Vascular abnormalities of the breast are rare pathological entities that include congenital malformations of the arteries, veins or lymphatic vessels as well as tumors of vascular, benign or malignant origin (hemangiomas, lymphangiomas, angiosarcomas).1 Regardless of their manifestation type and the age at which they are diagnosed, congenital processes must be differentiated from acquired processes, which are generally tumor forms that appear in isolation or in the context of different syndromes. In the congenital types, lymphatic malformations are usually the most frequent, presenting in the form of cystic lymphangiomas, and their association with vascular structures (especially venous) is relatively rare. The importance of this rare pathology lies in an adequate diagnosis, as these lesions can be confused with breast cancer both clinically and radiologically.
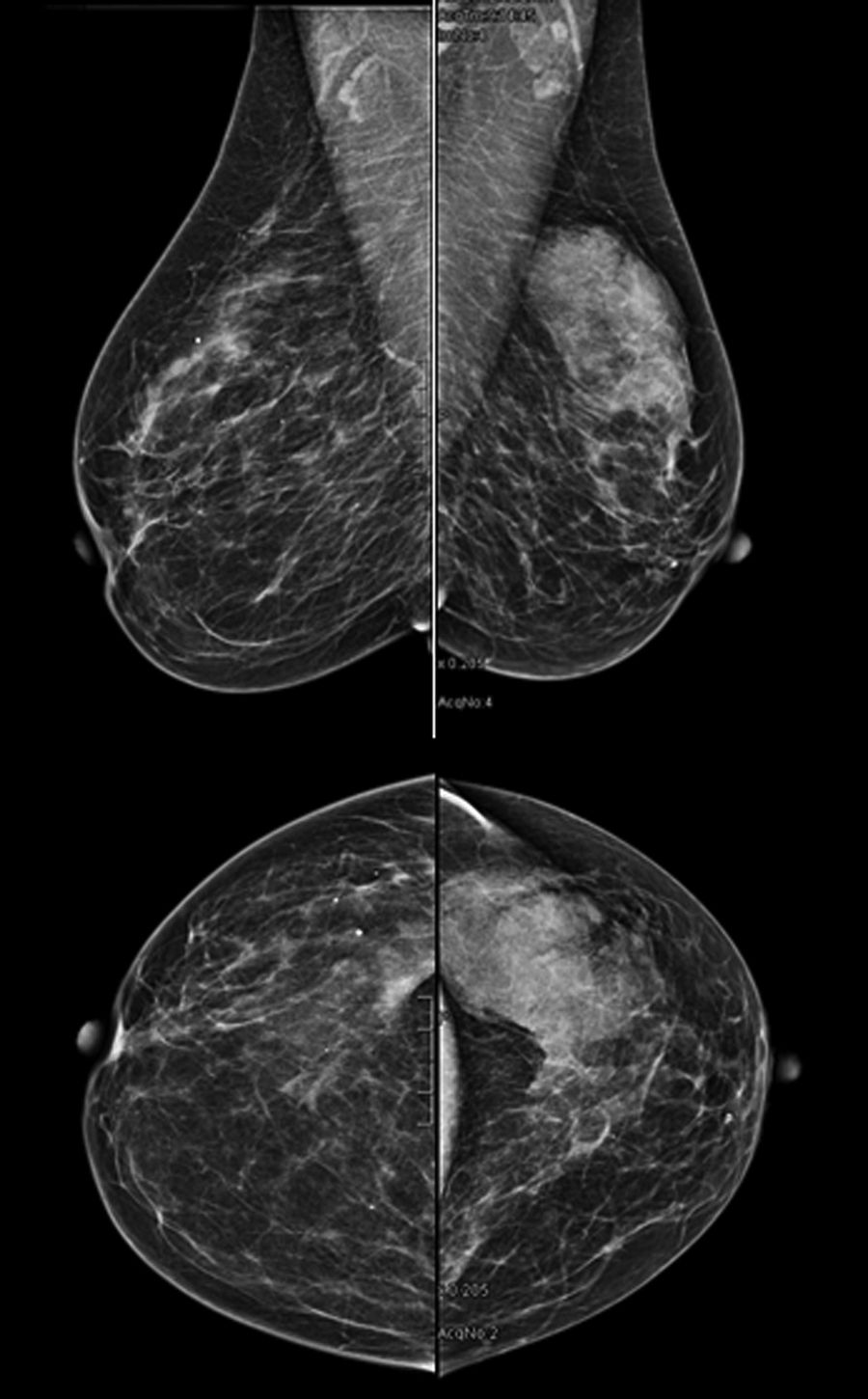
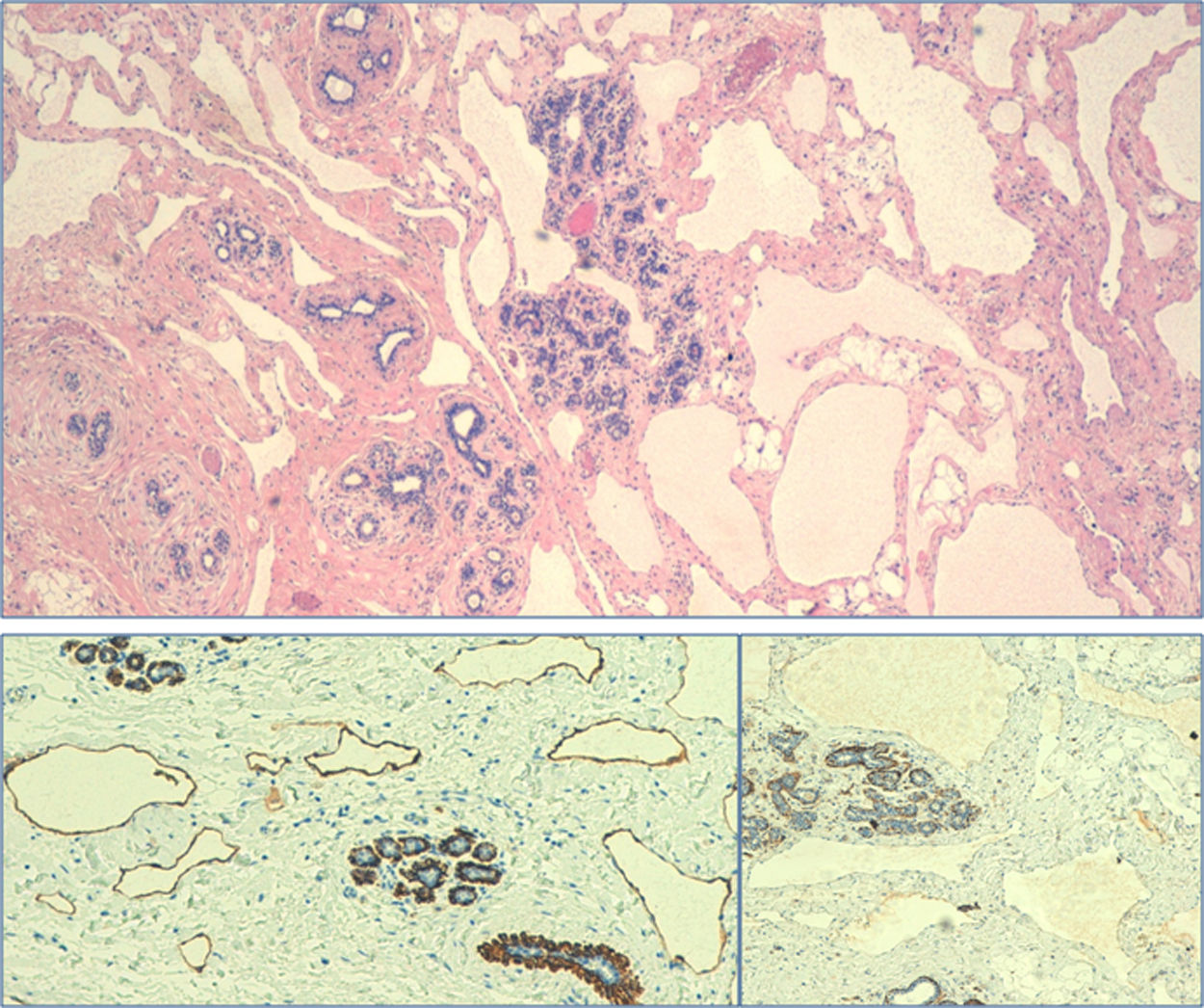
Clinical CaseA 39-year-old woman consulted for a lump in the left breast that had been evolving for several months, with no other symptoms. A mammogram detected a nodule measuring 56×18mm, BIRADS Iva, in the upper-outer quadrant of the left breast (Fig. 1). MRI showed a nodular lesion with progressive and homogeneous enhancement, with thin tracts of hyperenhancement and an ascending type 1 dynamic curve (associated with benign disease), with no suspicious axillary lymphadenopathies. Core-needle biopsy reported compatibility with a vascular-lymphatic malformation, suggestive of lymphangioma. Breast-conserving surgery was performed, during with the lesion was removed with free margins and the breast was reconstructed by mammoplasty. After excision, the definitive histology described a lesion that was soft in consistency and composed of numerous vascular structures of varying sizes that were twisted and thin-walled, covered by a flat endothelial monolayer, without atypia, that was positive for the lymphatic marker D2-40 and negative for WT-1, identified as a mixed vascular lymphatic-venous malformation with lymphatic predominance (Fig. 2). After a 3-month follow-up, the patient remained asymptomatic and had no complications.
