The aim of this study was to evaluate the prevalence, clinical characteristics and management of chronic venous disease (CVD) in patients seen at primary care clinics.
Patients and methodsThis cross-sectional study was carried-out in Spain by 999 primary care physicians. They recruited 20 consecutive patients who were attending their clinics for any reason except for a medical emergency. The following information was collected: demographic data, CVD risk factors, physical examination, clinical characteristics of the CVD and how it was managed.
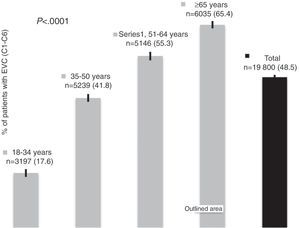
Results19800 patients were included, predominantly women (63%), with a mean age of 53.7±20 years. The prevalence of CVD (CEAP categories C1–C6) was 48.5% (95% CI, 47.8–49.2), significantly higher in women (58.5%; 95% CI, 57.6–59.4) than in men (32.1%; 95% CI, 31.0–33.1). The greater the age the higher the prevalence and the more advanced the CVD. Ninety-nine percent of the patients required some form of treatment, with a greater proportion among women (72% vs 39%, P<.0001). Sclerotherapy, endothermal ablation or surgery was required by 4% of the patients. Referral to the specialist was considered for 7% of the patients.
ConclusionChronic venous disease is highly prevalent among patients seen at primary care clinics in Spain, especially in women and elderly patients. Referral to a specialist and/or the use of the more invasive treatment procedures is uncommon.
El objetivo de este estudio fue evaluar la prevalencia de la enfermedad venosa crónica (EVC), sus características clínicas y la conducta terapéutica ante estos pacientes en Atención Primaria.
Pacientes y métodosEstudio transversal realizado en España por 999 médicos de Atención Primaria que debían reclutar a 20 pacientes consecutivos que acudieran a su consulta, de forma programada, por cualquier motivo. Se recogieron datos demográficos, factores de riesgo y datos clínicos de la ECV, exploración física que permitiera su categorización de acuerdo con la clasificación Clínica-Etiología-Anatomía-Patofisiología (CEAP), y la atención terapéutica recomendada.
ResultadosSe incluyó a 19.800 pacientes con una edad media±desviación estándar de (53,7±20) años y con predominio de mujeres (63%). La prevalencia de EVC (categorías CEAP C1 a C6) fue del 48,5% (IC del 95%, 47,8 a 49,2), significativamente superior en mujeres (58,5%; IC del 95%, 57,6 a 59,4) respecto de los hombres (32,1%; IC del 95%, 31,0 a 33,1). La ECV era más prevalente y avanzada según se incrementaba la edad de los pacientes. En el 59% de los pacientes se consideró necesario instaurar algún tratamiento, siendo más frecuente en mujeres que en hombres (72% vs 39%, p<0,0001). La recomendación de escleroterapia, ablación endotérmica o cirugía constituyó el 4% de todas las recomendaciones, y en un 7% se consideró necesaria la derivación al especialista.
ConclusionesLa EVC es altamente prevalente en pacientes atendidos en Atención Primaria en España, especialmente en mujeres y en edades más avanzadas. La derivación al especialista o la utilización de los tratamientos más invasivos es infrecuente.
The clinical presentation of chronic venous disease (CVD) varies from cosmetic problems to the presence of severe symptoms, including the presentation of ulcers. Frequently, the presence of varices causes discomfort, pain, absenteeism in the workplace, disability and deteriorated quality of life.1 In addition to the impact on individuals, the healthcare system is also affected. In the United States, for instance, the direct medical cost of CVD is estimated at 150 million to 1 billion dollars per year, and 2% of the national healthcare budget in the United Kingdom is spent on treating ulcers of the lower extremities.2
In 1999, an international group of experts recommended developing CVD research studies about its incidence and prevalence using standardized measurements for venous disease.3 Many of the studies focus on patients who have or report venous problems,4–7 while others center on subpopulations at risk.8–10 Furthermore, there are few studies that have used the CEAP (Clinical-Etiology-Anatomy and Pathophysiology) classification.11–16
Although the data are also limited, the treatment of patients with CVD seems to vary from one country to the next. A contributing factor may have been the fact that clinical practice guidelines or consensus did not appear until relatively recently, fundamentally since the year 2000.2,16–20
For all these reasons, the International Union of Phlebology designed this multicenter, international study whose objectives were to evaluate the prevalence of CVD from its initial stages along with its clinical characteristics, and to obtain data about the treatment of these patients in Primary Care. This article presents the results obtained in Spain.
