Leiomyosarcomas are aggressive tumors that can originate in any anatomical structure with the presence of smooth muscle cells. Those originating in vascular structures1 are uncommon (2% of all leiomyosarcomas). They have been reported mainly in the large central vessels, especially the inferior vena cava,2 and they are extremely rare in the peripheral veins of the extremities.3 Symptoms are non-specific and often suggestive of other more common disease, such as deep vein thrombosis.4–6 Treatment involves complete resection with safety margins as well as radiotherapy and/or chemotherapy, according to the stage. Prognosis is determined by location, size and degree of invasion of neighboring structures (due to the possibility to perform radical resection), along with the presence of metastatic dissemination at the time of diagnosis.7 The need for vascular reconstruction, frequently conducted in tumors located in the inferior vena cava, is optional and questioned in the case of peripheral vein involvement because of the capacity for compensation by collateral circulation.3,8
We present the case of a 65-year-old male patient with a prior medical history of arterial hypertension, dyslipidemia, smoking and esophagitis, who came to the emergency room with edema of the left lower extremity that had been progressing over the course of several weeks. Emergency echo-Doppler detected absence of collapsibility in the femoral region. Anticoagulant therapy with low-molecular weight heparin was then initiated due to the suspicion of deep vein thrombosis, and the patient was sent to the vascular surgery outpatient consultation.
At this time, the Doppler study was repeated, which determined that the absence of collapsibility was caused by an intravascular nodular image in the left common femoral vein, which was hypoechoic, solid, homogeneous, well-outlined and caused an approximate reduction of 90% in the lumen and measured approximately 1×0.4cm.
