The extraordinary impact of COVID-19 pandemic on Spanish hospitals has led to a redistribution of resources for the treatment of these patients, with a decreased capacity of care for other common diseases. The aim of the present study is to analyse how this situation has affected the treatment of cholecystitis and cholelythiasis.
MethodsIt is a descriptive national study after online voluntary distribution of a specific questionnaire with Google Drive™ to members of the Spanish Association of Surgeons (AEC).
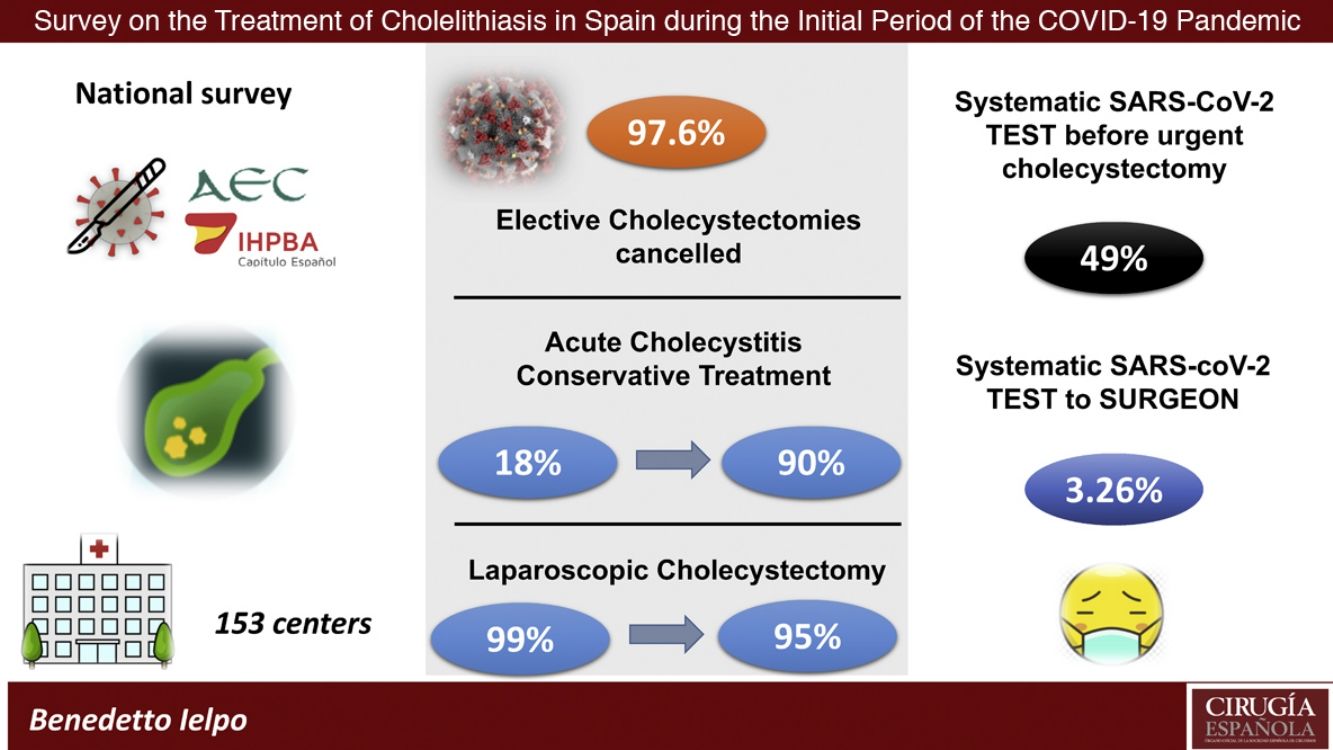
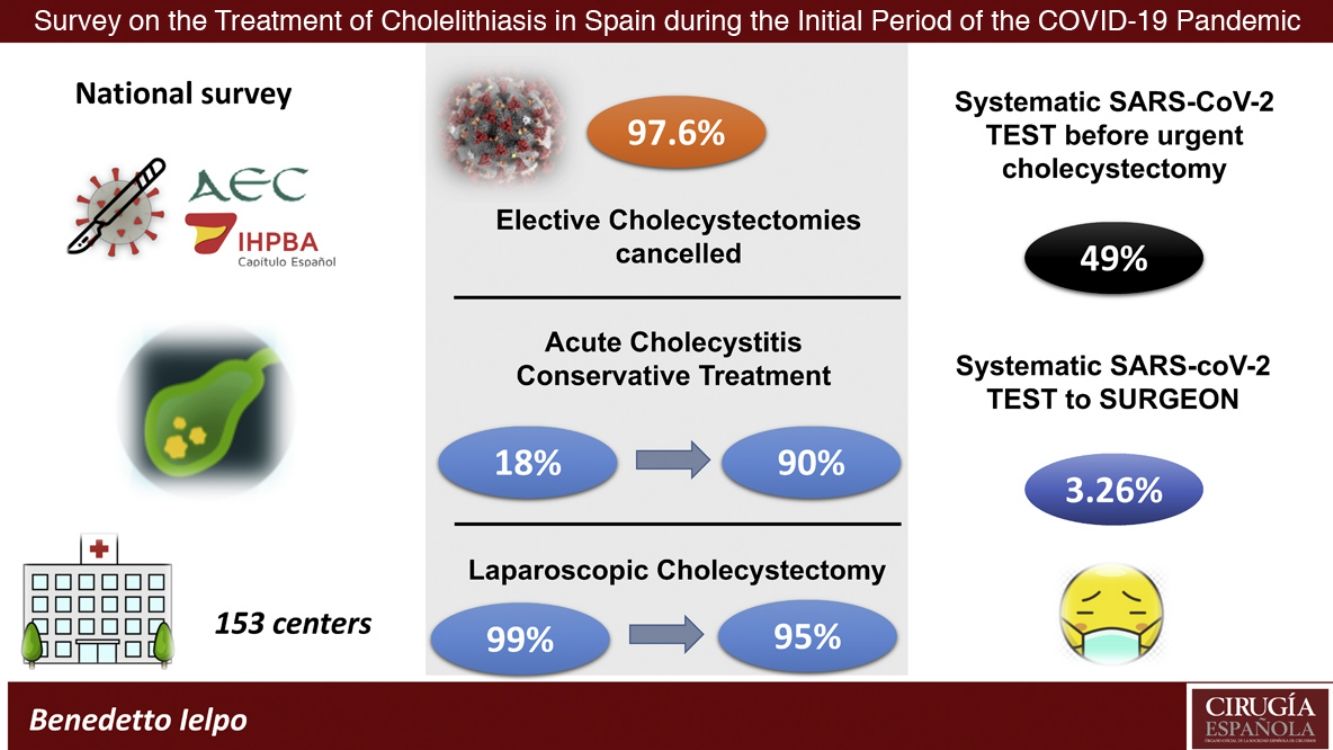
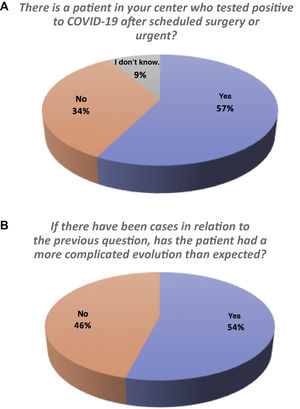
ResultsWe received 153 answers (one per hospital). Elective cholecystectomies have been cancelled in 96.7% of centres. Conservative treatment for acute cholecystitis has been selected in 90% (previously 18%), and if operated, 95% have been performed laparoscopically. Globally, only 49% perform preoperative diagnostic tests for SARS-CoV-2, and 58.5% recognize there have been cases confirmed postoperatively after other surgeries, with worse surgical outcomes in 54%.
ConclusionsThis survey shows that most of the Spanish centers are following the surgical societies suggestions during the pandemic. However, some data requires to be taken into account for the next phase of the pandemic.
La pandemia COVID-19 ha tenido una repercusión extraordinaria sobre los hospitales españoles, que han reorganizado sus recursos para tratar a estos pacientes, limitando su capacidad de atender otras patologías frecuentes. El presente estudio analiza la repercusión sobre el tratamiento de la colelitiasis y la colecistitis aguda.