Patients and MethodsThis cross-sectional multicenter study was performed in Spain between May 2009 and June 2010 by 999 Primary Care physicians who had been selected randomly throughout Spain. The study was approved by the Clinical Research Ethics Committee at the Hospital Clínic in Barcelona. Written informed consent was obtained from all the participants.
The participating physicians were asked to recruit 20 consecutive patients in a maximum period of 2 days. The inclusion criteria were: patients who came to their consultation for whatever reason who were over the age of 18. Emergency consultations were excluded. There were no sex or age limits. The study was done in accordance with standard clinical practice and without interfering with the diagnostic or therapeutic practices of the participating physicians.
On the single office visit of the study, the participating doctors collected information about the demographic data of the patients (age and sex), CVD risk factors such as family history, personal history of venous thrombosis or pulmonary embolism, postural habits, physical activity, smoking and history of hormonal treatment; clinical data about clinical CVD symptoms and their treatment to date; physical examination data consisting of the exploration of CVD signs following the CEAP classification, which should enable the doctor to diagnose CVD, and finally, data about the therapeutic recommendations provided by the participating physician for the patient, including possible referral to a specialist.
The statistical analysis was essentially descriptive, using mean±standard deviation for the quantitative variables and the distribution of absolute and relative frequencies for the categorical variables. In all the cases, the number of cases valid for analysis is provided. Exploratory bivariate analyses were also performed using for the comparisons the Student's t test or one-way ANOVA for the quantitative variables and the chi-squared test for categorical variables. A P≤.05 was considered statistically significant. Given the exploratory character of these analyses, no multiplicity corrections were done.
ResultsDemographic and Clinical Characteristics of the Participating SubjectsIn total, 19800 patients were recruited with a mean age±standard deviation of 53.7±20; 31% of the patients were 65 years old or older, and there was a predominance of women (63%). 45% of the recruited patients were actively working. Mean body mass index in men was 26.6±4 in men and 26±5 in women.
With regards to the CVD risk factors, 40% of the patients had a family history of CVD, 5% had a personal history of venous thrombosis or pulmonary embolism, and 39% did regular exercise. The number of hours that they spent standing and sitting were 6.8±3 and 6.1±3, respectively, and 60% were smokers or ex-smokers.
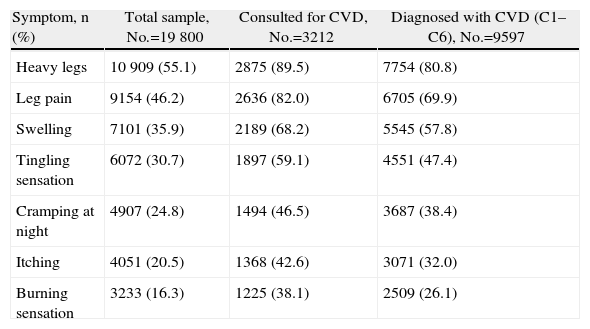
Symptoms and Prevalence of Chronic Venous Disease67.2% (n=13300) (95% confidence interval [CI], 66.5–67.8) presented some sign of CVD, with a mean per patient of 2.3±2 symptoms. The most frequent symptoms in the overall sample were the sensation of heavy legs (55%), leg pain (46%) and swelling (36%) (Table 1). In those patients with symptoms, these were more frequently exacerbated at the end of the day (63%), in the summer (51%), at night (44%) or after standing for lengthy periods (40%).
Symptoms of CVD.
| Symptom, n (%) | Total sample, No.=19800 | Consulted for CVD, No.=3212 | Diagnosed with CVD (C1–C6), No.=9597 |
| Heavy legs | 10909 (55.1) | 2875 (89.5) | 7754 (80.8) |
| Leg pain | 9154 (46.2) | 2636 (82.0) | 6705 (69.9) |
| Swelling | 7101 (35.9) | 2189 (68.2) | 5545 (57.8) |
| Tingling sensation | 6072 (30.7) | 1897 (59.1) | 4551 (47.4) |
| Cramping at night | 4907 (24.8) | 1494 (46.5) | 3687 (38.4) |
| Itching | 4051 (20.5) | 1368 (42.6) | 3071 (32.0) |
| Burning sensation | 3233 (16.3) | 1225 (38.1) | 2509 (26.1) |
CVD: chronic venous disease.
