Primary leiomyosarcoma of the inferior vena cava (IVC) is a rare mesenchymal tumor with a poor prognosis.1 Only 300 cases have been reported,1,2 so the data available to guide us in their treatment are very limited. Detailed case reports case can help make appropriate decisions for the proper management of future patients.
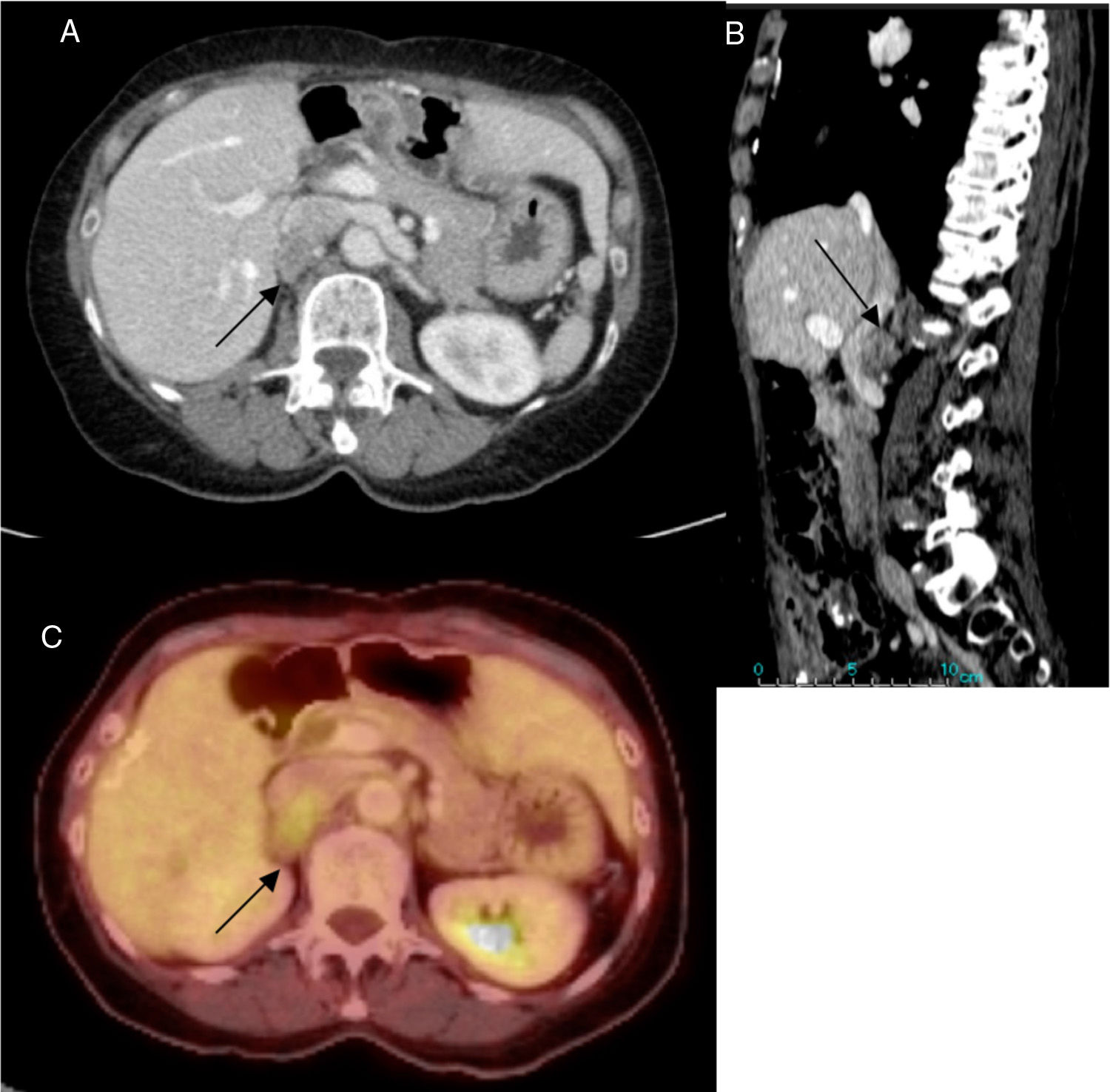
Our patient is a 63-year-old woman with multiple previous abdominal surgeries due to colon adenocarcinoma with liver metastases. The follow-up computed tomography (CT) scan detected a new 27-mm retroperitoneal nodule that was dependent on the posterior wall of the IVC (Fig. 1). After fine-needle aspiration (FNA) biopsy, she was diagnosed with primary leiomyosarcoma of the IVC. The patient was asymptomatic.
