajectory and the internal fistulous orifice were identified. Complex fistulae presented any of the following: involvement >30% of the external sphincter (medium-high transsphincteric and suprasphincteric), anterior location in women, multiple trajectories, recurrent fistulae, patients with previous incontinence.
We recorded the patient history of anal pathology, characteristics of the abscess (location and type), time of appearance and type of recurrence (abscess/suppuration), presence of symptoms during the first follow-up visit, and the presence and type of fistula in the ultrasound, when performed.
For the statistical analysis, we used the SPSS v.25® program (IBM Statistics®, Chicago, Illinois, USA). The quantitative variables have been expressed as number of cases and percentages, and according to their mean and standard deviation (SD) if they followed a normal distribution, or according to their median and range if they followed a non-normal distribution. The cumulative incidence of recurrence has been analyzed using the Kaplan-Meier method. A univariate study was carried out using the chi-squared test or Student’s t test, as appropriate, considering P-values <.05 statistically significant. With the clinically relevant variables (statistically significant or with a value close to statistical significance in the univariate study), a multivariate study was performed to minimize possible confounding factors between variables and establish independent risk factors. The results of this analysis have been expressed according to the odds ratio (OR) with its 95% confidence interval (95% CI), and P-values <.05 were considered statistically significant.
ResultsThe mean follow-up of the cohort was 119.7 ± 36.3 months.
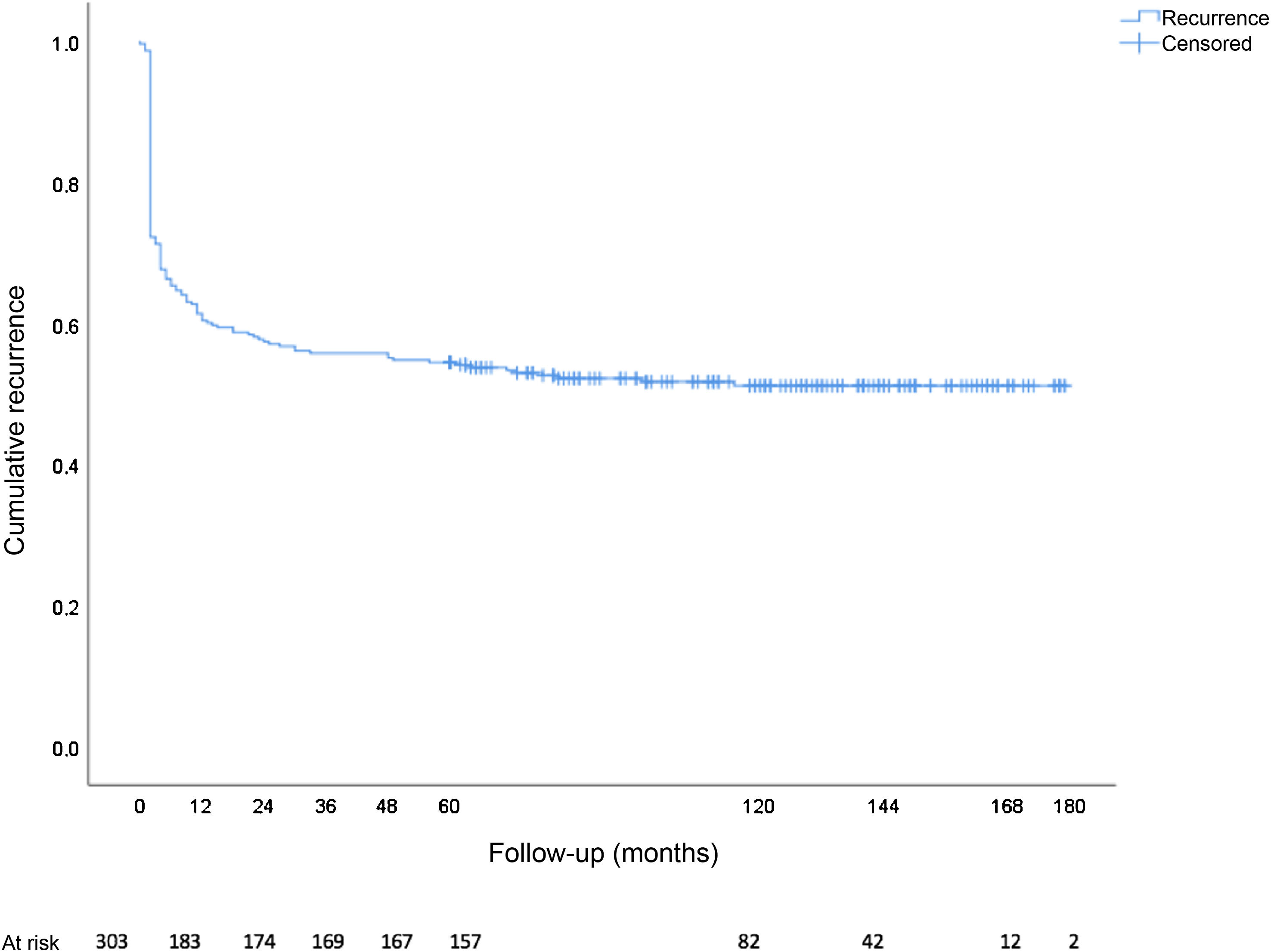
In total, there were 146 recurrences (48.2%), 89 of which (60.9%) were in the form of chronic suppuration, and 82.2% (120 cases) occurred during the first year of follow-up. The total cumulative incidence of recurrence (Kaplan-Meier) is shown in Fig. 2. The median onset of recurrence was two months (range 0-115 months, mean 10.7 ± 19.8 months). Out of the 51 asymptomatic patients who presented recurrence, 54.9% (28 patients) did so in the first year of follow-up and 70.6% (36 patients) during the first two years. In contrast, out of the 95 symptomatic patients who relapsed, 96.8% (92 patients) did so in the first 12 months. Recurrence as abscess was more frequent in asymptomatic patients (77.2% vs 22.8%; chi-square P < .001), while recurrence in the form of chronic suppuration was more frequent in symptomatic patients (92.1% vs 7.9%; chi-square P < .001).
Ultrasound scans were performed in 222 patients (73.3%): 84 (37.8%) asymptomatic and 138 (62.2%) symptomatic. The diagnosis of fistula was confirmed in 98 cases (44.1%). Ultrasound confirmed the diagnosis in 69.6% (96 patients) in cases with symptoms and/or a compatible physical examination, but only in 2.4% (2 patients) of asymptomatic patients; 45% of the fistulae diagnosed by ultrasound were classified as complex.