MétodosSe ha realizado un estudio nacional descriptivo mediante una encuesta online voluntaria, realizada en Google Drive™, distribuida por correo electrónico desde la Asociación Española de Cirujanos (AEC) a todos los cirujanos miembros.
ResultadosSe han recibido 153 encuestas (una por centro). El 96,7% de ellos han suspendido las colecistectomías electivas. El tratamiento conservador de la colecistitis aguda no complicada se ha realizado en un 90% de los casos (siendo previamente del 18%) y, en las colecistitis intervenidas, el 95% ha optado por el abordaje laparoscópico. Un 49% realiza algún test preoperatorio para SARS-CoV-2, y el 57% comunica haber tenido casos de confirmación postoperatoria tras alguna intervención, con peor evolución postoperatoria en el 54%.
ConclusionesEsta encuesta revela que la mayoría de los centros están siguiendo las recomendaciones de las sociedades quirúrgicas durante la pandemia por COVID-19. Sin embargo, se observan algunos datos que precisan ser tenidos en cuenta en las fases sucesivas de la pandemia.
On March 11, 2020, the World Health Organization (WHO) declared that the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) epidemic had reached pandemic status.1 In Spain, since the first case was registered on January 31, 2020,2 the virus has spread rapidly, with a prevalence of 5% according to the ENE-Covid3 national seroprevalence study, reaching 23 521 deaths on April 27, 20204 and a fatality rate of 8.5%.5 However, this figure was probably overestimated due to the large number of undiagnosed infected persons.
The reorganization of human and material resources to guarantee medical care for patients with COVID-19 has directly affected the surgical activity of Spanish hospitals.