Venous malformations are low-flow abnormalities that, unlike arterial malformations, are usually present in breast tissue from birth and become more evident due to growth during puberty or pregnancy, which is when they are usually diagnosed.1 They are alterations in embryonic development, and reference has even been made in the literature to their inherited family character, attributed to certain mutations.2 Although they are usually asymptomatic, they can cause symptoms due to their growth, which in this case is due to hypertrophy and dilation of the vessels involved and not due to hyperplasia. This datum, together with the fact that they do not present growth and spontaneous regression, is a characteristic that allows their distinction from hemangiomas. At diagnosis, low-flow, non-pulsatile, compressible masses may be found with inner thrombotic and coagulopathic phenomena.1
Another group of mixed malformations are hemangioendotheliomas. These are very rare entities that appear as a hypoechoic vascular mass on ultrasound and MRI, as lesions with heterogeneous hypoenhancement in T1 and slight hyperenhancement in T2.3 In the differential diagnosis, stromal pseudoangiomatous hyperplasia should be considered, which is more frequent in premenopausal women; these lesions are found incidentally during a routine study, appearing as masses or asymmetries if there are associated calcifications and showing nonspecific findings on MRI.4 The diagnosis is based on the histology study, where myofibroblasts are seen arranged in false vascular channels containing no red blood cells.3,4
Lymphangiomas are benign lymphatic malformations found mainly in children or young adults.1,5 They are rare tumors, with less than 15 cases reported in the literature.6 According to the number and size of the lymphatic vessels involved, they can be classified as: simple, if the vessels are the size of capillaries; cavernous, when formed by dilated lymphatic vessels; or cystic lymphangiomas, when formed by cystic spaces lined by endothelial cells and filled with lymph fluid. Like hemangiomas, they are usually superficial and their most frequent location is the axilla or tail of the breast, although they do not communicate with the normal drainage of the breast. Radiologically, lymphangiomas usually appear on mammography as well-circumscribed, solitary, lobulated masses, and on ultrasound their appearance depends on the number and size of the lymphatic vessels and cystic spaces involved. Doppler ultrasound does not usually show flow inside the lesion, while MRI may show enhancement of the septa but not of the lymphatic fluid.7,8 Core-needle biopsy usually provides the definitive diagnosis, describing lymphatic vessels that are more or less dilated, as in the case presented. Recently, D2-40 has been used as a selective marker of endothelial lymphatic cells, which would more precisely define their origin. It is an IgG2a monoclonal antibody that is positive in the case of lymphangiomas and is therefore able to establish a differential diagnosis with hemangiomas, angiolipomas and other vascular malformations.9
As for treatment, the management of lymphangiomas is also controversial. Cases have been reported of malignant degeneration in irradiated lymphangiomas (although infrequently), so other treatment options have emerged, such as sclerosis, laser or radiofrequency ablation and radiotherapy.10 To our knowledge, an associated venous component does not seem to affect the subsequent management of these cases.
Conflict of InterestsThe authors have no conflict of interests to declare with regard to this article.
Please cite this article as: Marín C, Galindo PJ, Guzmán F, Ferri B, Parrilla P. Malformación vascular linfovenular de mama: diagnóstico diferencial a propósito de un caso. Cir Esp. 2019;97:541–543.