Through exploratory laparotomy and after complex adhesiolysis, a solid tumor was evident from the infrahepatic vena cava to the origin of the left renal vein and attached to the right adrenal gland. No invasion of other intra-abdominal structures was observed.
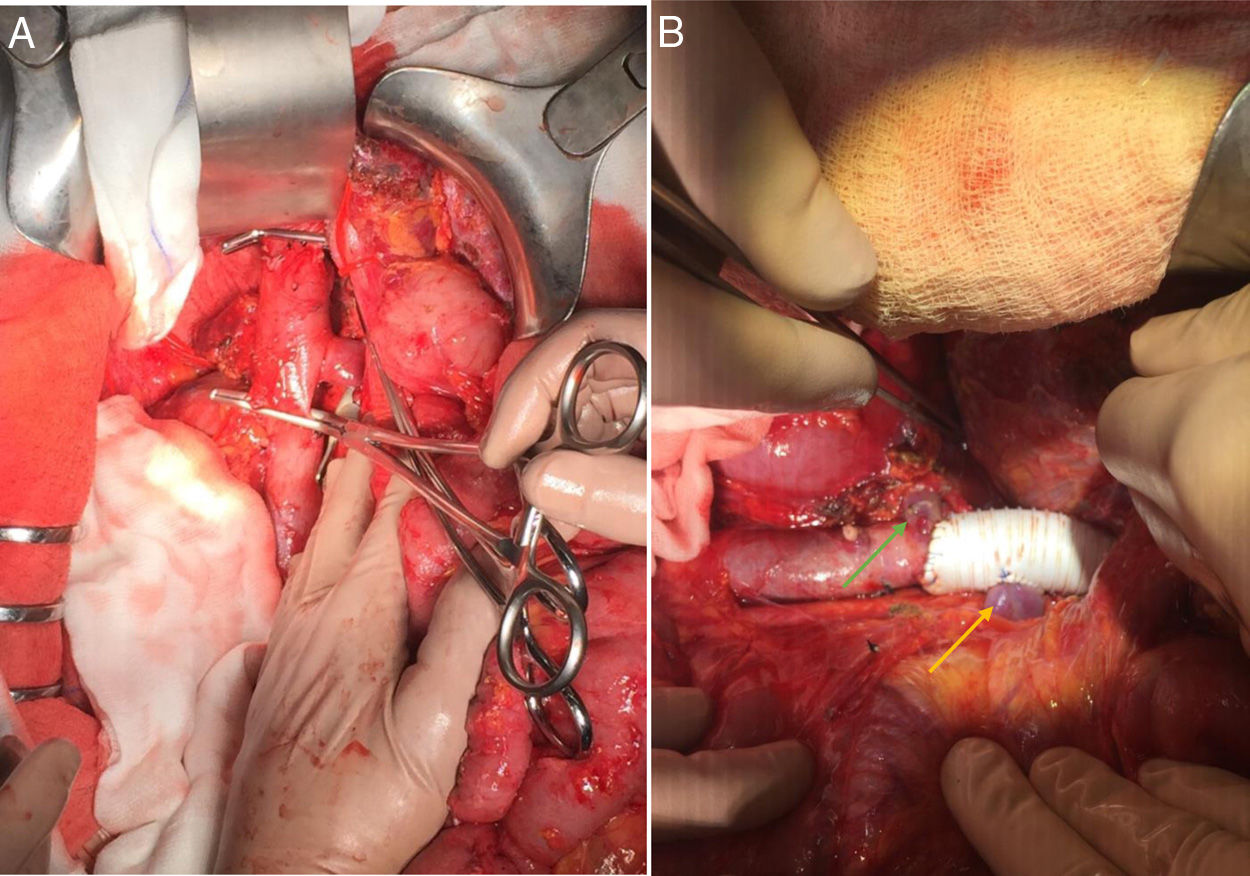
After clamping the retrohepatic vena cava, left renal vein and the confluence of the right renal vein (Fig. 2A), en bloc cavectomy was performed with the right adrenal gland. The flow was reconstructed with a 20-mm ringed polytetrafluoroethylene (PTFE) graft, with direct re-implantation of the left renal vein (Fig. 2B). The definitive pathology results confirmed the diagnosis of primary vascular leiomyosarcoma. Resection margins were tumor-free. After 24h in the intensive care unit, the patient was moved to the floor with no signs of vascular compromise.