Cholelithiasis is a very prevalent disease that affects 20% of the population in developed countries.6,7 It is the leading cause of hospital admission in Europe for digestive disorders,8 with fairly standardized international treatment recommendations.6–9 In order to determine the impact of the COVID-19 pandemic on the management of symptomatic cholelithiasis and acute cholecystitis, a survey was created and sent to Spanish surgeons.
MethodsOurs is a descriptive study of data collected from a survey answered by Spanish surgeons about the treatment of symptomatic cholelithiasis and acute cholecystitis during the first month of the COVID-19 pandemic in Spain.
On April 14, 2020, the AEC and the Spanish Chapter of the IHPBA (CE-IHPBA) sent by email a voluntary online survey, created in Google Drive™ (https://forms.gle/2iHgGbhYzL2vaDVH6), to all their members at Spanish hospitals. Surgeons were requested to complete only one survey per medical center (Appendix B in Additional material), and the questionnaire was re-sent 7 days later (available for 10 days).
The completed surveys were evaluated manually to exclude surveys with multiple entries from the same individual, responses from foreign hospitals, or responses from members of the same hospital, giving priority to the first response received in that case.
The data from the surveys were compared using the McNemar test and the post-hoc test. Categorical variables were reported as numbers and percentages. Differences were considered statistically significant when the P value was <.05. For the statistical analysis, the SPSS program (version 22; Chicago, IL, USA) was used.
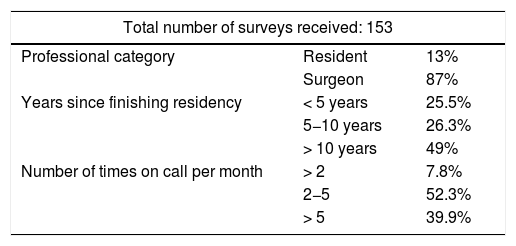
ResultsAfter excluding surveys sent from foreign medical centers (3) or from the same hospital (12), a total of 153 surveys were analyzed. Fig. 1 shows the distribution of responses by autonomous community. The characteristics of the surgeons who completed the survey are presented in Table 1.
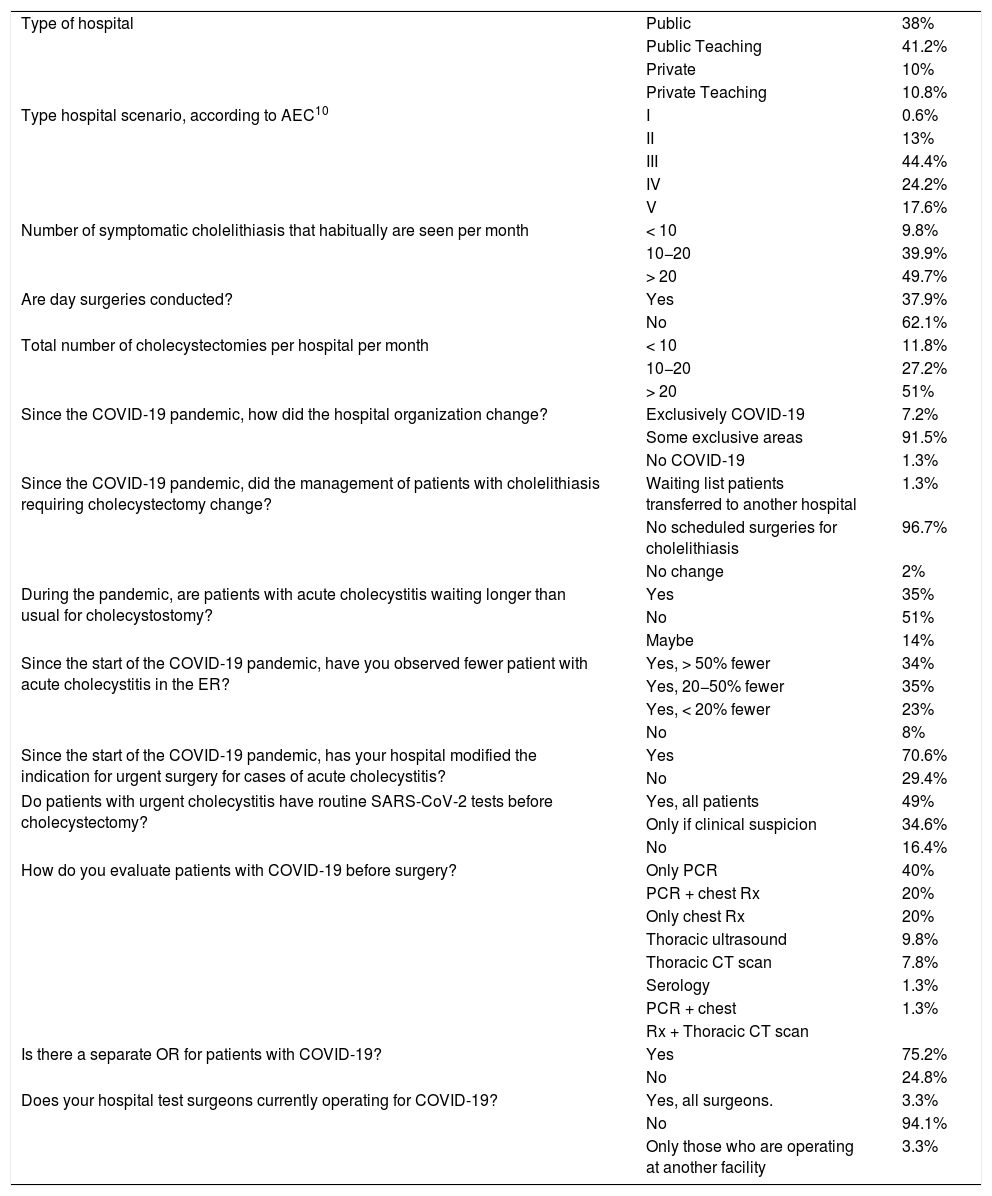
Table 2 demonstrates the scenario of the centers consulted according to the classification proposed by the Surgery-AEC-COVID-19 Working Group.10
Data about the hospitals, organization and management of cholelithiasis.
