Wilkie's syndrome or superior mesenteric artery (SMA) syndrome was first described in 1842 by Rokitanski, although it was Wilkie who published the first series of 75 patients in 1927.1 It is a rare cause of upper intestinal obstruction caused by compression of the third part of the duodenum between the abdominal aorta and superior mesenteric artery at its origin. We present the case of a patient with this syndrome who had initially been treated conservatively but later required surgical treatment due to persisting symptoms.
The patient is a 29-year-old woman, with no medical or surgical history of interest, who, over the course of the previous 18 months, had presented postprandial fullness and abdominal distension, accompanied by nausea and occasional vomiting.
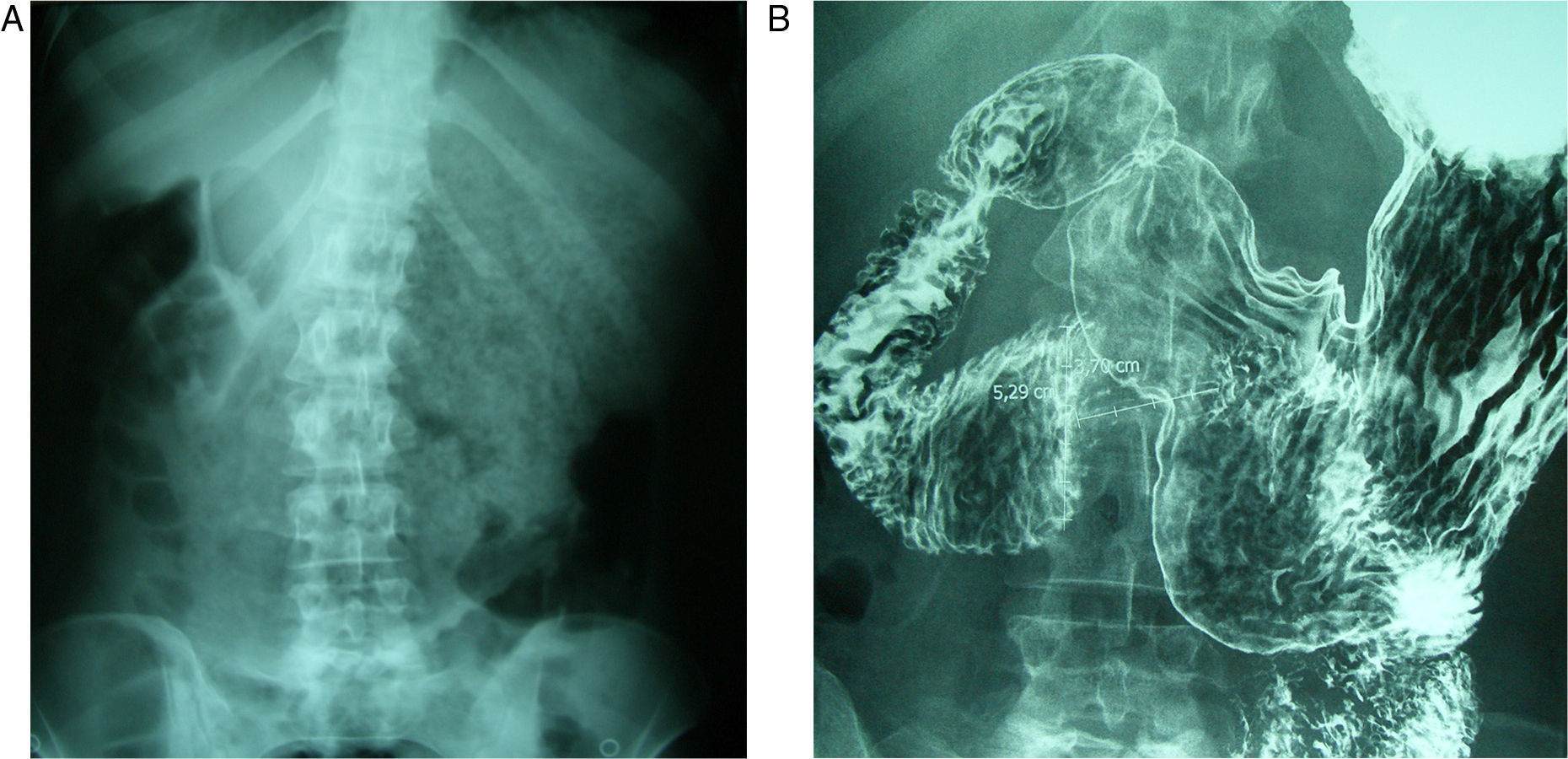
She came to the Emergency Department due to intolerance to oral intake, epigastric pain and bilious vomiting, which had begun abruptly. She was hemodynamically stable with mild signs of dehydration. Abdominal examination was normal, and the work-up showed normal blood tests. Simple radiography (Fig. 1A) revealed gastric dilatation. Conservative treatment was started with no oral