The total cumulative incidence of fistula (with and without ultrasound) was 40.3% (122/303 patients). The diagnosis of clinical and/or ultrasound fistula was significantly higher in patients with suppuration-type recurrence than with abscess-type recurrence (100% vs 24.6%; P < .001).
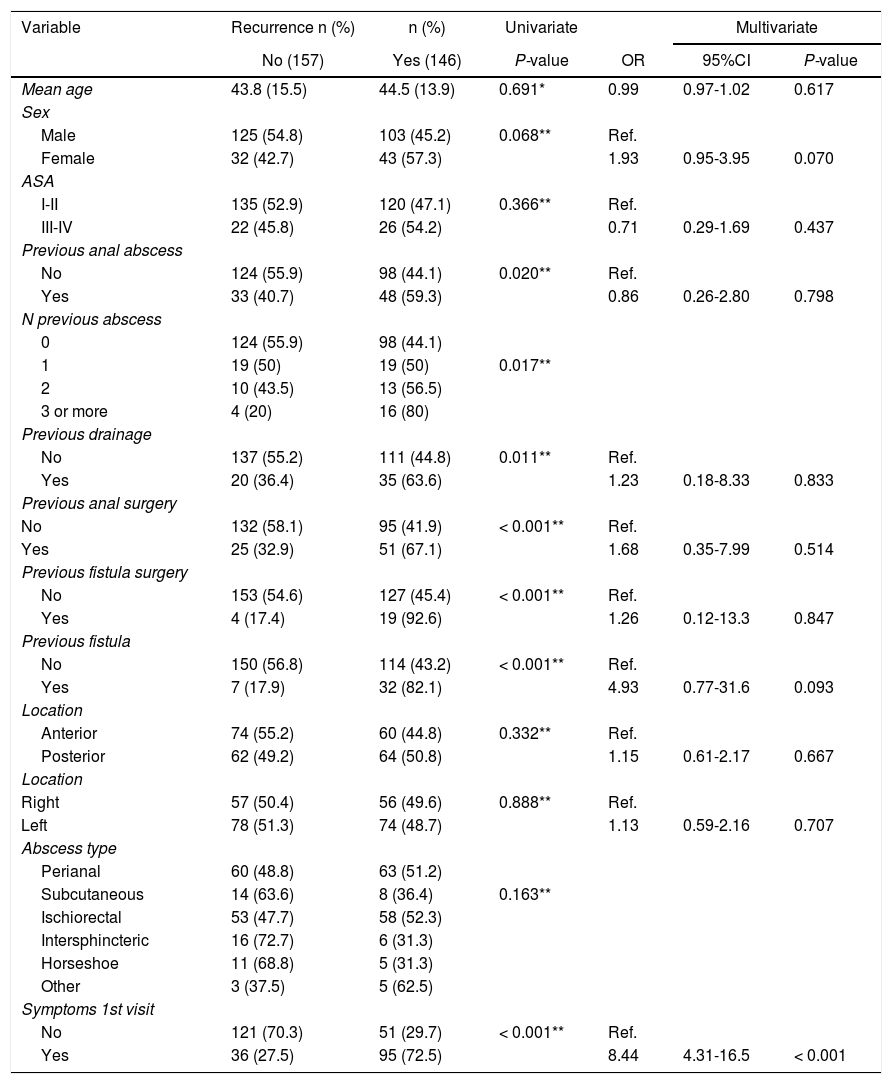
Recurrence showed a statistically significant association with a history of abscess and fistula, history of anal surgery (abscess drainage and fistula surgery) and presence of symptoms in the postoperative review in the univariate analysis. In the multivariate analysis, the presence of symptoms at the follow-up visit was identified as an independent risk factor for recurrence, as well as a trend towards it in females and with a history of anal fistula (Table 2).
Uni- and multivariate analysis according to recurrence.
| Variable | Recurrence n (%) | n (%) | Univariate | Multivariate | ||
|---|---|---|---|---|---|---|
| No (157) | Yes (146) | P-value | OR | 95%CI | P-value | |
| Mean age | 43.8 (15.5) | 44.5 (13.9) | 0.691* | 0.99 | 0.97-1.02 | 0.617 |
| Sex | ||||||
| Male | 125 (54.8) | 103 (45.2) | 0.068** | Ref. | ||
| Female | 32 (42.7) | 43 (57.3) | 1.93 | 0.95-3.95 | 0.070 | |
| ASA | ||||||
| I-II | 135 (52.9) | 120 (47.1) | 0.366** | Ref. | ||
| III-IV | 22 (45.8) | 26 (54.2) | 0.71 | 0.29-1.69 | 0.437 | |
| Previous anal abscess | ||||||
| No | 124 (55.9) | 98 (44.1) | 0.020** | Ref. | ||
| Yes | 33 (40.7) | 48 (59.3) | 0.86 | 0.26-2.80 | 0.798 | |
| N previous abscess | ||||||
| 0 | 124 (55.9) | 98 (44.1) | ||||
| 1 | 19 (50) | 19 (50) | 0.017** | |||
| 2 | 10 (43.5) | 13 (56.5) | ||||
| 3 or more | 4 (20) | 16 (80) | ||||
| Previous drainage | ||||||