| Type of hospital | Public | 38% |
| Public Teaching | 41.2% | |
| Private | 10% | |
| Private Teaching | 10.8% | |
| Type hospital scenario, according to AEC10 | I | 0.6% |
| II | 13% | |
| III | 44.4% | |
| IV | 24.2% | |
| V | 17.6% | |
| Number of symptomatic cholelithiasis that habitually are seen per month | < 10 | 9.8% |
| 10−20 | 39.9% | |
| > 20 | 49.7% | |
| Are day surgeries conducted? | Yes | 37.9% |
| No | 62.1% | |
| Total number of cholecystectomies per hospital per month | < 10 | 11.8% |
| 10−20 | 27.2% | |
| > 20 | 51% | |
| Since the COVID-19 pandemic, how did the hospital organization change? | Exclusively COVID-19 | 7.2% |
| Some exclusive areas | 91.5% | |
| No COVID-19 | 1.3% | |
| Since the COVID-19 pandemic, did the management of patients with cholelithiasis requiring cholecystectomy change? | Waiting list patients transferred to another hospital | 1.3% |
| No scheduled surgeries for cholelithiasis | 96.7% | |
| No change | 2% | |
| During the pandemic, are patients with acute cholecystitis waiting longer than usual for cholecystostomy? | Yes | 35% |
| No | 51% | |
| Maybe | 14% | |
| Since the start of the COVID-19 pandemic, have you observed fewer patient with acute cholecystitis in the ER? | Yes, > 50% fewer | 34% |
| Yes, 20−50% fewer | 35% | |
| Yes, < 20% fewer | 23% | |
| No | 8% | |
| Since the start of the COVID-19 pandemic, has your hospital modified the indication for urgent surgery for cases of acute cholecystitis? | Yes | 70.6% |
| No | 29.4% | |
| Do patients with urgent cholecystitis have routine SARS-CoV-2 tests before cholecystectomy? | Yes, all patients | 49% |
| Only if clinical suspicion | 34.6% | |
| No | 16.4% | |
| How do you evaluate patients with COVID-19 before surgery? | Only PCR | 40% |
| PCR + chest Rx | 20% | |
| Only chest Rx | 20% | |
| Thoracic ultrasound | 9.8% | |
| Thoracic CT scan | 7.8% | |
| Serology | 1.3% | |
| PCR + chest | 1.3% | |
| Rx + Thoracic CT scan | ||
| Is there a separate OR for patients with COVID-19? | Yes | 75.2% |
| No | 24.8% | |
| Does your hospital test surgeons currently operating for COVID-19? | Yes, all surgeons. | 3.3% |
| No | 94.1% | |
| Only those who are operating at another facility | 3.3% |
In most of the hospitals surveyed (90.8%), treatment of COVID-19 patients was done simultaneously with the treatment of other pathologies. Only a minority (1.3%) did not treat COVID-19 patients (Table 2).
The usual pre-pandemic surgical practice of the surveyed hospitals is indicated in Table 2. During the pandemic, 96.7% of the hospitals had suspended elective cholecystectomies.
In the management of acute cholecystitis, only 29.4% of those surveyed admitted maintaining the same indications for urgent surgery as before the onset of the health crisis (Table 2).
When a cholecystostomy was indicated, 51% of survey participants believed that the waiting for this procedure did not increase during the pandemic and 8% of hospitals have not detected a decrease in the number of urgent consultations for acute cholecystitis (Table 2).