21% of the patients (n=3929) (95% CI, 20–22) had consulted with their physicians due to their venous problems in the lower extremities, and there were significant differences between men (12%; 95% CI, 11–13) and women (26%; 95% CI, 25–27). Out of these 3929 patients, the Primary Care physicians confirmed the diagnosis of CVD in 3212 (82%).
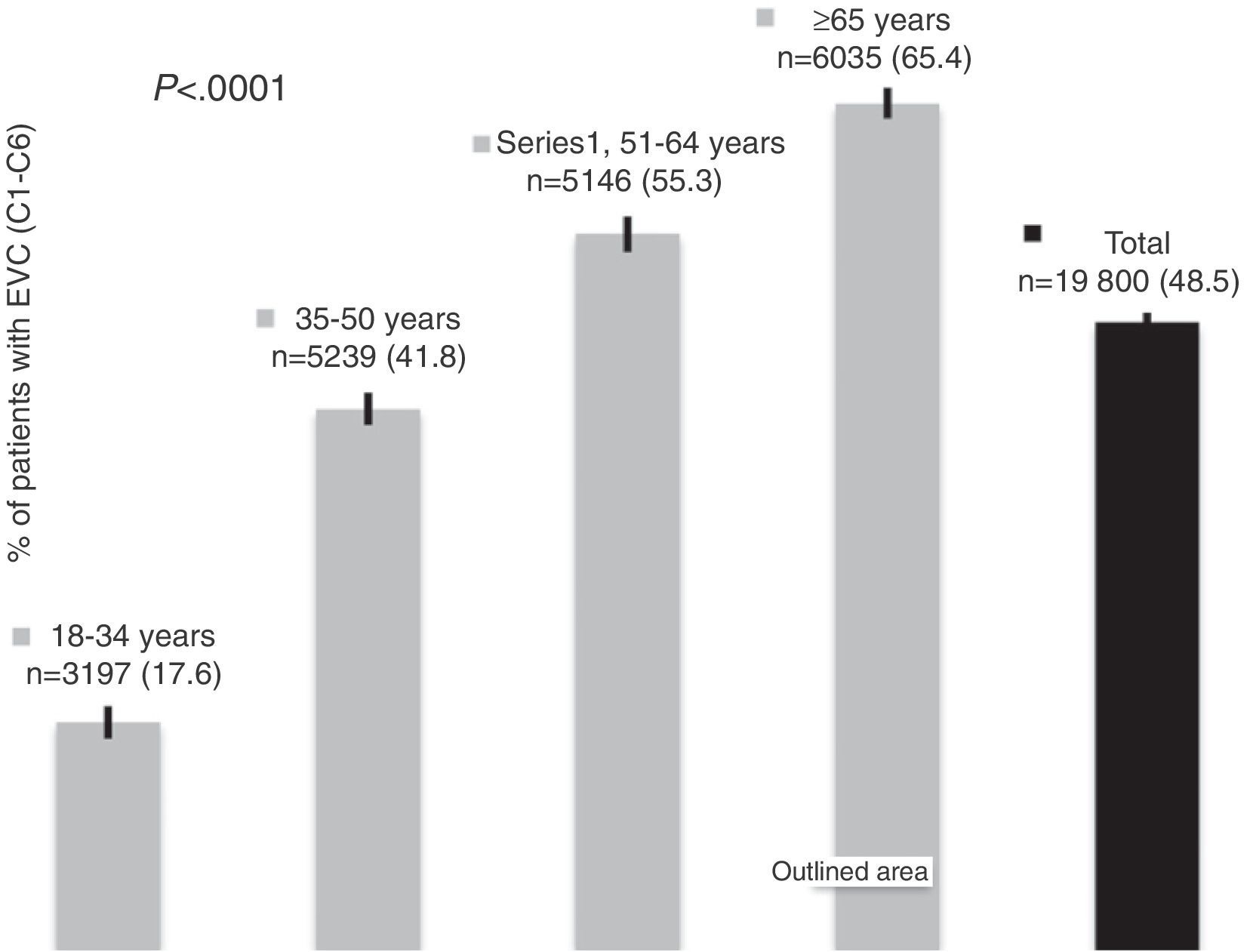
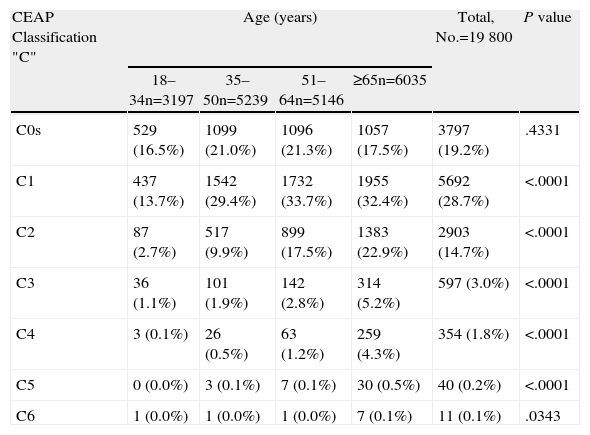
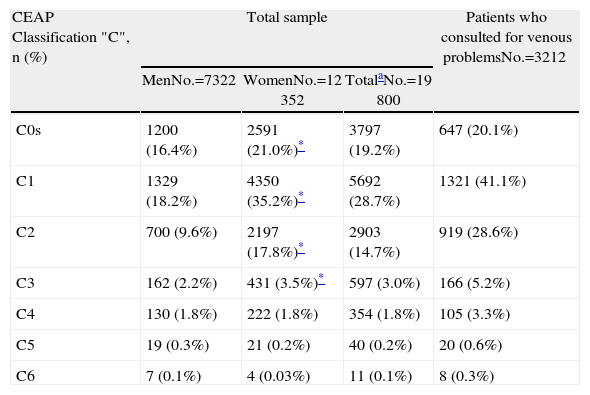
From the 19800 patients included, 9597 were categorized (according to physical examination) into categories C1 to C6 of the CEAP. The prevalence of CVD was 48.5% (95%, 47.8–49.2) and was significantly higher in women (58.5%; 95% CI, 57.6–59.4) than in men (32.1%; 95% CI, 31.0–33.1). When category C0s was included (meaning the presence of symptoms related with CVD, but no signs), the prevalence increased to 67.7% (95% CI, 67–68.3). The prevalence of CVD increased notably with age (Fig. 1) and, in the same manner, the disease presented in more advanced stages at older ages (Table 2). The distribution of the patients in accordance with the categories of the CEAP classification for the total sample and for those who consulted due to venous problems is presented