Before liver transplantation became widely applicable as a treatment option, the mortality rate for acute liver failure was as high as 85%. Today, acute liver failure is a relatively common transplant indication in some settings, but the results of liver transplantation in this context appear to be worse than those for chronic forms of liver disease. In this review, we discuss the indications and contraindications for urgent liver transplantation. In particular, we consider the roles of auxiliary, ABO-incompatible, and urgent living donor liver transplantation and address the management of a «status 1» patient with total hepatectomy and portocaval shunt for toxic liver syndrome.
Antes de que el trasplante hepático fuera una opción terapéutica ampliamente disponible, la tasa de mortalidad del fallo hepático agudo alcanzaba el 85%. En la actualidad, el fallo hepático agudo es una indicación de trasplante relativamente frecuente, pero sus resultados en este contexto son peores cuando se comparan con los de las enfermedades hepáticas crónicas. En este trabajo, tratamos las indicaciones y contraindicaciones para el trasplante hepático urgente. También examinamos el papel del trasplante hepático auxiliar, del incompatible-ABO y del trasplante hepático urgente con donante vivo, así como la utilidad de la realización de una hepatectomía total y un shunt portocava cuando existe síndrome de hígado tóxico en el paciente en alerta cero.
Acute liver failure (ALF) is one of the most dramatic conditions seen in medicine. An inciting factor or event leads to massive hepatic necrosis and a constellation of secondary clinical signs and symptoms, including marked jaundice and severe neurological deterioration, in a period of days to weeks. Historically, the prognosis of ALF was dismal, though advances in patient care and the advent and subsequent application of liver transplantation have led to remarkable improvements in survival. The efficacy of liver transplantation in the context of ALF has never been established through a randomized controlled trial, but to deny certain patients a potentially life-saving option and risk death for the sake of achieving irrefutable evidence is not ethically justified in the modern era. These days, the greatest difficulty in ALF remains knowing when supportive care may be sufficient or when recovery without transplantation is unlikely. In this review article, we discuss how the dilemma is approached and the roles that other non-traditional forms of liver transplantation may play in this setting.
Acute Liver FailureAcute liver failure is a multisystem disorder in which sudden and severe impairment of liver function, with or without encephalopathy, arises in a patient with no history of chronic liver disease.1 In the developed world, there are 1–6 cases of ALF per million persons per year.2–4 Based on its presentation, ALF may be classified as either hyperacute, acute, or subacute, depending on the time between the development of jaundice and the onset of liver failure. However, the importance of this classification has less to do with the temporal evolution and more to do with its association with the underlying cause of disease.5,6
EtiologyIn general, drug-induced injury predominates as the cause of ALF in the United States and most of Western Europe, while viral causes predominate in the developing world.7 The Spanish Group for the Study of Acute Liver Failure demonstrated that in Spain no one particular etiology for ALF prevails: viral hepatitis 37%, unknown cause 32%, drug or toxic reactions 20%, and the rest miscellaneous etiologies.4
While it only accounts for a small proportion of cases in Spain (6%), acetaminophen/paracetamol (APAP) intoxication is the most common cause of ALF in the US and the United Kingdom, and its appearance is characteristically hyperacute.8 Liver injury is typically proportional to the dose of APAP consumed. While currently the majority of cases of APAP-induced ALF are associated with very good rates of spontaneous recovery, others that meet certain clinical criteria, such as an arterial pH <7.25–7.30 despite fluid resuscitation, pose a high risk of rapid deterioration and death.9,10
Idiosyncratic reactions, which occur with drugs other than APAP, are largely unrelated to the amount taken. Most cases occur within the first 6 months after the drug's initiation. While fewer than 10% of affected patients will progress to ALF, up to 80% of those that do will either die or require emergency liver transplantation. In general, drug-induced ALF arises in older patients and follows a subacute course. Deep jaundice, high aminotransferases, and increased age are associated with particularly high mortality rates.11–14
Viral hepatitis has become an infrequent cause of ALF in the US, where approximately 8% and 4% of cases are due to acute hepatitis B virus (HBV) and hepatitis A virus (HAV) infections, respectively.8 However, HBV accounts for 30% of ALF in some parts of Europe and is the main cause in Asia, sub Saharan Africa, and the Amazon basin.4,15–18 Though less than 4% of cases of acute HBV infection lead to ALF, the mortality rate associated with HBV-induced ALF is higher than that associated with either HAV or hepatitis E virus (HEV). Hepatitis B virus has a longer incubation period and prodrome than other causes of viral hepatitis, and older age is associated with a worse prognosis.