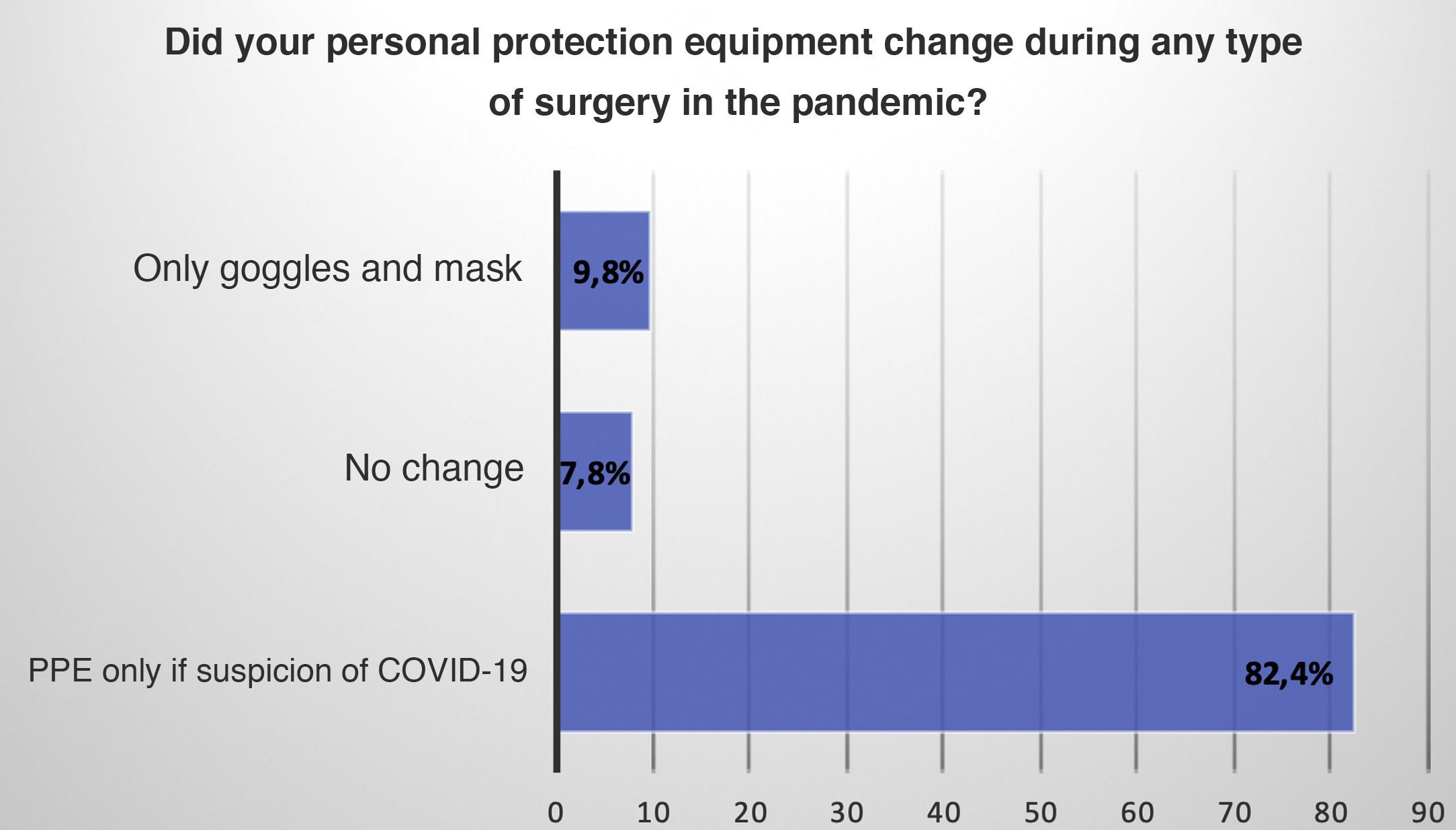
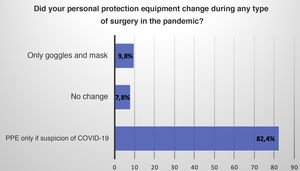
The laparoscopic approach in acute cholecystitis was preferred by 99% of hospitals, and during the pandemic stage this percentage was 95%. Some 27.5% of survey participants were of the opinion that the risk of contamination of healthcare personnel is greater during laparoscopy. The use of personal protective equipment (PPE) was limited to cases with suspected COVID-19 in 82.4% (Fig. 2).
