The sentinel lymph node for melanoma in the lower limbs frequently appears in the inguinal region. However, it may less frequently appear in the popliteal region,1 which is known as the “interval” or “in-transit” sentinel lymph node.2 These cases are usually accompanied by an inguinal sentinel lymph node and, in the case of metastasis in the popliteal sentinel, metastasis in the inguinal node also usually appears.2,3 The fact that the presence of a popliteal sentinel node in some cases is not accompanied by an inguinal lymph node is why the popliteal region is also known as the “minor basin”.3,4 In addition, although even more infrequent, cases have been reported with involvement of the popliteal sentinel node and not of the inguinal sentinel node, and the majority of authors chose not to perform inguinal lymphadenectomy in this situation.4,5 On the other hand, the treatment of patients with metastasis of the popliteal sentinel lymph node has also been debated, and popliteal lymphadenectomy is the treatment of choice for most authors,1,3,6 following general recommendations for the treatment of melanoma.7
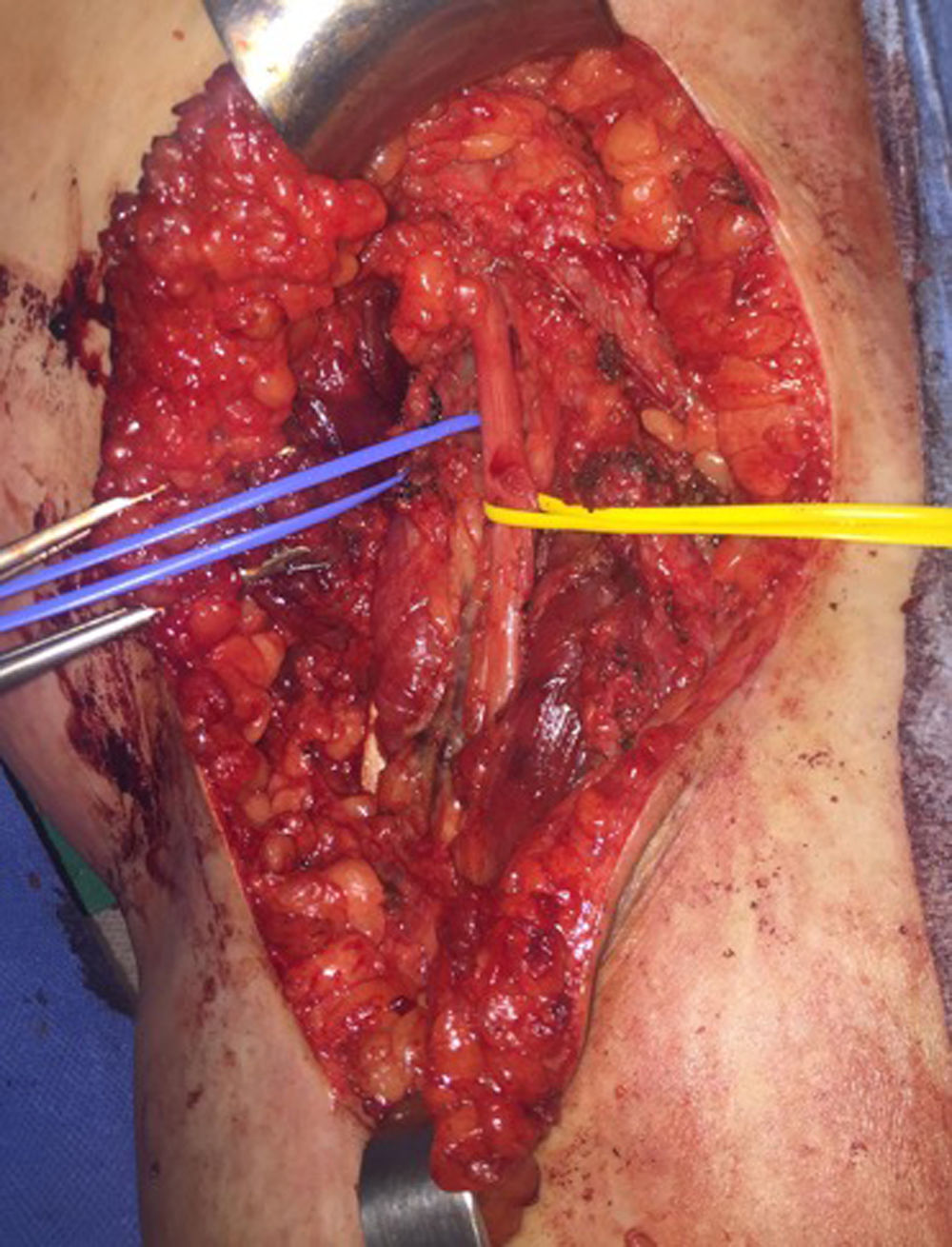
We present the case of a 17-year-old female patient with an ulcerated nodular lesion over a congenital nevus in the posterior region of the right ankle that had been progressing for about 2 months. The histology study of the excisional biopsy reported: superficial spreading melanoma in vertical growth phase, ulcerated, Breslow 3.8mm and Clark IV. The margins were enlarged and the sentinel lymph node was biopsied in a second intervention. Lymphoscintigraphy revealed 2 sentinel lymph nodes, one popliteal (Fig. 1) and another inguinal, and selective biopsies were taken of both. In the cutaneous resection piece, the histology study reported a predominantly dermal melanocytic nevus composed of a congenital pattern with mild dysplasia, which had been completely resected, and 2 hypodermic melanoma nodules, together with a popliteal lymph node with melanoma metastasis and signs of extracapsular extension, and an inguinal lymph node with no evidence of melanoma cells. Subsequently, positron emission tomography with 18F-fluorodeoxyglucose (FDG18-PET) was performed with computed tomography (CT), which was reported as normal. Lymphadenectomy of the right popliteal region was indicated (Fig. 2), but no further lymphadenopathies were found in the histology study. However, the follow-up FDG18-PET/CT performed 3 months after surgery showed evidence of a right femoral lymphadenopathy with a standard uptake value (SUV) of 7.4, suggestive of malignancy. Given this finding, a right inguinal lymphadenectomy was performed, and the lymph node metastasis was confirmed in the histological study together with 3 other lymph nodes that were also affected.