| No | 137 (55.2) | 111 (44.8) | 0.011** | Ref. | ||
| Yes | 20 (36.4) | 35 (63.6) | 1.23 | 0.18-8.33 | 0.833 | |
| Previous anal surgery | ||||||
| No | 132 (58.1) | 95 (41.9) | < 0.001** | Ref. | ||
| Yes | 25 (32.9) | 51 (67.1) | 1.68 | 0.35-7.99 | 0.514 | |
| Previous fistula surgery | ||||||
| No | 153 (54.6) | 127 (45.4) | < 0.001** | Ref. | ||
| Yes | 4 (17.4) | 19 (92.6) | 1.26 | 0.12-13.3 | 0.847 | |
| Previous fistula | ||||||
| No | 150 (56.8) | 114 (43.2) | < 0.001** | Ref. | ||
| Yes | 7 (17.9) | 32 (82.1) | 4.93 | 0.77-31.6 | 0.093 | |
| Location | ||||||
| Anterior | 74 (55.2) | 60 (44.8) | 0.332** | Ref. | ||
| Posterior | 62 (49.2) | 64 (50.8) | 1.15 | 0.61-2.17 | 0.667 | |
| Location | ||||||
| Right | 57 (50.4) | 56 (49.6) | 0.888** | Ref. | ||
| Left | 78 (51.3) | 74 (48.7) | 1.13 | 0.59-2.16 | 0.707 | |
| Abscess type | ||||||
| Perianal | 60 (48.8) | 63 (51.2) | ||||
| Subcutaneous | 14 (63.6) | 8 (36.4) | 0.163** | |||
| Ischiorectal | 53 (47.7) | 58 (52.3) | ||||
| Intersphincteric | 16 (72.7) | 6 (31.3) | ||||
| Horseshoe | 11 (68.8) | 5 (31.3) | ||||
| Other | 3 (37.5) | 5 (62.5) | ||||
| Symptoms 1st visit | ||||||
| No | 121 (70.3) | 51 (29.7) | < 0.001** | Ref. | ||
| Yes | 36 (27.5) | 95 (72.5) | 8.44 | 4.31-16.5 | < 0.001 | |
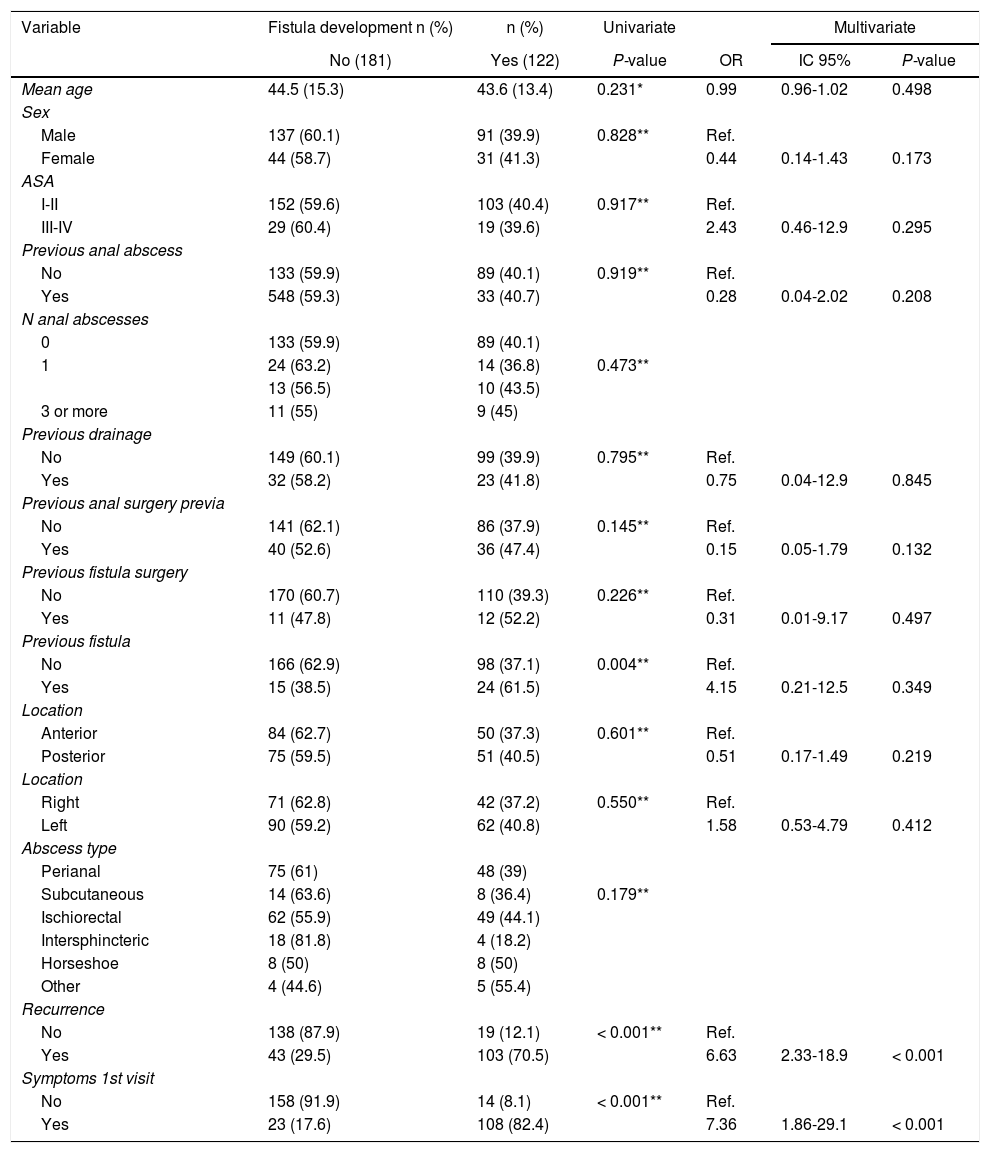
The appearance of recurrence during follow-up and the presence of symptoms in the follow-up visit were significantly related to the final diagnosis of fistula in the univariate analysis, both of which were independent risk factors in the multivariate analysis (Table 3).