Of about 1.5 million cases of acute HAV infection each year, <1% lead to liver failure. HAV-induced ALF is more severe in adults, who more commonly develop subacute disease.19 Hepatitis E virus is the most common cause of ALF in India, Pakistan, China, and Southeast Asia.20 It is more common in pregnant women, particularly in the third trimester, and may be transmitted vertically and result in ALF in the neonate. Other viral causes of ALF are uncommon and include herpes simplex 1 and 2, human herpesvirus 6, varicella zoster, Epstein Barr, cytomegalovirus, and parvovirus B19.
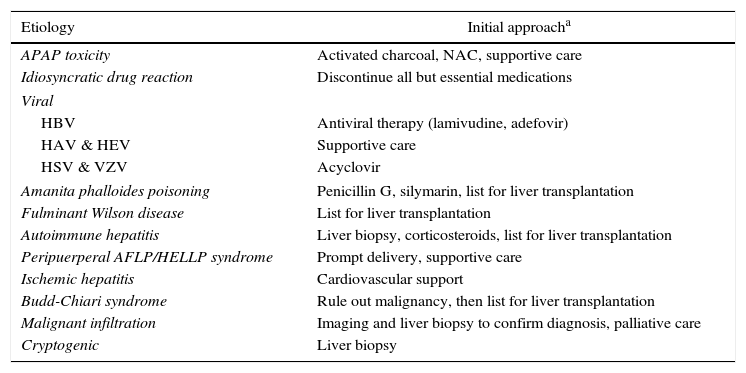
Other less common causes of ALF include Amanita phalloides poisoning21,22; fulminant Wilson disease23,24; autoimmune hepatitis25–27; acute fatty liver of pregnancy/hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome; ischemic hepatitis; acute hepatic vein thrombosis (Budd-Chiari syndrome)28; and malignant infiltration. Depending on the geographical location, around 18%–35% percent of cases may have no identifiable cause.4,8,19 Cryptogenic cases of ALF are associated with particularly poor survival with medical therapy alone; they more commonly have a subacute presentation and frequently require emergency liver transplantation.29,30Table 1 lists the various causes of ALF and the recommended initial approach in each.
Most Frequent Causes of Acute Liver Failure and Recommended Initial Approach in Each.
| Etiology | Initial approacha |
|---|---|
| APAP toxicity | Activated charcoal, NAC, supportive care |
| Idiosyncratic drug reaction | Discontinue all but essential medications |
| Viral | |
| HBV | Antiviral therapy (lamivudine, adefovir) |
| HAV & HEV | Supportive care |
| HSV & VZV | Acyclovir |
| Amanita phalloides poisoning | Penicillin G, silymarin, list for liver transplantation |
| Fulminant Wilson disease | List for liver transplantation |
| Autoimmune hepatitis | Liver biopsy, corticosteroids, list for liver transplantation |
| Peripuerperal AFLP/HELLP syndrome | Prompt delivery, supportive care |
| Ischemic hepatitis | Cardiovascular support |
| Budd-Chiari syndrome | Rule out malignancy, then list for liver transplantation |
| Malignant infiltration | Imaging and liver biopsy to confirm diagnosis, palliative care |
| Cryptogenic | Liver biopsy |
AFLP, acute fatty liver of pregnancy; APAP, acetaminophen/paracetamol; HAV, hepatitis A virus; HBV, hepatitis B virus; HELLP, hemolysis, elevated liver enzymes, low platelets; HEV, hepatitis E virus; HSV, herpes simplex virus; NAC, N-acetylcysteine.
Perhaps the greatest dilemma associated with liver transplantation for ALF is its indication. Indicating liver transplantation too soon risks transplanting a patient with potentially reversible liver dysfunction and unnecessarily subjecting him or her to complex surgery and lifelong immunosuppression. As well, it risks misusing the finite resource that is a transplantable organ. On the other hand, indicating liver transplantation too late risks transplanting a patient who has already developed irreversible sepsis, multisystem organ failure, and/or brain injury. It also risks death of the patient while awaiting transplantation.10,31–33 Regardless of the ultimate decision, however, all patients presenting with ALF should undergo transplant evaluation as soon as possible.