intake, nasogastric suction and fluid therapy. An upper gastrointestinal (GI) series (Fig. 1B) showed that the esophagus, stomach and duodenal bulb had normal characteristics. There was, however, difficult emptying in the third part of the duodenum, which was consistent with functional disorder or SMA. On magnetic resonance imaging (MRI) study, the angle between the SMA and aorta was observed to be 17°.
The patient evolved favorably and a clinical follow-up was scheduled. During the following year, however, the symptoms reappeared with greater intensity. At this stage, surgical treatment was decided on after an upper GI series that confirmed the diagnosis.
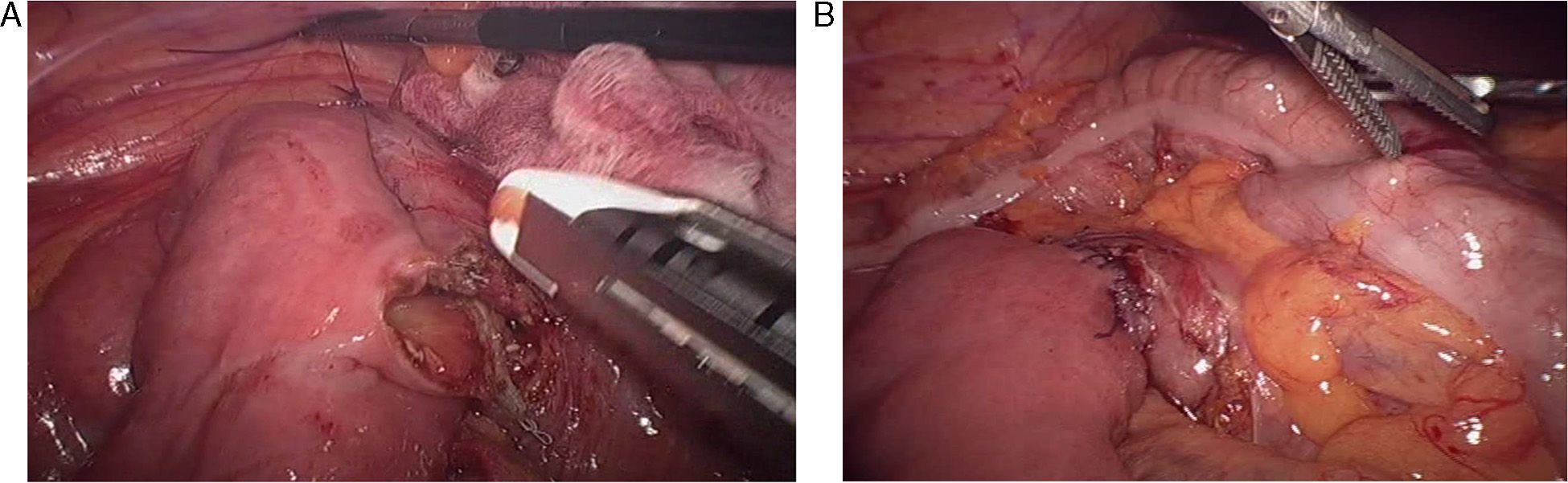
The patient was operated on laparoscopically using 4 trocars. The procedure included dissection of the duodenal c-loop with an infra-mesocolic approach and mechanical duodenojejunostomy between the second and third parts of the duodenum and the jejunum, about 25cm away from the angle of Treitz (Fig. 2A and B) with a 45mm linear endostapler using 2.5mm staples (white load). The postoperative period was uneventful, and the patient was discharged on the third day post-op with normal digestive tolerance.
