We report the frequency and age of metaplasia, dysplasia and carcinoma of the gallbladder, and seek to establish a sequence of progression of these, since several studies suggest that this is the carcinogenesis pathway.
Materials and methodsDescriptive retrospective cross-sectional study over a period of 4 years, with an analytical component of 1514 patients with cholelithiasis, in whom cholecystectomy was performed.
ResultsThe mean age of the sample was 46 years and 72% of patients were female. The prevalence (and mean age) of pyloric metaplasia, intestinal metaplasia, dysplasia and carcinoma was 22.6 (47), 2.1 (46), 0.2 (54) and 0.6% (63 years), respectively. There was a significant association between intestinal and pyloric metaplasia (P<.001, chi2) and between dysplasia and carcinoma (P<.005, Yates), but not between metaplasia and dysplasia.
ConclusionImproved studies should be conducted for the correct interpretation of the pathogenesis of gallbladder cancer.
Se reporta la prevalencia y la edad de metaplasia, displasia y carcinoma de vesícula biliar y se trata de establecer una secuencia de progresión de las mismas, ya que diversos estudios la sugieren como vía de la carcinogénesis.
Material y métodosEstudio descriptivo, retrospectivo de corte transverso con componente analítico, de 1.514 pacientes con colelitiasis en quienes se realizaron colecistectomías, en un periodo de 4 años.
ResultadosEl 72% de los pacientes fueron mujeres, con un promedio general de edad de 46 años. La prevalencia (y promedio de edad) de metaplasia pilórica, metaplasia intestinal, displasia y carcinoma fue de 22,6 (47), 2,1 (46), 0,2 (54) y 0,6% (63 años), respectivamente. Hubo una asociación significativa entre metaplasia pilórica e intestinal (p<0,001, chi2), y entre displasia y carcinoma (p<0,005, Yates), no así entre metaplasia y displasia.
ConclusiónSe deben realizar mejores estudios para la correcta interpretación de la patogénesis del cáncer de vesícula biliar.
Cancer of the gallbladder (GBC) is the most frequent cancer of the biliary tract worldwide and the fifth most frequent cancer of the gastrointestinal tract.1–4 In all, 0.5%–2% of patients present GBC in specimens after elective cholecystectomy for cholelithiasis.1,3 GBC remains a malignancy with a poor prognosis, with five-year survival rate of less than 5%.2
It generally presents in patients of advanced age: more than 90% of patients are aged over 50 years and incidence increases with age, reaching its peak between 70 and 75 years. It is more common in females, three times more prevalent than in males.1,5 It also has prominent geographic differences; there is a high incidence in Chile, Bolivia, North-West Europe and Poland, amongst other countries.
Symptomatic cholelithiasis and chronic inflammation are the most frequent symptoms associated with GBC, mentioned in traditional literature.5,6 Due to advances in understanding this disease, abnormal biliopancreatic union, dysplasia and adenoma (both epithelial lesions) are currently recognised as three premalignant states prior to progression to GBC.7
Metaplasia of the gallbladder epithelium is produced by chronic inflammation, such as that caused by cholelithiasis.8 There are two principle types of metaplasia observed in the bile duct: pyloric (gastric) and intestinal.9 Pyloric metaplasia is the most common and is found in 50% of specimens from cholecystectomy due to cholelithiasis or chronic calculous cholecystitis.10 The incidence of intestinal metaplasia increases with age and the duration of cholelithiasis.9
Various authors suggest that metaplasia is the connection as a carcinogenic route between cholelithiasis and dysplasia of the gallbladder, and subsequently to cancer.10–14 Moreover, some studies have indicated that the progression time from dysplasia to carcinoma in situ and to invasive gallbladder cancer is from 10 to 15 years.15
This study determines the frequency of metaplasia, dysplasia and GBC in patients who have undergone cholecystectomy due to symptomatic cholelithiasis and the age at which these lesions presented, in an attempt to establish the existence of a sequence of progression between them.