Uni- and multivariate analysis according to the development of the fistula.
| Variable | Fistula development n (%) | n (%) | Univariate | Multivariate | ||
|---|---|---|---|---|---|---|
| No (181) | Yes (122) | P-value | OR | IC 95% | P-value | |
| Mean age | 44.5 (15.3) | 43.6 (13.4) | 0.231* | 0.99 | 0.96-1.02 | 0.498 |
| Sex | ||||||
| Male | 137 (60.1) | 91 (39.9) | 0.828** | Ref. | ||
| Female | 44 (58.7) | 31 (41.3) | 0.44 | 0.14-1.43 | 0.173 | |
| ASA | ||||||
| I-II | 152 (59.6) | 103 (40.4) | 0.917** | Ref. | ||
| III-IV | 29 (60.4) | 19 (39.6) | 2.43 | 0.46-12.9 | 0.295 | |
| Previous anal abscess | ||||||
| No | 133 (59.9) | 89 (40.1) | 0.919** | Ref. | ||
| Yes | 548 (59.3) | 33 (40.7) | 0.28 | 0.04-2.02 | 0.208 | |
| N anal abscesses | ||||||
| 0 | 133 (59.9) | 89 (40.1) | ||||
| 1 | 24 (63.2) | 14 (36.8) | 0.473** | |||
| 13 (56.5) | 10 (43.5) | |||||
| 3 or more | 11 (55) | 9 (45) | ||||
| Previous drainage | ||||||
| No | 149 (60.1) | 99 (39.9) | 0.795** | Ref. | ||
| Yes | 32 (58.2) | 23 (41.8) | 0.75 | 0.04-12.9 | 0.845 | |
| Previous anal surgery previa | ||||||
| No | 141 (62.1) | 86 (37.9) | 0.145** | Ref. | ||
| Yes | 40 (52.6) | 36 (47.4) | 0.15 | 0.05-1.79 | 0.132 | |
| Previous fistula surgery | ||||||
| No | 170 (60.7) | 110 (39.3) | 0.226** | Ref. | ||
| Yes | 11 (47.8) | 12 (52.2) | 0.31 | 0.01-9.17 | 0.497 | |
| Previous fistula | ||||||
| No | 166 (62.9) | 98 (37.1) | 0.004** | Ref. | ||
| Yes | 15 (38.5) | 24 (61.5) | 4.15 | 0.21-12.5 | 0.349 | |
| Location | ||||||
| Anterior | 84 (62.7) | 50 (37.3) | 0.601** | Ref. | ||
| Posterior | 75 (59.5) | 51 (40.5) | 0.51 | 0.17-1.49 | 0.219 | |
| Location | ||||||
| Right | 71 (62.8) | 42 (37.2) | 0.550** | Ref. | ||
| Left | 90 (59.2) | 62 (40.8) | 1.58 | 0.53-4.79 | 0.412 | |
| Abscess type | ||||||
| Perianal | 75 (61) | 48 (39) | ||||
| Subcutaneous | 14 (63.6) | 8 (36.4) | 0.179** | |||
| Ischiorectal | 62 (55.9) | 49 (44.1) | ||||
| Intersphincteric | 18 (81.8) | 4 (18.2) | ||||
| Horseshoe | 8 (50) | 8 (50) | ||||
| Other | 4 (44.6) | 5 (55.4) | ||||
| Recurrence | ||||||
| No | 138 (87.9) | 19 (12.1) | < 0.001** | Ref. | ||
| Yes | 43 (29.5) | 103 (70.5) | 6.63 | 2.33-18.9 | < 0.001 | |
| Symptoms 1st visit | ||||||
| No | 158 (91.9) | 14 (8.1) | < 0.001** | Ref. | ||
| Yes | 23 (17.6) | 108 (82.4) | 7.36 | 1.86-29.1 | < 0.001 | |
Among the numerous existing techniques for the treatment of anal abscesses. DD is the most frequent, with a strong recommendation grade and a level of evidence 113–15.
The goal of treatment is to cure the disease while preserving fecal continence16. The results are expressed according to the recurrence rate in the form of reappearance of the abscess or the development of chronic suppuration or fistula.