Spontaneous survival occurs in 40%–56% of patients with ALF8,34–36; those that will not achieve sufficient regeneration need to be identified early in the course of their disease. Survival without transplantation for patients with ALF is poor in the elderly and with subacute presentation or severe hepatic encephalopathy.8 Other indications for liver transplantation in ALF may include acute deterioration in mental status, multisystem organ dysfunction, and hypoglycemia.37
The etiology of ALF is perhaps the most important factor in predicting spontaneous survival. In general, outcomes are better for ALF associated with APAP intoxication, HAV, hepatic ischemia, and pregnancy (≥50% transplant-free survival) than for HBV, idiosyncratic drug reactions, Wilson disease, or cryptogenic causes (<25% transplant-free survival).8,38
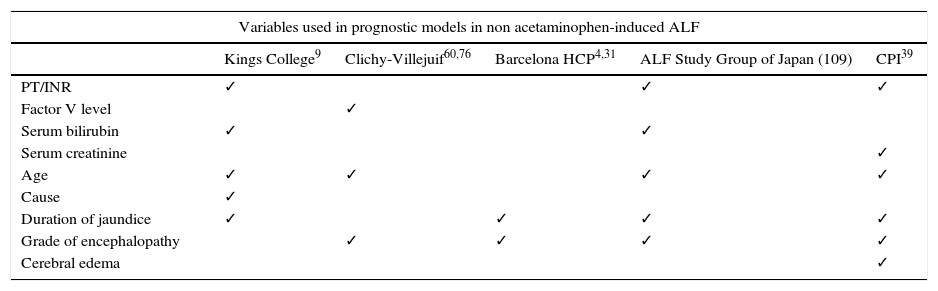
Several prognostic models have been developed to determine the likelihood of spontaneous survival in ALF (Table 2). Among them, the Kings College Hospital criteria, which include models for APAP and non-APAP etiologies, are the most commonly utilized and most frequently tested.9 Even the Model for End-stage Liver Disease (MELD) score, which was initially introduced and validated as a prognostic indicator in chronic liver disease, has found utility in ALF.39,40 In general, while the specificity of these scoring systems is adequate, all suffer from relative lack of sensitivity,41 and accuracy varies based on location.42 Dynamic models taking into account the evolution of critical parameters over time are an attractive means for selecting of ALF patients that would benefit from transplantation, though they need to identify patients in a timely enough fashion so as not to preclude the procedure.43
Prognostic Models for ALF.
| Variables used in prognostic models in non acetaminophen-induced ALF | |||||
|---|---|---|---|---|---|
| Kings College9 | Clichy-Villejuif60,76 | Barcelona HCP4,31 | ALF Study Group of Japan (109) | CPI39 | |
| PT/INR | ✓ | ✓ | ✓ | ||
| Factor V level | ✓ | ||||
| Serum bilirubin | ✓ | ✓ | |||
| Serum creatinine | ✓ | ||||
| Age | ✓ | ✓ | ✓ | ✓ | |
| Cause | ✓ | ||||
| Duration of jaundice | ✓ | ✓ | ✓ | ✓ | |
| Grade of encephalopathy | ✓ | ✓ | ✓ | ✓ | |
| Cerebral edema | ✓ | ||||
Criteria for the selection of patients with ALF for emergency liver transplantation.
CPI, Clinical Prognostic Indicators; HCP, Hospital Clínic i Provincial; INR, international normalized ratio; PT, prothrombin time.
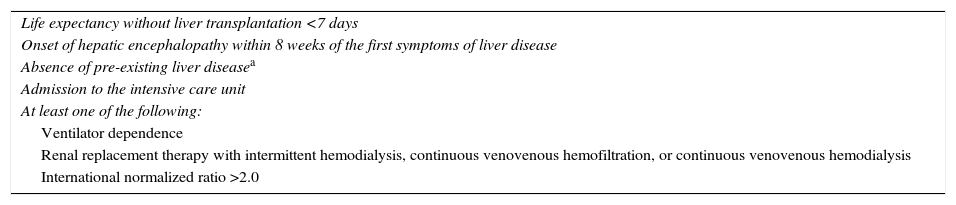
Emergency liver transplantation is the only effective treatment for advanced forms of ALF. Acute liver failure accounts for 6%–9% of all liver transplant activity in the US and Europe.44,45 In Spain, ALF was the indication in 4.7% of the liver transplants performed between 1984 and 2015, a figure that remained stable over the entire thirty-year period.46 Series have shown that 25%–51% of patients admitted with ALF ultimately undergo emergency liver transplantation.8,47,48 The current Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing (UNOS) listing criteria for ALF are included in Table 3. In Spain, patients may be listed for liver transplantation for ALF when the duration of the disease process is <8 weeks and the patient has no underlying chronic liver disease.49
Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing (UNOS) Criteria for Listing a Patient With ALF for Liver Transplantation (“Status 1A”).