in Table 3. The proportion of patients with more advanced disease (categories C4–C6) was small and practically identical in men and in women (2.1% and 2%, respectively); however, in the women there was a greater prevalence of the disease observed in categories C1–C3. The patients who consulted for venous problems had somewhat more advanced disease (Table 3).
CVD Stage (CEAP Classification “C”) According to Age.
| CEAP Classification "C" | Age (years) | Total, No.=19800 | P value | |||
| 18–34n=3197 | 35–50n=5239 | 51–64n=5146 | ≥65n=6035 | |||
| C0s | 529 (16.5%) | 1099 (21.0%) | 1096 (21.3%) | 1057 (17.5%) | 3797 (19.2%) | .4331 |
| C1 | 437 (13.7%) | 1542 (29.4%) | 1732 (33.7%) | 1955 (32.4%) | 5692 (28.7%) | <.0001 |
| C2 | 87 (2.7%) | 517 (9.9%) | 899 (17.5%) | 1383 (22.9%) | 2903 (14.7%) | <.0001 |
| C3 | 36 (1.1%) | 101 (1.9%) | 142 (2.8%) | 314 (5.2%) | 597 (3.0%) | <.0001 |
| C4 | 3 (0.1%) | 26 (0.5%) | 63 (1.2%) | 259 (4.3%) | 354 (1.8%) | <.0001 |
| C5 | 0 (0.0%) | 3 (0.1%) | 7 (0.1%) | 30 (0.5%) | 40 (0.2%) | <.0001 |
| C6 | 1 (0.0%) | 1 (0.0%) | 1 (0.0%) | 7 (0.1%) | 11 (0.1%) | .0343 |
Distribution of the Patients in Accordance With the CEAP Classification Categories for Chronic Venous Disease.