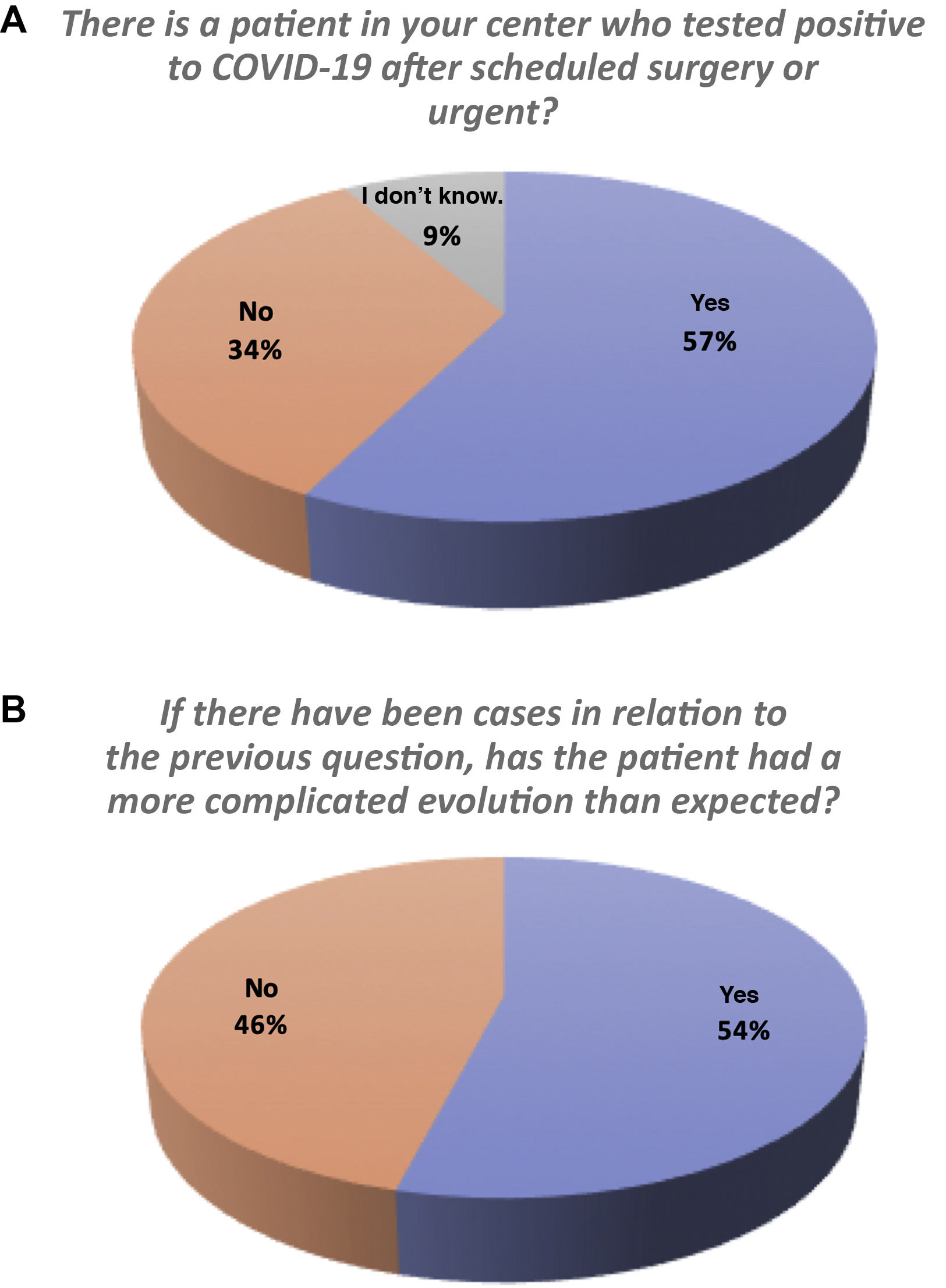
57% of the surgeons reported having had cases of postoperative confirmation of COVID-19, and 54% of these had presented a more complicated postoperative evolution (Fig. 3A and B).
DiscussionTables 1 and 2 show that more than half of the responses came from medical centers with a significant patient volume, performing more than 20 cholecystectomies per month, and the majority (41.82%) have been in a high state of alert.
The impact of the health crisis on surgical services resulted in the cancellation of elective cholecystectomies in 97.6% of the hospitals. This decision was not innocuous, since the annual risk of developing complications in symptomatic cholelithiasis has been estimated at 1%–3%.8 In the next phase of recovery from the pandemic, the national healthcare system will have to design an adequate strategy to perform a high number of cholecystectomies in the shortest possible time. The future recovery of ordinary surgical activity is a challenge where surgeons will have to face longer waiting lists, more complications derived from the delayed surgery, and the risk of perioperative infection by SARS-CoV-2.
Major outpatient surgery is a safe alternative for elective cholecystectomy11,12 in appropriately selected cases, as it reduces the patients’ exposure to in-hospital infection and helps respond to the demand for hospital beds during the pandemic. However, only 37.9% of hospitals have experience in this strategy (Table 1), and it must be implemented in the de-escalation phase. Other initiatives, such as telephone or video consultations13 and the use of absorbable skin sutures, could help reduce the number of in-person visits.
A significant drop has been observed in consultations for acute cholecystitis (Table 2). This is in line with recent publications that describe fewer surgical emergencies, but more advanced disease.14–16 The confinement of the population, the general instructions to go to the hospital only in strictly necessary cases and the fear of intra-hospital infection could explain these facts.