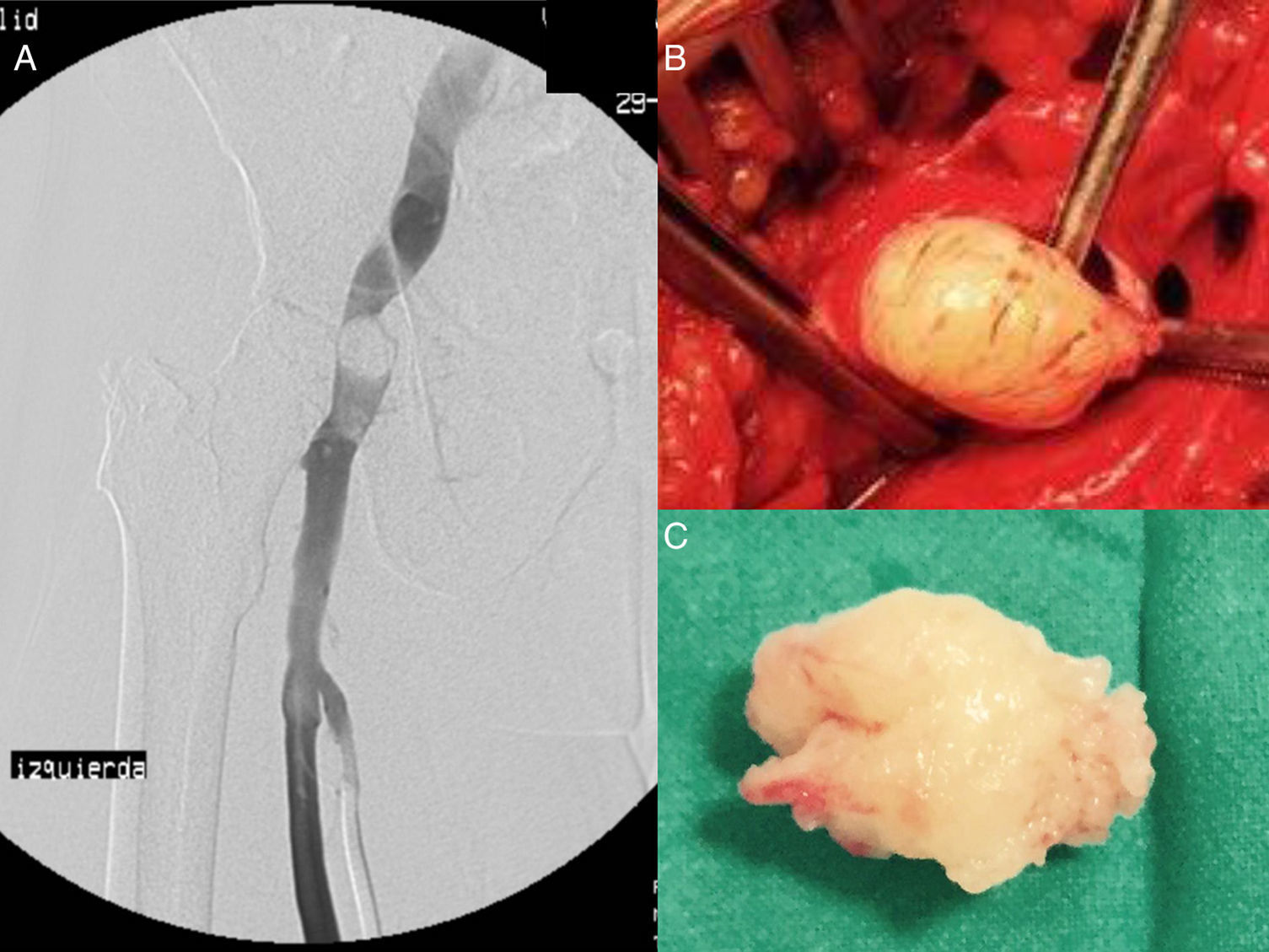
Ascending phlebography of the left lower extremity showed the existence of the filling defect in the left common femoral vein due to a well-outlined mass, which resulted in decreased vessel size and passage of peripheral contrast (Fig. 1A). Given these findings and the characteristics described on ultrasound, the initial diagnostic possibility proposed was the existence of a benign mass.
We decided to conduct a surgical biopsy of the lesion. Under neuraxial anesthesia, we performed a longitudinal left inguinal incision, dissection of the common femoral vein and longitudinal venotomy. A whitish pedunculated mass was observed on the posterior side of the vein, which was well-outlined, measuring 2cm in length and occupying the entire lumen of the vessel. The mass was resected and the venotomy closed with a saphenous vein patch (Fig. 1B).
The pathology study was compatible with leiomyosarcoma: “Macroscopy: partially resected tissue mass, whitish in color and elastic-firm consistency, irregular ovoid shape, with a maximum diameter of 2.5cm” (Fig. 1C). “Microscopy: malignant mesenchymal neoplasm comprised of fascicules of elongated cells with smooth muscle characteristics, mostly well or moderately differentiated, although with areas of abundant large lobulated hyperchromatic nuclei. Mitotic rate: ±3 mitoses per 10HPF, with presence of atypical mitoses. Small foci of initial tumor necrosis are observed. Neoplastic cells present expression of actin, muscle actin and desmin. The tumor is in contact with the biopsy margins.”
The patient was evaluated by the oncology department, and an extension study was requested with magnetic resonance imaging (MRI) of the pelvis and computed tomography (CT) of the thorax, abdomen and pelvis; both tests were normal.