| CEAP Classification "C", n (%) | Total sample | Patients who consulted for venous problemsNo.=3212 | ||
| MenNo.=7322 | WomenNo.=12352 | TotalaNo.=19800 | ||
| C0s | 1200 (16.4%) | 2591 (21.0%)* | 3797 (19.2%) | 647 (20.1%) |
| C1 | 1329 (18.2%) | 4350 (35.2%)* | 5692 (28.7%) | 1321 (41.1%) |
| C2 | 700 (9.6%) | 2197 (17.8%)* | 2903 (14.7%) | 919 (28.6%) |
| C3 | 162 (2.2%) | 431 (3.5%)* | 597 (3.0%) | 166 (5.2%) |
| C4 | 130 (1.8%) | 222 (1.8%) | 354 (1.8%) | 105 (3.3%) |
| C5 | 19 (0.3%) | 21 (0.2%) | 40 (0.2%) | 20 (0.6%) |
| C6 | 7 (0.1%) | 4 (0.03%) | 11 (0.1%) | 8 (0.3%) |
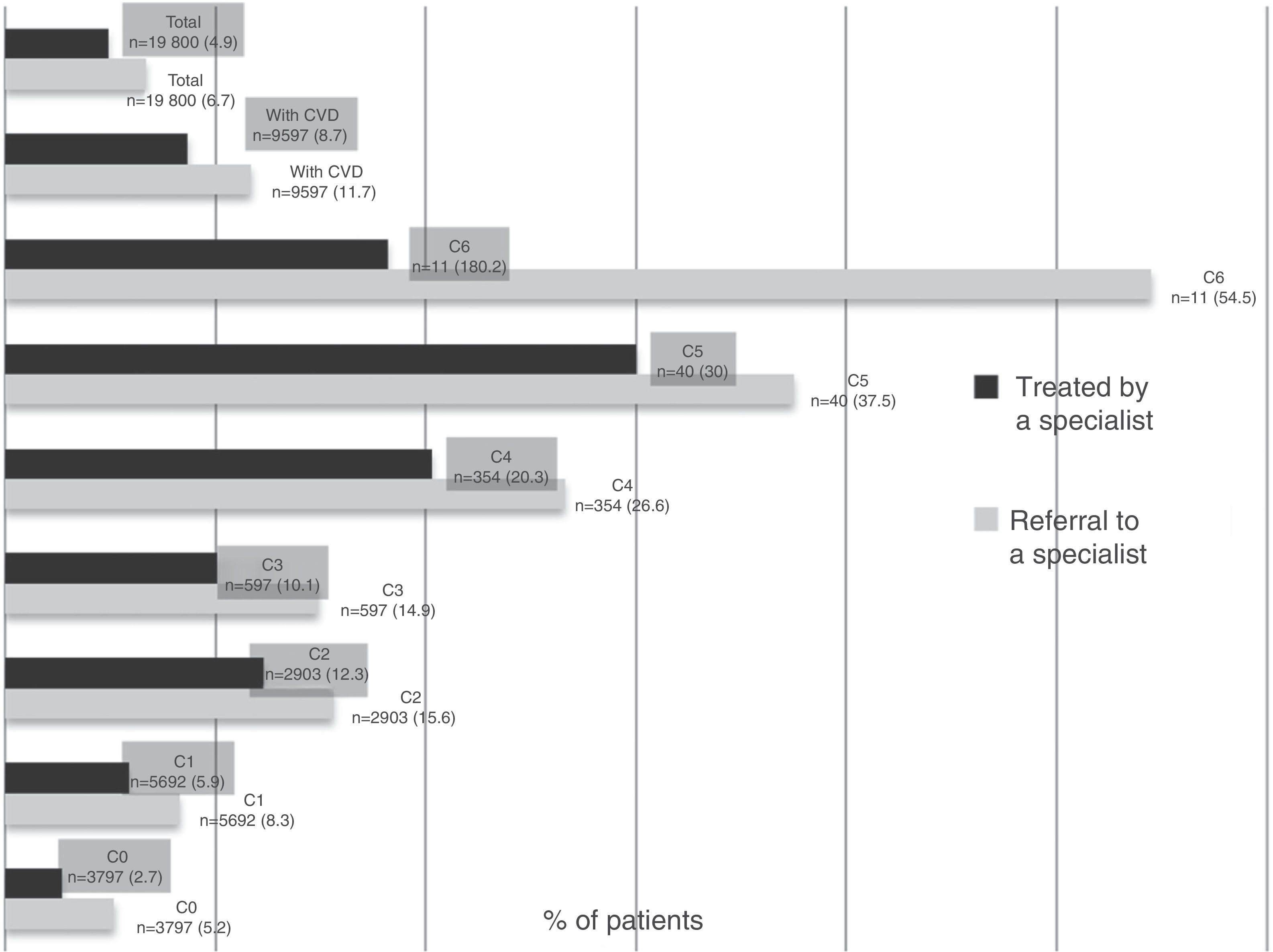
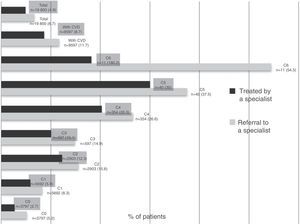
It was considered necessary to refer almost 7% of all the patients to specialists, and 5% were already being treated by specialists. Compared with men, a greater proportion of women required referral to a specialist (7.5% vs 5.5%, P<.0001) or were being treated by a specialist (5.8% vs 3.3%, P<.0001). Both the proportion of patients who required referral to a specialist as well as those who were already being treated by a specialist increased with more advanced disease stages (Fig. 2).
