Gastric volvulus is an uncommon clinical condition and is associated with type II–III hiatal hernias. Its acute presentation constitutes a surgical emergency. Despite its low frequency, results of laparoscopic treatment have already been published.
Material and methodsA retrospective study was performed on all cases diagnosed with gastric volvulus undergoing laparoscopic surgery between 1998 and 2010. The surgical technique, the post-operative outcome, and the clinical follow-up are described.
ResultsA total of 10 cases were identified, one was a primary gastric volvulus, and the remainder were secondary. A laparoscopic anterior gastropexy as the sole procedure was performed on 7 patients. A Nissen fundoplication with mesh reinforcement of the crural closure was performed on the 3 remaining cases. Postoperative outcome was uneventful in 9 patients, with an early start of the diet, and hospital discharge between 48 and 72h. After a mean follow-up period of 18 months, radiological hernia recurrence occurred in one case but recurrence of the volvulus was not observed.
ConclusionLaparoscopic anterior gastropexy is, in our experience, an effective and safe procedure with a low morbidity, for the treatment of acute gastric volvulus in patients with high surgical risk.
El vólvulo gástrico es una entidad clínica poco frecuente y se asocia a hernias hiatales tipo II–III. Su presentación aguda constituye una urgencia quirúrgica. Pese a su baja frecuencia, ya se han publicado resultados sobre el tratamiento laparoscópico.
Material y métodosEstudio retrospectivo de todos los casos diagnosticados de vólvulo gástrico agudo intervenidos por vía laparoscópica desde 1998 a 2010. Se describe la técnica quirúrgica, la evolución postoperatoria y el seguimiento clínico.
ResultadosSe identificaron 10 casos, uno era un vólvulo primario y el resto secundarios. A 7 pacientes se les realizó una gastropexia anterior como único procedimiento. En los 3 restantes se llevó a cabo fundoplicatura de Nissen y cierre de los pilares con refuerzo protésico. La evolución postoperatoria fue favorable en 9 pacientes, con inicio precoz de la dieta y alta en 48–72h. Con un seguimiento medio de 18 meses, solo hemos constatado una recidiva herniaria radiológica y ninguna recidiva del vólvulo.
ConclusiónLa gastropexia anterior por laparoscopia es, en nuestra experiencia, un procedimiento efectivo y con baja morbilidad para el tratamiento del vólvulo gástrico agudo en pacientes con elevado riesgo quirúrgico.
Gastric volvulus involves an abnormal rotation of the stomach around one of its axis that causes luminal obstruction, which may be temporary and reversible. Cases with abrupt onset, however, can lead to gastric ischemia, either with or without associated respiratory distress. In these cases, morbi-mortality reaches 80%,1 representing a surgical emergency. The volvulus can be either primary, due to weakness or laxness of normal gastric supporting structures, or, more frequently, secondary, associated with type II–III hiatal hernias. Classic surgical treatment of chronic gastric volvulus consists of correction of the etiopathogenic factors. Laparoscopic surgical repair has been shown to be safe and effective2,3 in addition to offering the patient the advantages of minimally invasive procedures.3,4 However, the acute form of presentation is very rare and experience in treating this entity is therefore very limited. Treatment is also made more difficult by a series of factors such as the patient's age (which is generally older), associated comorbidities and the clinical situation of the patient. Nonetheless, results have been published for laparoscopic treatment of acute gastric volvulus by means of anterior gastropexy.5
The objective of this study is to present the clinical and radiological results of 10 patients diagnosed with acute gastric volvulus who were treated laparoscopically.
Materials and MethodsOurs is a retrospective study of a series of patients diagnosed with acute gastric volvulus from January 1998 to December 2010 who were operated on laparoscopically. Excluded from the study were those patients who had been diagnosed with gastric volvulus by imaging tests during hiatal hernia studies and had not presented volvulus symptoms.
The complementary examinations used in the diagnosis were: chest radiography, gastrointestinal transit study and computed tomography.
Surgical TechniqueThe surgical procedures were performed by the laparoscopic approach. Patients were placed in a semi-sitting position with the lower limbs in abduction; the trocars were set in a position similar to that used in the treatment of gastroesophageal reflux disease: 11-mm trocars in the mesogastrium, left hypochondrium, left flank and subxiphoid area, and a 5-mm trocar in the right hypochondrium.