The incidence of the popliteal sentinel lymph node in the case of melanoma in the lower limbs ranges from 1% to 9.6%,1 appearing mainly in lesions distal to the knee and dorsal-lateral.2,8 In general, popliteal lymphadenectomy is recommended in cases of sentinel lymph node involvement,1,3,5,6 which some series report at around 1%.3 Furthermore, in this case the age of the patient and extracapsular involvement of the sentinel node were factors in favor of performing popliteal lymphadenectomy.
In contrast, inguinal lymphadenectomy is not recommended in the event that the sentinel lymph node in this region is negative, as in this case, which is usually an uncommon situation.3–5 However, taking into account the early recurrence of this patient, her progression suggests the opportuneness of having performed the inguinal lymphadenectomy at the onset,9 simultaneously with the popliteal node dissection. Perhaps this should be considered in selected cases that are similar, where extracapsular invasion of the popliteal sentinel node was observed.
The surgical technique for popliteal lymphadenectomy was described by Karakousis.10 The patient is placed in the prone position with the knee slightly flexed; an “S” incision is made. The lateral limit is determined by the biceps femoris muscle proximally and the lateral head of the gastrocnemius muscle distally. The medial limit is determined by the semitendinosus and semimembranosus muscles and the medial head of the gastrocnemius. The identification of the peroneal nerve and the dissection to its origin allows the tibial and the sural cutaneous nerves to be identified. Resection of all the adipose tissue to the popliteal vessels is important. Likewise, it is important to be familiar with the technique, given its infrequency in clinical practice and because it is also a technique that is not free of complications. Consideration should be given to lymphedema, especially in cases that are accompanied by inguinal lymphadenectomy.6 In addition, in cases of metastasis of the popliteal sentinel lymph node where lymphadenectomy has been performed, affected lymph nodes other than the sentinel node are not usually found.2,3 In fact, no other lymphadenopathies are usually found,2 as in our case. Therefore, Kretschmer et al. recommend ultrasound follow-up of the popliteal fossa, considering selective biopsy of the sentinel ganglion therapeutic.8
In contrast, some studies show a greater local recurrence in cases of melanoma with popliteal drainage,3 and the metastasis of the popliteal sentinel node is considered a marker of more advanced disease that causes altered drainage patterns,2 which concurs with the evolution of this patient.
In conclusion, it is essential to know about the possibility of popliteal lymph node involvement in cutaneous melanoma. As for its prognostic importance and management, more extensive series are needed with longer follow-up times in order to standardize its treatment.
Please cite this article as: Febrero B, Rodríguez JM, Piñero A, Ríos A, Parrilla P. Consideraciones terapéuticas de la metástasis en el ganglio centinela de la región poplítea por melanoma. Cir Esp. 2018;96:661–662.