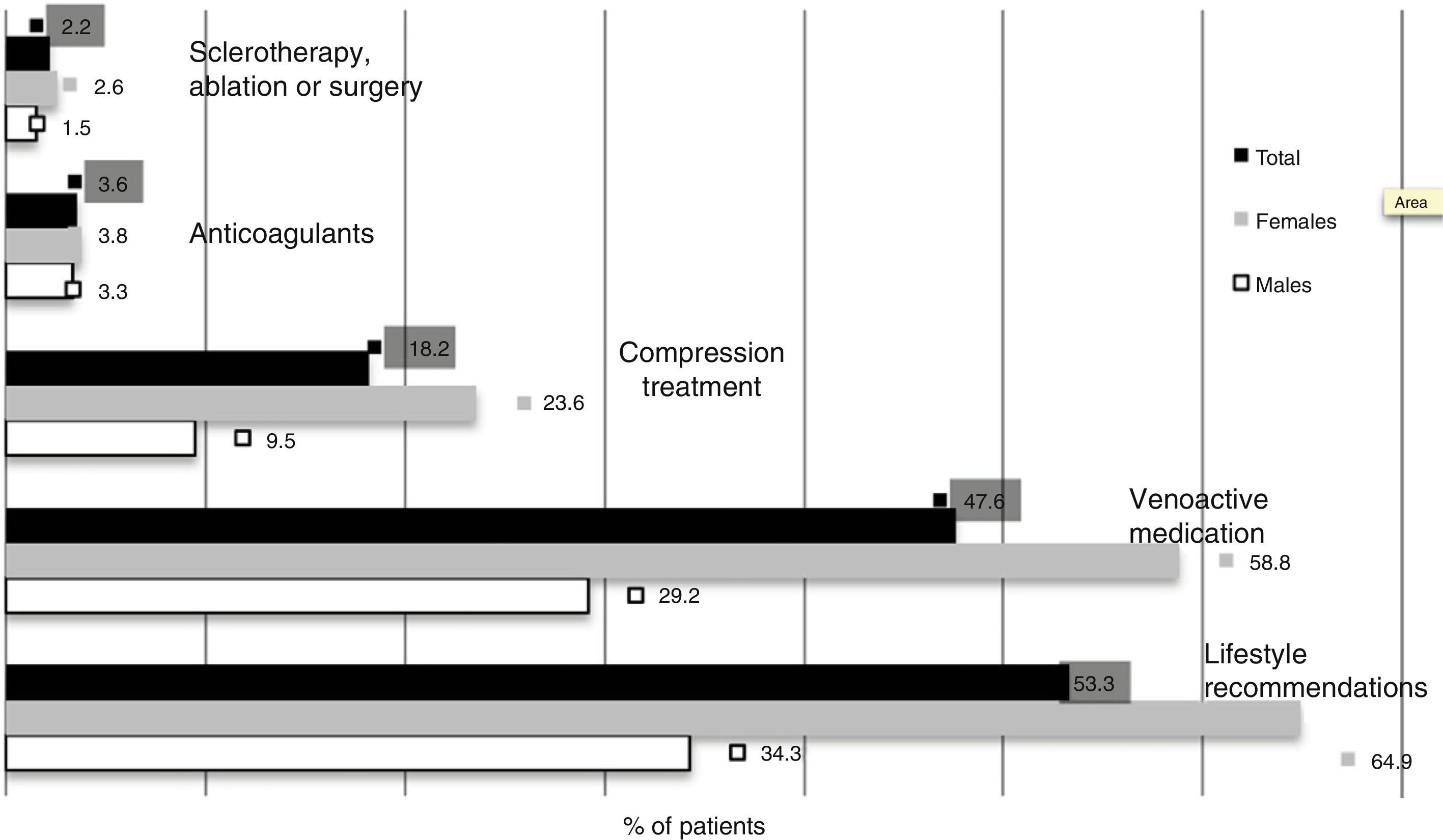
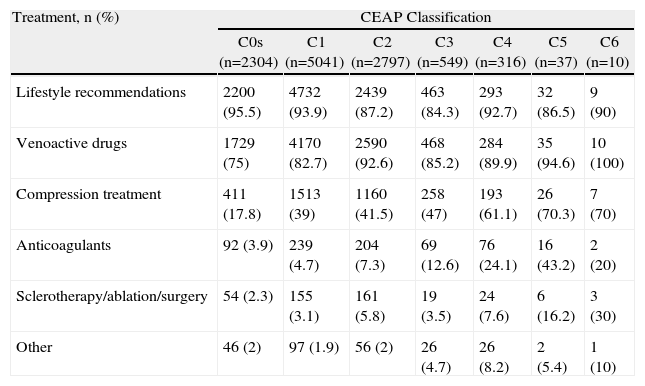
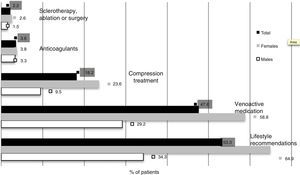
In 11449 (59%) of the patients included, it was considered necessary to establish a treatment. The recommended treatments in these patients were lifestyle recommendations (92%), venoactive medication (82%), compression treatment (32%), and anticoagulant therapy due to venous complications (6%); venous repair (sclerotherapy, endovenous ablation or surgery) was considered indicated in only 4%. Once again, the need for treatment was significantly greater in women than in men (72% vs 39%, P<.0001). The treatments recommended according to the clinical stage of the disease are presented in Table 4.
Treatments Recommended by the Primary Care Physician for Patients With CVD in Accordance With the Clinical Stage (CEAP).
| Treatment, n (%) | CEAP Classification | ||||||
| C0s (n=2304) | C1 (n=5041) | C2 (n=2797) | C3 (n=549) | C4 (n=316) | C5 (n=37) | C6 (n=10) | |
| Lifestyle recommendations | 2200 (95.5) | 4732 (93.9) | 2439 (87.2) | 463 (84.3) | 293 (92.7) | 32 (86.5) | 9 (90) |
| Venoactive drugs | 1729 (75) | 4170 (82.7) | 2590 (92.6) | 468 (85.2) | 284 (89.9) | 35 (94.6) | 10 (100) |
| Compression treatment | 411 (17.8) | 1513 (39) | 1160 (41.5) | 258 (47) | 193 (61.1) | 26 (70.3) | 7 (70) |
| Anticoagulants | 92 (3.9) | 239 (4.7) | 204 (7.3) | 69 (12.6) | 76 (24.1) | 16 (43.2) | 2 (20) |
| Sclerotherapy/ablation/surgery | 54 (2.3) | 155 (3.1) | 161 (5.8) | 19 (3.5) | 24 (7.6) | 6 (16.2) | 3 (30) |
| Other | 46 (2) | 97 (1.9) | 56 (2) | 26 (4.7) | 26 (8.2) | 2 (5.4) | 1 (10) |