| Life expectancy without liver transplantation <7 days |
| Onset of hepatic encephalopathy within 8 weeks of the first symptoms of liver disease |
| Absence of pre-existing liver diseasea |
| Admission to the intensive care unit |
| At least one of the following: |
| Ventilator dependence |
| Renal replacement therapy with intermittent hemodialysis, continuous venovenous hemofiltration, or continuous venovenous hemodialysis |
| International normalized ratio >2.0 |
It is important to identify and even delist patients who are too ill to benefit from liver transplantation. Contraindications include age (center-dependent); extra-hepatic malignancy and other co-morbid conditions that would impact post-transplantation survival; severe cardiac, pulmonary, or multisystem organ failure (continuous norepinephrine infusion >1μg/kg/min, PEEP >12cm H2O and FiO2 >60%, mean pulmonary artery pressure >40mmHg, and/or PaO2/FiO2 <100); active bacterial or fungal infection; and brain death.50–53 Some of the more relative contraindications, such as organ system dysfunction, are age-sensitive, as younger patients are more likely to reverse complications postoperatively.
Special Considerations for the Transplantation ProcedureThere are a few aspects regarding the transplantation procedure worth mentioning. Overall, given the lack of longstanding portal hypertension and portosystemic collaterals, intraoperative hemorrhage is rare. Standard coagulation parameters typically measure only procoagulant factors, but levels of hepatically synthesized anticoagulant factors (e.g., antithrombin and proteins C and S) may also be reduced. The use of viscoelastic methods to more comprehensively study coagulation in this setting indicates that rebalanced hemostasis exists in many patients in ALF.54
Intracranial and cerebral perfusion pressures worsen during native liver hepatectomy, improve during the anhepatic phase, and then rise again during reperfusion.55 The patient's head should be kept up and neutral as much as possible. Care should be taken with the use of volatile anesthetics, which may cause cerebral vasodilation.53 Intracranial pressure monitoring is of unclear clinical benefit in this setting, though its use does appear to be relatively low-risk.56 Hypothermia is an approach that has been thought to help avoid cerebral edema in ALF, though a recent multi-center randomized controlled trial failed to demonstrate a benefit in terms of preventing intracranial hypertension or improving survival.57
Given their propensity to develop profound hypoglycemia, patients with ALF should have blood glucose carefully monitored and corrected throughout the transplant procedure. Serum potassium, phosphate, and magnesium levels should also be checked and repleted as necessary, though caution needs to be exercised in patients in acute renal failure. In these patients, intraoperative continuous venovenous hemofiltration or hemodialysis is likely necessary.
Finally, the necrotic liver is an excellent medium for microbial growth. Though empiric use of antibacterials and antifungals in all patients with ALF is controversial, most clinicians administer these agents to all patients listed for liver transplantation.6
OutcomesOne-year survival rates for emergency liver transplantation are generally 7%–15% lower than those for elective indications; however, they are comparable to those seen in chronic liver disease patients who were in intensive care (64%) or on life support (54%) immediately prior to transplantation.44,45,58,59 According to the Spanish liver transplant registry (RETH), graft and patient survival rates after urgent liver transplantation are 77% and 85% at 1 month and 70% and 76% at 1 year, respectively, rates that are significantly lower than those seen for “elective” transplant indications (92% graft and 95% patient at 1 month, 81% graft and 87% patient at 1 year).46 Most deaths occur within the first 3 months secondary to neurological or septic complications.10,34,60–63
Three large studies from Europe and the United States have defined characteristics associated with a poor outcome after liver transplantation for ALF.10,64,65 Recipient age >45–50 years was identified in all three studies. The studies also identified factors associated with the severity of illness in the recipient (the need for vasopressor support or mechanical ventilation or creatinine >2mg/dL) and graft quality (advanced donor age, ABO incompatibility, partial graft, or steatosis). Compounding risk factors was shown to lead to progressive reduction in survival.