The recurrence rate is widely variable (1.6%-88%)17–26, although globally it is around 50%. The heterogeneous recurrence rates possibly reflect differences in diagnostic method, follow-up time and the presence of comorbidities such as IBD or a history of abscesses, fistulae or anal surgeries. IBD is closely related to the development of anal fistula17–19, but in many of the series it is not considered an exclusion criterion or its existence is simply not mentioned.
One of the main causes of recurrence is the presence of an undiagnosed fistula at the time of abscess drainage, which is estimated to be present in 30%-70% of cases13. There is controversy about the need or not to treat the fistula in the acute moment, if it is identified. Proponents of only performing drainage and debridement base their reasoning on the fact that it is a quick and simple process that can be performed by less experienced surgeons, and that less than half of the patients will present recurrence, while only one-third will develop a fistula6,18,20–22. In contrast, advocates of concomitant fistula treatment base their argument on the results of the meta-analysis by Malik et al23, which shows a significant decrease in recurrence without causing worsened continence, as long as the fistulae are simple. Despite this evidence, the concomitant treatment of the fistula does not enjoy sufficient consensus, especially for less experienced surgeons24.
In our study, we have found a recurrence rate of 48%, a figure in the middle range of published studies20,21,25–32. However, this is a very long-term datum (mean follow-up 119 months) in patients with previous episodes of abscess and anal fistula, but all of cryptoglandular origin. As has been reported by other authors11,20,21, the vast majority of recurrences occur in the first year of follow-up (82%) and are mainly in the form of chronic suppuration. Based on the study by Ho et al33, in which the mean time for complete healing of anorectal incisions was 7.2 weeks, we defined the time of recurrence as being after the 8th week of follow-up. In the series, only 4 patients (1.3%) had recurrence before that date (all abscesses), but they were included in the analysis.
In terms of the follow-up time, in our case we found that the flattening of the cumulative incidence curve for recurrence stabilizes after around 40 months. Previously, Yano et al22 described flattening after 20 months in their study of 205 patients with a recurrence rate of 36% and a mean follow-up of 20 months.
The incidence of fistula reported to date after the drainage of an anal abscess varies widely between 26% and 87%, depending on the series20,28–30,34. In a population-based retrospective study, Sahnan et al18 established the incidence of 15.5% in idiopathic primary cases, with a mean follow-up of 60 months, although they included techniques other than exclusive drainage. In our case, and with the diagnostic support of endoanal ultrasound, we found an incidence of fistula after urgent drainage of 44.1% (98 fistulae out of 222 ultrasounds performed), especially if they presented symptoms (69.6% vs 2.4%). If we also analyze patients with clinical criteria but without ultrasound, we could state that the total incidence of clinical and/or ultrasound fistula in our series is 40.3% (122/303 patients), a figure in the lower range of previously published reports and, in our opinion, a figure close to reality given the long follow-up period. It is possible that the adjuvant administration of antibiotics may decrease the rate of fistula development, although its use is still controversial since existing studies have published opposing results35,36. At the moment, the only existing systematic review on this issue is pending publication37.
We have identified the presence of symptoms in the first two months after drainage as an independent risk factor for recurrence (OR 8.44; 95%CI 4.31-16.5; P<.001) and for the development of a fistula (OR 7.36; 95%CI 1.86-29.1; P<.001), in addition to a statistical tendency to recur in the presence of a history of fistula (P=.09) and in the female sex (P=.07).
Our cohort includes patients with abscesses of cryptoglandular origin, both primary and recurrent, and with a history of fistula and anal surgery. This could make the results worse than expected. But the length of the follow-up makes it more realistic. This study has the limitations of being a retrospective and single-center study. In addition, ultrasound studies were not carried out randomly, so it is not free of possible biases.
ConclusionAfter urgent drainage and debridement of an anal abscess, half of patients relapse and 40% develop fistula. Recurrence occurs more frequently during the first year of follow-up, so longer follow-ups would not be necessary. The need for endoanal ultrasound to evaluate the presence of a fistula is highly questionable in the absence of signs or symptoms.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Chaveli Díaz C, Esquiroz Lizaur I, Eguaras Córdoba I, González Álvarez G, Calvo Benito A, Oteiza Martínez F, et al. Recidiva e incidencia de fístula tras el drenaje urgente de un absceso anal. Resultados a largo plazo. Cir Esp. 2022;100:25–32.