The results are practically identical to those from the DETECT studies published in 2000 and 2006, which detected CVD prevalence (defined by CEAP classes C0 to a C6) of 68.6 and 69.7%, respectively.14,21 Nevertheless, it is important to emphasize that, compared with those 2 studies, the patients of our study presented less advanced disease; thus, in the DETECT 2000 and 2006 studies, 15% and 19% of the patients with CVD, respectively, were in stages C3–C6, while in our study only 7.5% were in those stages of the disease. The distribution by sexes of the 3 studies is almost identical and the mean age is somewhat higher in our study (53.7 vs 52.3 and 51.4 years in our study and in the DETECT 2000 and DETECT 2006 studies, respectively). Nonetheless, the mentioned age differences along with the fact that the 3 studies had very extensive patient samples and used the same patient selection method indicate, in our opinion, that bias selection alone would not be able to explain such clear differences. Unfortunately, our study did not enable us to assess whether this change in severity of the disease is due to greater awareness amongst patients or Primary Care physicians about the importance of CVD and its rapid identification and intervention.
When compared with other countries, our CVD prevalence results are similar to 2 studies done in Primary Care in Poland12 and Bulgaria16 that found (with the same diagnostic criteria) CVD prevalences of 49 and 44%, respectively. In contrast, the prevalence was less (38.3%) in a Primary Care study carried out in Saudi Arabia13 and quite higher (71%) in a more recent study from the U.S.A. This latter study, however, was a CVD screening program in which 42% indicated having consulted with their physician due to varicose veins,15 which would explain the different prevalence rates.