It is controversial whether the pandemic situation should change the surgical indication for acute cholecystitis. There is a general consensus in most of the guidelines17–22 to adopt conservative treatment in suspected or COVID-19–positive patients, for fear that surgery will aggravate the patient’s respiratory condition23 and to minimize the risks of infection of a highly transmissible viral disease.
According to the results of our survey, 57% of hospitals have had cases of postoperative SARS-CoV-2 infection, with an unfavorable postoperative evolution in 54% of the cases (Fig. 3A and B). This experience coincides with other publications23–25 that document greater postoperative complications that could be attributable to this infection. We do not know what complications have developed, and this is a limitation of our study, but it will be the subject of future research.
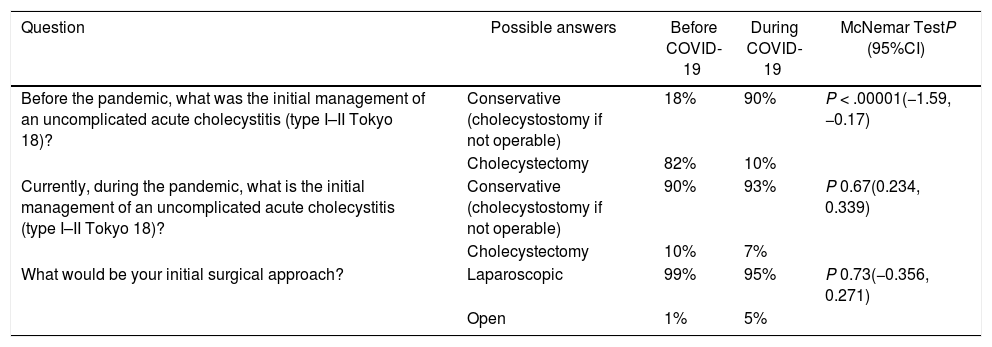
The increased patient load caused by the pandemic and the limited availability of diagnostic tests mean that in many centers this medical treatment strategy has been transferred to the general population, especially in grade I and II cholecystitis, usually surgical,9 where conservative treatment rose from 18% to 90% during the pandemic (Table 3). According to the literature,6,26,27 it is a therapeutic alternative with success rates of 86%, but at the expense of a 22% recurrence of symptoms and a higher percentage of open cholecystectomies in the subsequent hospitalization. The American College of Surgeons advocates urgent cholecystectomy for patients with low surgical risk to minimize hospital stay during the pandemic.28
Changes in treatment of acute cholecystitis before and during the COVID-19 pandemic.
| Question | Possible answers | Before COVID-19 | During COVID-19 | McNemar TestP (95%CI) |
|---|---|---|---|---|
| Before the pandemic, what was the initial management of an uncomplicated acute cholecystitis (type I–II Tokyo 18)? | Conservative (cholecystostomy if not operable) | 18% | 90% | P < .00001(−1.59, −0.17) |
| Cholecystectomy | 82% | 10% | ||
| Currently, during the pandemic, what is the initial management of an uncomplicated acute cholecystitis (type I–II Tokyo 18)? | Conservative (cholecystostomy if not operable) | 90% | 93% | P 0.67(0.234, 0.339) |
| Cholecystectomy | 10% | 7% | ||
| What would be your initial surgical approach? | Laparoscopic | 99% | 95% | P 0.73(−0.356, 0.271) |
| Open | 1% | 5% |
CI: confidence interval.
In addition, the hospitalization of patients with conservative treatment recorded in our survey may be even longer. There were delays for cholecystostomies observed at 35% of the hospitals (Table 2), probably due to the overload of radiodiagnostic services and sick leaves among healthcare staff. Hence, this underlines the importance of surgeons having resources and training to perform percutaneous cholecystostomies.
Therefore, the therapeutic strategy of acute cholecystitis in the epidemiological situation that we find ourselves must be evaluated individually, weighing the benefit of surgery against any existing alternatives, while contemplating COVID-19 status, patient surgical risk, and the resources available at each hospital.18,29
Initially, the fear of aerosolization that could occur with the use of pneumoperitoneum led the Association of Surgeons of Great Britain and Ireland (ASGBI) to advise against the use of laparoscopy during the pandemic, but this was later rectified.21 Although the presence of viruses (such as hepatitis B) has been documented in the pneumoperitoneum,30 there is no current evidence of the transmission of SARS-CoV-2 during laparoscopy,20,31 and it is ethically questionable to deny patients the demonstrated advantages of the laparoscopic approach in acute cholecystitis.20,31 In line with the AEC document,17 95% of surveyed participants initially maintained use of the laparoscopic approach during the pandemic (Table 3). However, 27.45% of medical centers believed that the risk of contamination of staff by SARS-CoV-2 was greater by laparoscopy (Fig. 3B). This fear may be unfounded, and there may even be a lower risk of laparoscopic transmission, given the lower use of sharp instruments and less exposure to body fluids. Therefore, the choice of surgical approach must be made on an individual basis.