Alternatives to Conventional Liver Transplantation in Acute Liver FailureAcute liver failure causes significant stress in multiple organ systems, and the greatest chance of immediately meeting a patient's metabolic needs and reversing his or her multisystem organ dysfunction is with a high-quality whole-liver allograft from a donor of the patient's own blood type. While awaiting an adequate, let alone optimal, liver graft from a deceased donor, however, an ALF patient might deteriorate significantly or even die. Even in large-volume Western centers, 15%–30% of ALF patients listed for emergent liver transplant may die before transplant can be performed.31,61 Ultimately, it is up to intensivists and transplant surgeons to evaluate the risks and benefits of waiting longer versus proceeding with the transplantation of a suboptimal liver graft.
Auxiliary Liver TransplantAuxiliary liver transplantation (ALT) is the heterotopic or orthotopic implantation of a partial or whole liver graft, leaving behind part or all of the native liver. Auxiliary liver transplantation is an unsuitable approach when the underlying cause of liver failure is fulminant Wilson disease or Budd-Chiari syndrome or when toxic liver syndrome has developed. In theory, ALT should provide hepatic support while the native liver recovers, at which point immunosuppression may be withdrawn and the graft surgically removed or allowed to atrophy. In reality, this goal is only achieved in about one-quarter to one-third of patients undergoing the procedure.66–70 Furthermore, leaving the necrotic native liver in place may lead to multisystem organ failure or native liver cirrhosis in spite of the presence of the auxiliary graft.66,71 Regeneration of the native liver is most likely in patients who are young (<40 years old), who suffer acute viral illnesses or APAP overdoses, and who have a hyperacute presentation,71 though these are the same patients in whom spontaneous rates of recovery are also the highest.
When ALT is performed heterotopically, the liver graft–generally partial–is implanted below the native liver, which is left in place. Though technically easier to perform, heterotopic ALT is associated with a high rate of postoperative complications.67 The graft is implanted onto and may therefore collapse the infrahepatic inferior vena cava. The heterotopic graft also competes with the native liver for portal inflow, which slows native liver regeneration and may lead to portal vein thrombosis.67
In orthotopic ALT, a portion of the native liver is resected and replaced by a corresponding partial graft (typically left hemiliver or left lateral segment in children, right hemiliver in adults). Inflow is divided between the native and auxiliary livers, raising concerns about competition for portal inflow.72–74 Biliary, infectious, and neurological complications occur at higher rates than in standard orthotopic liver transplantation.61,68 As in living donor liver transplantation (LDLT), a partial graft of adequate size and quality must be provided (in general, >1% of the recipient's body weight). Though results tend to be better for this approach than for heterotopic ALT, orthotopic ALT is very technically demanding and should only be performed by surgeons experienced in hepatic surgery and LDLT.
Abo-Incompatible Liver TransplantOriginally, the justification for performing ABO-incompatible liver transplantation in the context of ALF was based on the following: (1) when certain clinical indicators were present, mortality in ALF was virtually 100%9,75; (2) when indicated, liver transplantation had to be performed as soon as possible to prevent the development of catastrophic neurological sequelae76; and (3) there was no effective hepatic replacement therapy to bridge a patient with ALF awaiting a liver.77 Furthermore, there was circumstantial and experimental evidence to suggest that the liver was relatively resistant to the effects of humoral immunity. Subsequent clinical experience, however, has shown us that hyperacute rejection is, in fact, a serious problem in ABO-incompatible livers, arising in up to 20% of recipients.78
Overall, ABO-incompatible liver transplantation is associated with higher rates of recipient complications, including acute and hyperacute rejection, vascular thrombosis, and biliary injury.78,79 Complications arising in this context appear to be relatively resistant to conservative therapy and ultimately require re-transplantation in the majority of cases.78 Furthermore, while the use of plasmapheresis and higher doses of immunosuppression may help decrease rejection, they do so at the cost of simultaneously increasing infectious complications among recipients.78 ABO-incompatible liver transplantation is also associated with significantly lower patient and graft survival rates: 75% and 52% versus >80% and 75% at 1 month for ABO identical/compatible grafts according to the RETH.46 Given these facts, most European transplant organizations have abandoned the use of ABO-incompatible liver transplantation, even in emergency situations.58
Urgent Living Donor Liver TransplantationA few case series have been published on the use of LDLT in patients with ALF.80–86 Immediate graft function is usually excellent if adequate hepatic mass is provided.84 Furthermore, LDLT is the only option in countries without brain death laws. However, to avoid progressive neurological dysfunction in the recipient, the donor evaluation is done in very rapid fashion, sometimes in as little as 6h.52,81,84 Most potential donors are siblings, children, and/or spouses, who are influenced by the patient's imminent death. The potential to select inappropriate donors is higher in this setting, as are concerns about subtle donor coercion and the veracity of informed consent.