Another upper GI series performed 3 months after the surgical intervention showed that the contrast passed from the normal-sized duodenum to the jejunal loops, with no images of stenosis. Two years after the operation, the patient remains asymptomatic.
The possible causes of SMA syndrome are debilitating disease (AIDS, cancer), eating disorders, postoperative effects (orthopedic surgeries and adhesiolysis due to obstruction of the small intestine), severe trauma and spinal column deformities. Recently, cases have been reported related to rapid weight loss after bariatric surgery.2
The incidence of SMA syndrome is 0.2%. It may occur at any age, but is most common in adolescents and young adults, especially women (2:1).3
Symptoms are nonspecific and may include postprandial epigastric pain, bloating, early satiety, nausea and vomiting. The pain is alleviated in the knee–chest position and in left lateral decubitus.4 The causes of death are due to severe electrolyte alterations, gastric perforation, obstructive bezoar or gastric or portal pneumatosis.3
Radiologic studies are essential. Historically, upper GI series and arteriography were the standard diagnostic tests, but more recently, CT angiography and MRI have shown greater sensitivity.
Classic upper GI study findings are dilatation of the first and second parts of the duodenum, antiperistaltic flow of the barium proximal to the obstruction, delayed gastrointestinal transit and relief of the obstruction with patient position changes.4
In angiographic studies, patients with SMA syndrome present an aortomesenteric angle of 7–22° (normal: 28–65°) and the distance between the aorta and the SMA is 2–8mm (normal: 10–34mm).
The treatment of SMA syndrome is generally conservative and is initially aimed at the correction of hydroelectrolytic and metabolic alterations, decompression of the gastrointestinal tract (including the use of posture maneuvers) or the placement of a nasogastric tube and recovery of the nutritional state. The use of prokinetics may be effective.2,4,5 As in the case of our patient, those with acute SMA syndrome almost always respond to conservative treatment; chronic symptoms, however, usually require surgical intervention after a period of refeeding.3
Surgical treatment is indicated when either medical treatment fails or the duodenal dilatation is persistent and progressive.2
The surgical techniques used are Strong's procedure, vascular re-implantation and gastrointestinal bypass.6 Strong's operation involves dissecting the ligament of Treitz and extensive mobilization of the duodenum in order to displace it from the aortomesenteric angle.
Transposition of the SMA at the infrarenal aorta is a standardized technique for the treatment of chronic ischemia that can be effective in SMA syndrome by thus avoiding disruption of the intestine.6,7
In patients with important gastric distension, gastrojejunostomy is a valid option, but it may cause bile reflux and anastomotic ulcer. Roux-en-Y and side-to-side duodenojejunostomy are the most frequently used surgical procedures, with a success rate of 90%. Nonetheless, they present a risk of intestinal stenosis and fistula.6 The laparoscopic approach, as described by Gersin and Heniford in 1998, provides definitive treatment by means of a minimally invasive technique, with its intrinsic advantages.7–9 Therefore, from our standpoint and in light of the case presented, it should currently be considered the treatment of choice.
Please cite this article as: Etxebarria Beitia E, Díez del Val I, Loureiro González C, González Serrano C, Bilbao Axpe JE. Duodenoyeyunostomía laparoscópica como tratamiento del síndrome de la arteria mesentérica superior. Cir Esp. 2014;92:129–131.