It is imperative to adopt a series of precautions to maximize the protection of the surgical team, as recommended by the AEC, SAGES, EAES and other scientific societies.17–19,21,31,32
The use of a filtration system for laparoscopy CO2 evacuation is a widespread practice in Spanish hospitals, with the exception of 27.72% of medical centers. Moreover, as shown by the results of this survey, most hospitals (59.84%) are using systems they have designed themselves, using disinfectant liquids (sodium hypochlorite), filters connected to suction systems or to the water seal (Pleur-evac®),33 which may be due to the lack of adequate filtration material in this first phase of the pandemic. Currently, there is no air evacuation filter system that has been validated against the coronavirus, but this pandemic most likely demonstrates the need for its future development.
Other strategies to reduce the exposure of the surgical team to infection and the surgical risk of the patient focus on minimizing the medical staff required in the operating room and the performance of surgical procedures by surgeons with the greatest experience.17,18,20 The purpose of this proposal is to reduce surgical time and, potentially, the risk of postoperative complications, but it has worked in detriment to the training program for general surgery residents, who actively participate in urgent surgeries, and particularly in cholecystectomies. Most national (AEC) and international (ACS) surgical societies advise against the intervention being performed by surgeons-in-training during the pandemic.18 However, this suggestion has only been put into practice in 52.94% of the hospitals surveyed.
In Spain, 20.2% of reported COVID-19 cases have been healthcare personnel,5 and 26 deaths have been documented,5 including Spanish surgeons. The 23 116 registered cases5 constitute the highest number of infections among healthcare workers reported in Europe and are probably related to the insufficient availability of adequate PPE,34 the lack of systematic screening of asymptomatic carriers during the onset of the pandemic, and the initial absence of separation of healthcare circuits at many hospitals, including the lack of an independent operating room for patients with COVID-19 in 24.8% of those surveyed (Table 2). Currently, surgical societies recommend the use of complete PPE in surgical interventions only if there is clinical suspicion or confirmation of SARS-CoV-2 infection,17,18,20,22 and 82.4% follow these recommendations (Fig. 2).
However, in the current context and with the available diagnostic tests (still in the evaluation phase due to their low sensitivity), it is difficult to safely determine whether a patient is an asymptomatic carrier of the disease. For this reason, in this initial phase, we suggested the universal adoption of PPE and diagnostic tests in all urgent surgeries.
Regarding this latter problem, our survey reveals that 16.4% of hospitals do not perform any diagnostic tests before proceeding with an urgent cholecystectomy (Table 2). These data reflect the heterogeneity of available resources and the geographic variability of prevalence in Spain.3
Routine PCR screening for SARS-CoV-2 RNA, which is performed most frequently (60% of respondents; associated with chest X-ray in 20%), usually entails a delay of 6−8 h before performing the surgery. 20% of the hospitals exclusively use chest X-rays prior to the operation, which could reflect the scarcity of screening tests. 7.8% of hospitals use preoperative chest CT scans, although mostly (90%) as an extension of an abdominal CT scan and not as a specific study (Table 2). Radiological studies are more cost-effective in symptomatic patients, and can occasionally detect disease in paucisymptomatic patients, but their sensitivity for screening has not been established. The combination of diagnostic methods does not manage to solve the difficulty of diagnosing the infection in the incubation phase and in the first days of the clinical symptoms, which is where the highest number of false-negatives PCR tests and CT scans accumulate.18,35,36 Another controversial aspect is the screening of COVID-19 in surgical services. The current protocol of the Ministry of Health reserves the screening test exclusively for health professionals with respiratory symptoms.37 Healthcare workers who have been in close contact with a case are actively monitored, while still maintaining their professional activity. Adherence to this protocol may explain why surgeons are not tested in 94.1% of the hospitals (Table 2). This strategy, and the shortage of effective protection material, has probably contributed to our country becoming the international leader in the number of infected healthcare workers.
Surgeons who are asymptomatic carriers must be identified because they can be a source of infection. Periodic screening of surgeons should be implemented in the de-escalation phase for the safety of patients and medical professionals themselves.18,38
This study reports information obtained exclusively from a survey and should be interpreted within the context of the limited evidence from this type of study. However, in the absence of scientific evidence during this first phase of the pandemic, this study provides relevant information on the patient care provided and the application of the advice of surgical societies in patients with biliary pathology.
In conclusion, the results of our study are testimony to the elevated patient care load and strain felt in Spanish hospitals due to COVID-19. The initial phase of the pandemic has had a very significant impact, causing the suspension of elective cholecystectomies and modifying the treatment of acute cholecystitis.
The results of our survey may facilitate the development of protocols for the treatment of biliary pathology in the de-escalation phase of the pandemic.
Conflict of interestThe authors have no conflict of interests to declare in the writing of this manuscript.
Please cite this article as: Ielpo B, Prieto M, Ortega I, Balibrea JM, Rubio-Pérez I, Juvany M, et al. Encuesta nacional sobre el tratamiento de la colelitiasis en España durante la fase inicial de la pandemia por COVID-19. Cir Esp. 2021;99:346–353.