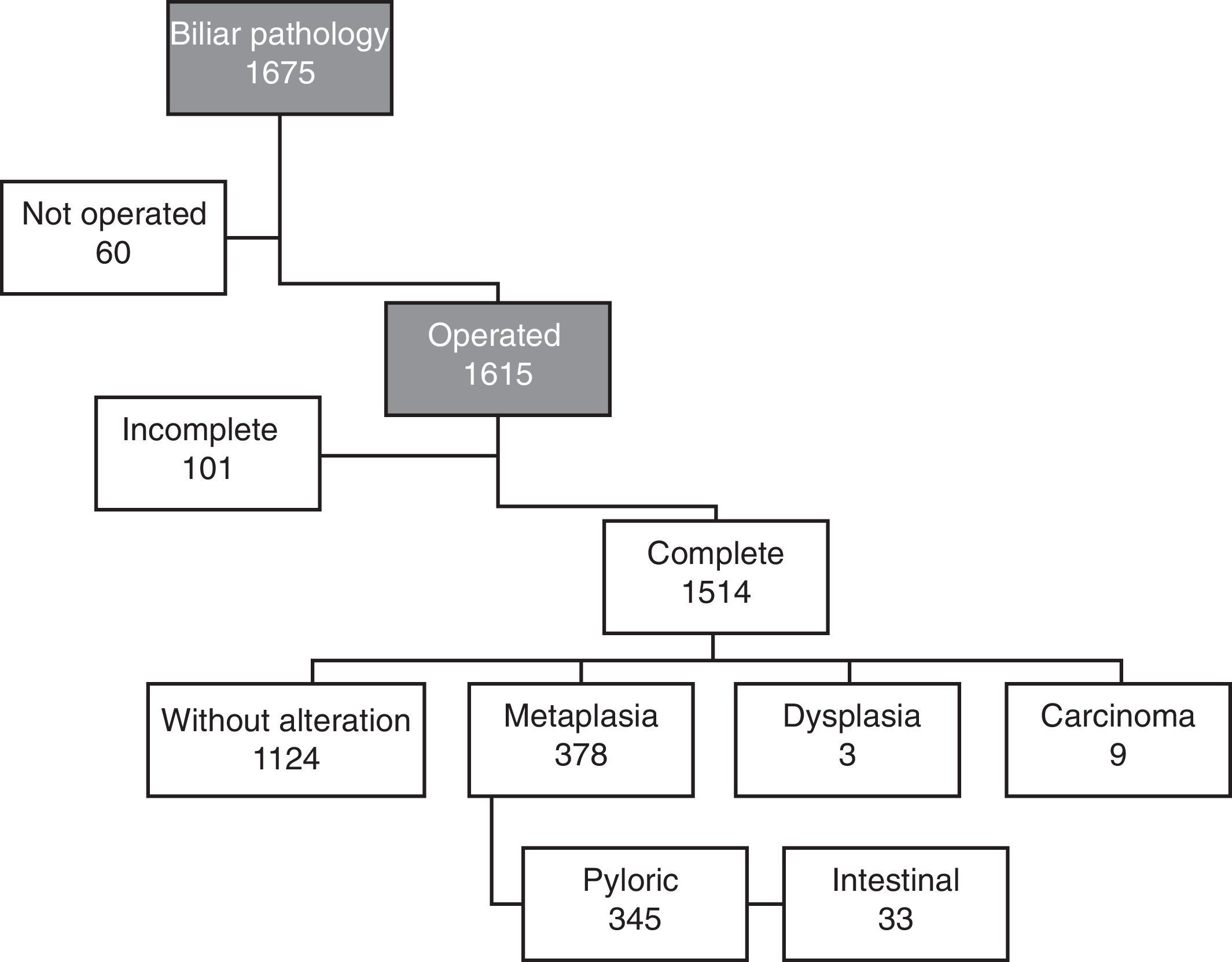
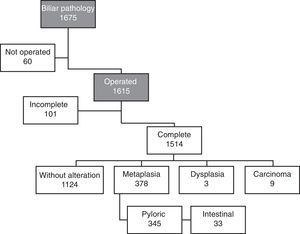
Materials and MethodsA descriptive, retrospective and transverse study with an analytical component was conducted of 1514 consecutive cases of patients from the II Department of Surgical Clinic of the Hospital de Clínicas of the Medical Science Faculty of the National University of Asunción (FCM-UNA), Paraguay. All patients with biliary disease admitted to the unit from 1 January 2005 to 31 December 2008 were included in the study. Included as biliary disease were symptomatic cholelithiasis, chronic cholecystitis, acute cholecystitis, acute biliary pancreatitis, choledocolithiasis, Mirizzi syndrome, obstructive jaundice, acute cholangitis, GBC, bile duct cancer, biliodigestive fistula, bile duct stenosis and gallbladder mass. A total of 1675 case records were collected. Patients who had not been operated were rejected and only those who had undergone cholecystectomy were included (exclusively or with other surgical procedures), totalling 1615 records. The pathological anatomy reports for the 1615 case records were sought in the department's archives and in the Pathological Anatomy Institute of the FCM-UNA. Of these, 101 records could not be recovered; the final number of case records found was 1514 (Fig. 1).
The absolute and relative frequency of the qualitative variables was described. The description of the quantitative variables was made using mean and standard deviation, and the data were analysed using nonparametric chi tests2 Yates correction and Fisher's exact test, using the Epi Info™ computer programme version 3.5.1.
The confidentiality of individual data was upheld and it was ensured that the exposure of results was collective and, if individual, that privacy was maintained.
ResultsOf the total 1514 patients assessed, 1090 were women (71.9%), with a male to female ratio of 1:2.5 and an average general age of 45.6±16 years.
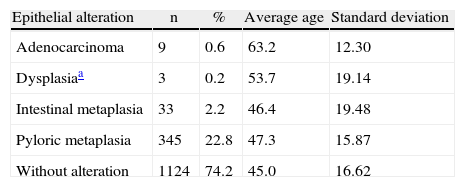
The prevalence of pyloric metaplasia, intestinal metaplasia, dysplasia and carcinoma was 345 (22.8%), 33 (2.2%), 3 (0.2%) and 9 (0.6%, all women) patients, respectively. In addition, the average age was 47.3, 46.4, 53.7 and 63.2 years, respectively (Table 1). The average age of patients who did not present the aforementioned epithelial alterations was 45.0±16 years. The difference in age between the patients with dysplasia and carcinoma was 10 years.