Two surgical techniques were used: laparoscopic anterior gastropexy as a single procedure, with points of fixation from the fundus to the diaphragm and the greater curvature to anterior parietal peritoneum; or hiatal repair with hernia reduction, resection of the sac and a short, loose Nissen fundoplication and prosthetic hiatal reinforcement. We used a 10cm×5cm preformed mesh with polypropylene on one side and silicone on the other (in contact with the organs) and a central silicone reinforcement ring.
After hospital discharge, the patients were scheduled for follow-up appointments 15 days after surgery. At this time, GI transit studies were ordered and repeated yearly.
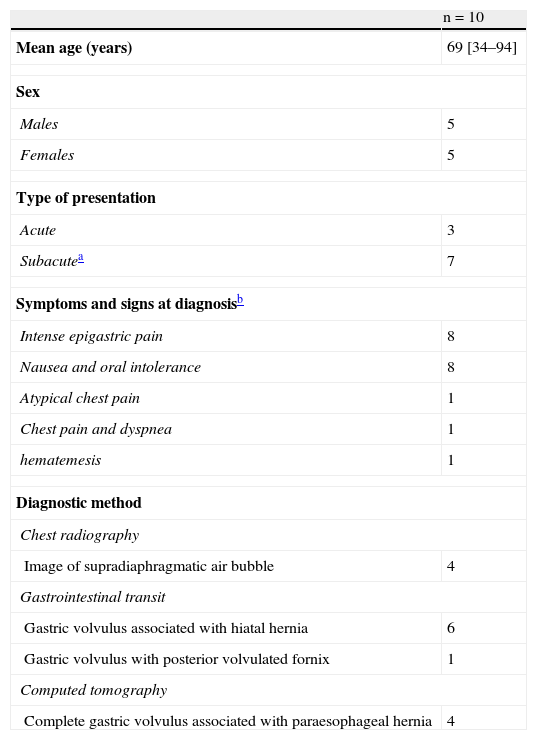
ResultsDuring the study period, 10 patients were identified with the diagnosis of acute gastric volvulus (5 men and 5 women) with a mean age of 69 (range 34–94) (Table 1). Only 2 patients had presented previous transitory episodes of volvulus, which they had not consulted for. The most frequent symptoms at the time of diagnosis were intense epigastric pain with nausea and intolerance to oral intake, presented by 8 patients; other symptoms at onset were atypical chest pain accompanied by vagal response and orthopnea, atypical chest pain with dyspnea and hematemesis (Table 1).
Clinical Characteristics of the Patients.
| n=10 | |
| Mean age (years) | 69 [34–94] |
| Sex | |
| Males | 5 |
| Females | 5 |
| Type of presentation | |
| Acute | 3 |
| Subacutea | 7 |
| Symptoms and signs at diagnosisb | |
| Intense epigastric pain | 8 |
| Nausea and oral intolerance | 8 |
| Atypical chest pain | 1 |
| Chest pain and dyspnea | 1 |
| hematemesis | 1 |
| Diagnostic method | |
| Chest radiography | |
| Image of supradiaphragmatic air bubble | 4 |
| Gastrointestinal transit | |
| Gastric volvulus associated with hiatal hernia | 6 |
| Gastric volvulus with posterior volvulated fornix | 1 |
| Computed tomography | |
| Complete gastric volvulus associated with paraesophageal hernia | 4 |
The complementary studies used for diagnosis revealed that the etiology of the volvulus was primary in one patient and secondary to type II–III hiatal hernia in the remainder.
One patient was immediately operated on due to associated severe respiratory failure caused by the intrathoracic compression of the volvulus. Pneumoperitoneum was adequately tolerated and improved after gastric reduction. In the remaining 9, surgery was able to be delayed an average of 72h (range 48–120h) after symptoms had been alleviated with gastric decompression with a nasogastric tube (NGT) in 7 patients or endoscopically in 2. In all cases, the laparoscopic approach was used. Anterior gastropexy was the only technique performed in 7 patients: in 5 cases of elderly patients with severe comorbidity, in one patient with primary volvulus and in another case due to the patient's poor general state. The 3 patients with volvulus secondary to type III hiatal hernia, good general state and no relevant comorbidity underwent hernia repair. No cases had a NGT left in after surgery.