(A) Vascular clamping of the retrohepatic vena cava, origin of the left renal vein and confluence of the right renal vein prior to cavectomy and en bloc resection with the right adrenal gland. (B) Vascular reconstruction using a ringed PTFE graft and direct re-implantation of the left renal vein (yellow arrow); origin of the right renal vein at the resection edge (green arrow).
Due to intestinal perforation, re-operation was necessary on the third postoperative day. The subsequent patient progress was satisfactory, and she was discharged on the tenth postoperative day with no signs of infection or graft thrombosis on follow-up CT. Seven months later, there are no data of tumor recurrence, thrombosis or prosthetic infection.
Inferior vena cava leiomyosarcoma is a rare, locally very aggressive, malignant tumor with slow growth, which means that they can remain asymptomatic until advanced stages of the disease.1 The most frequent location is infrarenal.3
Currently, en bloc surgical resection is the only potential cure. Complete exeresis with free margins increases long-term survival.4–6
Different grafts can be used for the reconstruction of the inferior vena cava. However, given the limited number of case reports, there is no consensus about which technique or material is most appropriate.
Some authors advocate venous grafts or primary suture with the aim of reducing the risk of infections or thrombosis.3,7 However, authors like Michael et al.6 highlight several technical factors that, even today, are the subject of debate.
When PTFE grafts are used, some suggest the use of ringed grafts to prevent collapse. In contrast, others argue that this type of grafts have worse tissue integration and may predispose patients to the formation of entero-prosthetic fistulae to the duodenum.1–6 In the case of our patient, we used a ringed PTFE graft as described, which is the most widely used surgical technique, in association with coverage by the greater omentum to prevent the formation of fistula tracts.
In patients with involvement of the middle segment, we must also consider whether to reconstruct the renal veins. In the case of the right renal vein, the need for restoration of flow is inexorable; however, on the left side, the renal vein could be ligated due to the presence of collateral circulation.
In our patient, the tumor reached the origin of the left renal vein. In this case, we opted for direct re-implantation to the PTFE prosthesis in order to reduce the risk of subsequent renal disease that would further increase the morbidity of the procedure.
Recent studies advocate neoadjuvant radiotherapy (RTx) for the management of inferior vena cava leiomyosarcoma. It may help improve local control of the disease7,8 and could even facilitate tumor resection due to the induction of local tissue edema and parietal thickening of the IVC caused by RTx.8 However, until now, there is no global consensus on the efficacy of neoadjuvant RTx in this type of neoplasms.
There is also no consensus on the value of chemotherapy, and its use is restricted to patients with progression, tumor recurrence or metastatic disease.3,8 We opted for surgical management as our only treatment, due to the limited evidence available on these treatments and the absence of data on involvement of neighboring organs or distant metastases in the preoperative study.
Thus, leiomyosarcoma of the IVC is a clinical and surgical challenge. En bloc R0 resection is essential to achieve healing, and the role of RTx and chemotherapy in the prognosis of these patients is still unknown as it mainly depends on the location, degree of tumor extension and cellular aggressiveness, as well as the possibility of complete excision with tumor-free surgical margins.
Please cite this article as: Puerta A, Vilar JA, Núñez J, López Hervás P, Nuño J. Leiomiosarcoma de vena cava inferior. Cir Esp. 2020;98:243–245.