Patients undergoing emergent liver transplantation are very sick and depend on immediate excellent graft function, more so than patients undergoing elective procedures. Almost all liver transplant surgeons would agree that urgent LDLT needs to ensure adequate graft size (at least 0.8% if not 1% of the recipient's body weight).81,84,86 In Western medical centers, this frequently requires the transplantation of a right hemiliver graft, which is associated with relatively high rates of donor morbidity (38%–44%) and not insignificant rates of donor mortality (0.2%–0.9%).87–92
Taking all these facts into consideration, several organ transplant and other healthcare organizations have made recommendations against the use of LDLT in ALF.85,93,94 However, there is little argument that urgent LDLT may play an important role in the pediatric setting, in which the donor procedure (typically a left lateral sectionectomy) is considerably safer and deceased donors of an appropriate size are scarce. Recipient one-year survival rates range from 67% to 89%, and the life-saving potential of emergent pediatric LDLT appears to outweigh the associated risks and ethical concerns.81,95,96
Total Hepatectomy and Portocaval Shunt for Toxic Liver SyndromeOnce a patient with ALF has been listed for transplantation, the greatest obstacle lies in keeping the patient stable until a donor organ becomes available. While awaiting a new liver, the patient's own necrotic liver may become a significant source of toxic vasoactive compounds, provoking refractory metabolic acidosis and circulatory, renal, and respiratory failure in a condition known as “toxic liver syndrome”. The suggestion was made, however, that by eliminating the source of toxins (i.e., the native liver), other organs may recover. It was supported by the observation that intracranial and cerebral perfusion pressures tended to improve dramatically during the anhepatic phase of liver transplantation.55,97–99 Ultimately, this has prompted some groups to perform “two-stage” liver transplant procedures for toxic liver syndrome.
In the two-stage procedure, emergency hepatectomy is performed in advance of the arrival of a transplant allograft, oftentimes without even knowing if one will become available. A portocaval shunt is created, and the patient is left anhepatic. During the anhepatic period, the patient is typically bridged with continuous hemofiltration or hemodialysis in the intensive care unit or the operating room itself.100–102
In 1993, Ringe and colleagues described the first and largest series of total hepatectomy and portocaval shunt.102 A total of 32 consecutive patients were included, among whom the initial indication was toxic liver syndrome (No.=25), uncontrollable hepatic hemorrhage (No.=6), and unresectable tumor of the proximal bile duct (No.=1). Thirteen patients died anhepatic, none of whom showed any signs of stabilization or improvement after hepatectomy, while 19 patients underwent transplantation after a mean anhepatic time of 16.5h (range 6.6–41.5). Nine of the transplanted patients died, among whom sepsis was the cause of death in seven, and ten ultimately survived (31%). The authors noted that while most patients with unsalvageable trauma and an early hepatectomy survived, prolonged hepatic ischemia and extensive hepatic necrosis carried a significantly increased risk of death from sepsis, even when liver transplantation could successfully be performed.
Total hepatectomy and portocaval shunt should be performed before the onset of infection and irreversible multisystem organ failure; knowing when to do so, however, is difficult. Overall, improvements in hemodynamic parameters and/or metabolic acidosis and the lack of overt signs of infection when total hepatectomy is performed appear to be the most important predictors of a successful outcome for subsequent liver transplantation.102,103
ConclusionsLiver transplantation has improved the prognosis in ALF significantly; the biggest difficulty facing the clinician remains knowing when it is indicated. Continuous assessment of the patient's evolution is critical to avoid the development of complications that will negatively impact the postoperative course or preclude transplantation altogether. The “gold standard” for the surgical treatment of ALF is still orthotopic liver transplantation with a whole graft. Auxiliary liver transplant should be applied cautiously and only at centers with expertise in hepatic surgery. ABO-incompatible grafts should be avoided, if at all possible. Urgent LDLT raises ethical concerns but may be a good option for children and the only option for adults in certain parts of the world. Finally, in some patients, the timely application of hepatectomy and portocaval shunt may be beneficial, though knowing when to do so is difficult.
Conflicts of InterestThe authors declare no conflicts of interest.
Please cite this article as: Hessheimer AJ, Nacif L, Flores Villalba E, Fondevila C. Trasplante hepático debido a fallo hepático agudo. Cir Esp. 2017;95:181–189.