Post-operative evolution was favorable in 9 patients; oral diet was initiated after 24h and patients were discharged in 48–72h. The patient who underwent emergency surgery presented severe respiratory failure that required the insertion of thoracic drains due to the presence of bilateral pleural effusion and prolonged orotracheal intubation. This patient remained in the ICU, with a total post-operative hospital stay of 21 days. In the remaining patients, no complications were registered in the short- or medium term.
Mean follow-up was 18 months (range 6–96 months). A hernia recurrence was detected with follow-up radiography 18 months after surgery in one patient who had undergone a classic repair, although there was no radiological progression during the 7 years of follow-up. This patient as well as the remaining subjects all remained asymptomatic. A high number of patients were lost to follow-up after the second year; only 4 patients (3 with classic repair and one with gastropexy) completed follow-up periods longer than 36 months and are currently alive.
DiscussionGastric volvulus is a rare clinical entity that involves abnormal rotation of the stomach on one of its axis, causing luminal obstruction and risk of ischemia.
Its most frequent presentation is chronic, which is associated with type II–III hiatal hernias.6 Clinically, it may run its course either without symptoms or with a series of non-specific symptoms, such as the sensation of abdominal fullness, intermittent epigastric pain that occasionally radiates toward the left hemithorax, chronic anemia, dysphagia or meteorism.
However, gastric volvulus may occur abruptly and cause characteristic symptoms described by Borchardt in 1904: acute epigastric pain, unproductive vomiting and inability to insert an NGT.7
Thus, symptoms depend on the degree of torsion and the acuteness of the volvulus onset.5 When onset is acute, it is a surgical emergency due to the risk of gastric ischemia and associated respiratory distress, with a mortality rate of up to 60%–80% in untreated cases. Currently, it seems that the morbidity and mortality of acute gastric volvulus has decreased to 20% as a consequence of the advances in its diagnosis and treatment.1
Gastric volvulus usually presents after the fifth or sixth decades of life, although there are more than 600 pediatric cases reported.16 There is a primary type, in which there is no underlying cause, and a secondary type, in which the most frequent predisposing etiologic factor is the presence of hiatal hernias,8 although it is also associated with traumatic, congenital diaphragmatic hernias, etc. Morphologically, volvuli are classified according to their major axis of rotation as either organo-axial (the most frequent), mesentero-axial or a mix of these 2 types.
The treatment of gastric volvulus is surgical and traditionally consists of the surgical correction of associated factors. The laparoscopic approach has been able to minimize surgical aggression of the procedure in these patients and results have been published of its use not only in the management of chronic gastric volvulus associated with hiatal hernia, but also in acute situations.1,3,9–12 Surgical correction is effective but not risk-free, even with laparoscopy: vagus injury, pneumothorax, hemorrhage recurrence of volvulus can occur.12,13
Given its low frequency, experience with laparoscopic surgical treatment in acute situations is limited. The primary objective is to avoid gastric ischemia. Thus, for its treatment a series of fundamental steps are defined: gastric decompression, derotation and correction of predisposing factors.
Initial decompression can be done by inserting an NGT, which occasionally also allows for partial derotation; nonetheless, its effectiveness is limited and there is risk of perforation during placement maneuvers.14 We have used NGT in 8 cases, since there is no on-call endoscopist at our Institution. We have observed no complications with the procedure, although we have seen a lack of effectiveness caused by either the inability to insert the NGT or volvulus relapse. Once in place, NGT allows us to decompress the stomach, maintain it partially rotated, or use the NGT as a tutor in order to avoid new episodes of volvulus while preparing the patient for deferred surgery.
If available, upper gastrointestinal (UGI) endoscopy15 is the ideal method for decompression and derotation. It provides the advantage of visualizing the state and viability of the gastric mucosa, and likewise verifies its recovery.