The notable differences between the sexes in the prevalence of CVD in our study are in consonance with the previously mentioned studies performed in Primary Care.12,13,16 In reality, there are only a few studies that do not support this difference between the sexes, the most notable exception being the Edinburgh Vein Study, which detected a prevalence of truncal varicose veins of 40% in men versus 32% in women.22 This is also consistent with the findings of previous studies: the marked increase of prevalence with age and, as expected, the presentation of more advanced disease as patients age.14 It has already been described in other studies that the greater the time that passes from the onset of the disease until the patient consults with a specialist, the more advanced the disease is.5
The proportion of patients that the Primary Care physicians decided to refer to specialists (7%) is very similar to the percentage of the DETECT 2006 study (9%), and the distribution of CEAP classes of that study is almost identical.21 An important proportion of patients who presented more advanced disease were not treated by specialists, nor was their referral expected (more than 30% in stages C5–C6 and more than 50% in stage C4). Although in our setting there are clinical guidelines for the management of CVD in Primary Care,23 specialist referral criteria have been published and there is a consensus among different scientific societies,24 this information has not been sufficiently communicated among Primary Care doctors.
As for the treatments recommended by Primary Care physicians (Fig. 3), they advocated conservative measures, and the recommendation of more aggressive treatments was uncommon; sclerotherapy, endovenous ablation or surgery were suggested in 4% of the patients who were recommended therapeutic intervention. In Spain, there are no specialists in vascular pathologies in the Primary Care setting, and the indication of these therapies is not the responsibility of general practitioners, so they are not usually recommended. In other European countries, the recommendation of these more invasive treatments seems to be more frequent. In the study done in Bulgaria, treatment with sclerotherapy was recommended by the Primary Care physician in 3% of cases and surgery in 6%.16 Meanwhile, in a study performed in Italy, closer to our setting, the treatments recommended by specialists for CVD (C0–C6) were medication (80%), compression (56%), sclerotherapy (19%) and surgery (18%); the recommendation for surgical treatment reached 40% of the patients for classes C5–C6.25 The fact that in our study a rather notable proportion of women received treatment for CVD, also reported in other countries in our setting, is not only explained by the fact that they had more advanced disease. Although merely speculative, these differences could reflect the higher demand for treatment by women due to a greater awareness about the problem of CVD, either for health reasons or, in some cases, for esthetic reasons.
Our study has several limitations. As stated previously, the use of a convenience sampling may have represented a selection bias whose possible consequences have already been commented on. Furthermore, no sampling was done of the participating centers; therefore, despite the high level of participation of Primary Care physicians and their patients, our study cannot be considered representative of the entire Primary Care system in Spain. Last of all, no patients from our study nor a sample of these were seen by a specialist to confirm the diagnoses, which could bias the results one way or another. Nonetheless, it must be indicated that, in a study where this double evaluation was done, the agreement between the Primary Care physicians and specialists was very high.16
In conclusion, CVD is highly prevalent among patients who use Primary Care services in Spain, and the data is consistent with previous studies. There are important differences both between the sexes and compared with studies performed in other European countries. The development of updated specific clinical practice guidelines favoring diagnosis in early stages of the disease would help Primary Care physicians to properly manage these patients and correctly refer them to specialists.
FundingNo grants have been received to fund this study.
Conflict of InterestsDr. José-Román Escudero has received remuneration for the coordination of this study.
The authors would like to thank Laboratorios Servier S.L. for their support of the study done in Spain, Françoise Pitsch for helping with the data processing, and the Primary Care physicians for contributing to this study. We would also like to thank Dr. Fernando Rico-Villademoros for his help in editing this manuscript, which was funded by Laboratorios Servier S.L.
Please cite this article as: Escudero Rodríguez J-R, Fernández Quesada F, Bellmunt Montoya S. Prevalencia y características clínicas de la enfermedad venosa crónica en pacientes atendidos en Atención Primaria en España: resultados del estudio internacional Vein Consult Program. Cir Esp. 2014;92:539–546.
Content from this article has been previously presented as part of the Vein Consult Program, Epidemiological Study of the UIP (Results in Spain) at the 19th National Congress of the Spanish Chapter of Phlebology of the SEACV, held April 7–9 in Granada.