Metaplasia, Dysplasia and Gallbladder Cancer Findings.
| Epithelial alteration | n | % | Average age | Standard deviation |
| Adenocarcinoma | 9 | 0.6 | 63.2 | 12.30 |
| Dysplasiaa | 3 | 0.2 | 53.7 | 19.14 |
| Intestinal metaplasia | 33 | 2.2 | 46.4 | 19.48 |
| Pyloric metaplasia | 345 | 22.8 | 47.3 | 15.87 |
| Without alteration | 1124 | 74.2 | 45.0 | 16.62 |
A significant difference was found on analysis of the association between pyloric and intestinal metaplasia (P<.001, chi2) (Table 2).
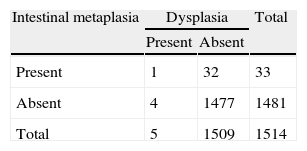
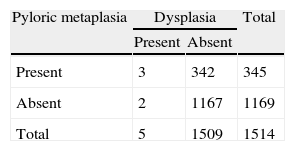
No significant association was found between intestinal metaplasia and dysplasia (P=.1, 2 tailed, Fisher) (Table 3) or between pyloric metaplasia and dysplasia (P=.14, Yates) (Table 4).
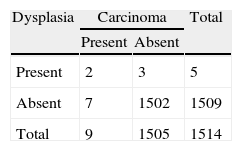
A significant association was found between dysplasia and carcinoma (there were two cases of adenocarcinoma with sources of dysplasia, which were added to the dysplasia group to conduct the analysis) (P<.005, Yates) (Table 5).
DiscussionThe number of patients (101) who were not included in the study because no pathological report had been presented is of concern, despite searching by name and surname in both units. A solution to this circumstance must be found, to ensure patient safety and indeed to avoid possible situations of medical-legal conflict.
The proportion of female patients found in this study (71.9%) is similar to that cited by Lai and Lau in Hong Kong.1
The association between cholelithiasis and GBC is well known; it is encountered in 80% of cases of the latter.3,6 In this study, the presence of cholelithiasis (corroborated by ultrasound) was required for the patients to be included.
A low prevalence of metaplasia, dysplasia and carcinoma was found. According to Albores-Saavedra and Henson, cited by Meirelles-Costa et al., the incidence of histological alterations found in chronic cholecystitis is a reflection of the amount of segments analysed and the technique used; an incidence of 13.5 and 3.5% respectively of dysplasia and carcinoma in situ was reported.3
The prevalence of intestinal metaplasia found (22.8%) is similar to that cited by Yamagiwa and Tomiyama and Yamagiwa in Japan.13,16 It was less than that found in studies in Brazil (73.8%)17 and greater than that in studies in India (15.5%),18 the United States (9.8%)10 and Canada (10.8).19 The prevalence of pyloric metaplasia was much lower (2.2%).
The 0.2% frequency of dysplasia encountered is similar to that of Dowling and Kelly's study (0.4%),19 although there is research reporting a frequency of 13.5% (Mexico, Albores-Saavedra et al.).11
The average age of the patients with dysplasia (53.7 years) is similar to that found in the United States (52.6 years),10 whereas in Chile (with a high prevalence of GBC) the average is 46.3 years.15
The prevalence of GBC was also low. Furthermore, the difference between the average age of patients with dysplasia and carcinoma was ten years, a figure similar to that found in Chile by Roa et al.15 A significant association was found between dysplasia and carcinoma (Table 5).
If metaplasia is a stage prior to dysplasia, the patients with metaplasia would present a lower average age than those with dysplasia. This study demonstrates a progressive gradient from patients with normal mucosa, to metaplasia, dysplasia and eventually carcinoma (45, 46–47, 53 and 63 years of age, respectively). But this finding cannot be confirmed with certainty, as no significant association was demonstrated between metaplasia and dysplasia (Tables 2 and 3) and because this is a study that was designed in principle to calculate the frequency of metaplasia, dysplasia and carcinoma.
Despite this, the findings of other authors indicate that the progression from pyloric metaplasia to dysplasia takes approximately three years, and from dysplasia to carcinoma, fifteen years15,20; these are findings similar to those of this study (6–7 and 10 years, respectively).
Better analyses are required to gain further understanding of the pathogenesis of GBC. The knowledge that will be acquired will be crucial for proposing changes in surgical treatment, such as elective cholecystectomy for asymptomatic cholelithiasis, for example.
Conflict of InterestsThe authors declare that there is no conflict of interests.
Please cite this article as: Segovia Lohse HA, Cuenca Torres OM. Prevalencia y secuencia metaplasia-displasia-carcinoma de vesícula biliar. Estudio retrospectivo unicéntrico. Cir Esp. 2013;91:672–675.