Some authors have advocated endoscopic derotation as the only treatment. However, even though it may be useful in very high risk patients and selected cases, it is not effective as a definitive treatment because re-volvulus is unpredictable and potentially catastrophic.16,17 Koger et al.10 use UGI endoscopy as support during the laparoscopic approach in emergency situations, which allows not only the evaluation of the state of the gastric mucosa, but also to appropriately position the stomach after fixation.
Although it was only available in two of our cases, we believe that UGI endoscopy is the ideal method for achieving derotation because it is done with direct vision. It provides effective gastric decompression that notably improves patients’ conditions. It is also able to convert an emergency situation into a situation where definitive treatment is deferrable while the patient's state is optimized. Nevertheless, we do not consider that its intraoperative use is necessary as a complement to the surgical intervention in all cases. If we are able to derotate the stomach and stabilize the patient, UGI endoscopy provides no additional benefit during definitive surgical correction. It may be useful in cases requiring emergency surgical intervention either because derotation is not achieved, or due to the patient's severe condition or suspicion of gastric ischemia.
The definitive treatment of volvulus involves correcting any associated predisposing factors. It has been demonstrated that surgical repair can be done laparoscopically, both in acute as well as chronic situations. Several authors1,5 defend the treatment of predisposing factors as the main mechanism for avoiding recurrence; they do agree, however, that in high-risk patients surgical treatment may be limited to gastropexy.
In our opinion, in patients with good general condition without serious associated comorbidities in whom we have been able to defer surgical intervention after initial gastric derotation and who present secondary volvulus, definitive treatment includes hernia reduction, resection of the hernial sac, closure of the esophageal hiatus with/without the use of prosthetic material and the creation of a short, loose total fundoplication. In these cases, we do not consider it necessary to perform gastric fixation with either gastropexy or temporary gastrostomy,6 as some authors do, and we have not observed cases of gastric volvulus at follow-up.
Certain points of hernia repair, such as sac removal, whether to use reinforcing materials and the association of anti-reflux mechanisms are currently the subject of controversy. As for the resection of the hernial sac, we continue to perform this procedure in the same way as in open surgery because, in addition to having the advantages of a direct view provided by laparoscopy, it allows us to determine exactly the anatomy of the hiatus; nevertheless, it is a procedure that has added morbidity, and some authors report no reduction in the relapse rate.18 We use prosthetic material for the closure of the hiatus in cases in which we observe closure with tension and/or tissue weakness, similar to Palanivelu et al.5 We used this material in the 3 patients because the hiatuses were very wide and weakened by the presence of large chronic hernias. Last of all, the association of an anti-reflux procedure (in our case a short, loose 360° fundoplication) is done systematically because we believe that the unstructured hiatus after reconstruction is not a sufficient valvular mechanism to avoid gastroesophageal reflux.
But most acute gastric volvuli generally present in patients with poor general conditions who require emergency surgical intervention and in the elderly with high surgical risk. These circumstances make it difficult to consider a standard surgical repair, as this would entail long surgical times and high morbidity, and we therefore opt for laparoscopic anterior gastropexy, without resecting the sac or correcting the hiatal defect. Fixation was done with simple sutures, although other authors have used total transparietal sutures19,20 or even the placement of a percutaneous endoscopic gastrostomy (PEG) associated with the gastropexy for a time or even definitively.21,22 We believe that PEG is an unnecessary and aggressive procedure that does not eliminate the possibility of volvulus, because volvulus around the PEG has been reported, as it can act as a torsion axis.23,24
Although our series is not extensive and the follow-up is short, laparoscopic anterior gastropexy as a single procedure seems to be a safe and effective treatment that resolves the emergency situation.1–5,25,26
In conclusion, we believe that the laparoscopic surgical approach has been demonstrated to be effective for treating both acute and chronic gastric volvulus, while providing the advantages of reduced morbidity offered by laparoscopy. In emergency situations, in patients with high surgical risk and in cases of primary volvulus, laparoscopic anterior gastropexy is sufficient, although studies of long-term results are needed.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Martínez García R, et al. Tratamiento del vólvulo gástrico agudo mediante abordaje laparoscópico. Cir Esp. 2013;91:189-93.