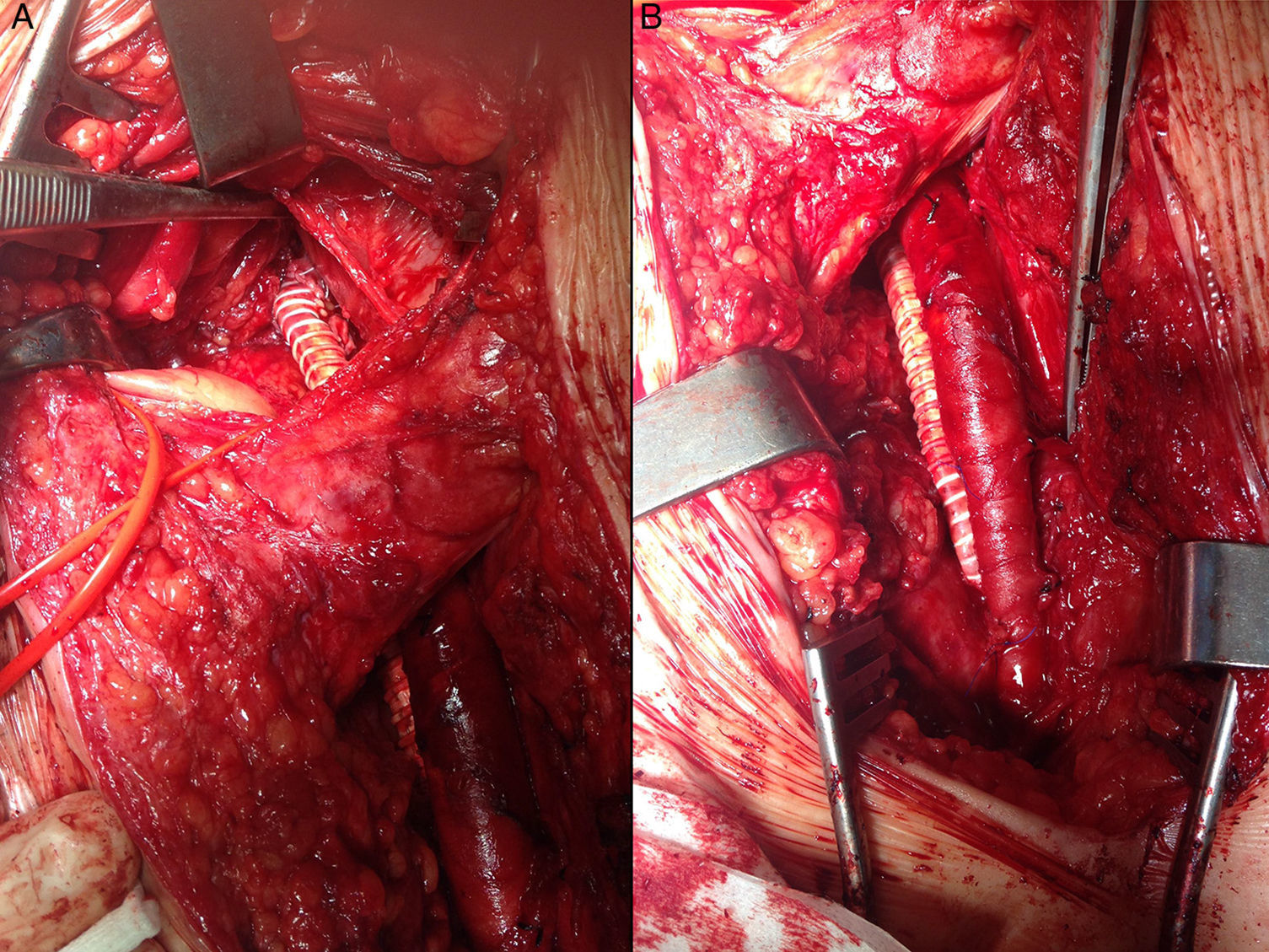
It was decided to perform surgery to extend the surgical margins. A left inguinal longitudinal incision was made with oblique cranial extension in the left iliac fossa and retroperitoneal access, and dissection and control of the external iliac vein, common femoral vein, femoral vein and deep femoral vein. Resection was conducted of the common femoral vein and distal third of the external iliac vein, together with vascular reconstruction using a ringed PTFE graft with end-to-end anastomosis between the external iliac vein and the femoral vein (Fig. 2).
The pathology study of the specimen reported: “Macroscopy: venous segment measuring 6.5cm long, which presented a maximum diameter of 3cm and a thickened area that appeared to be perivascular scarring with an approximate diameter of 5cm. Microscopy: venous segment and adjacent soft tissue with scar-type fibrosis, with no evidence of persisting neoplasm in the margins.”
With the diagnosis of intravascular leiomyosarcoma in the common femoral vein, stage pT1a pN0 cM0 R1, we decided not to administer adjuvant oncologic treatment. Six months after the intervention, the patient continues to be asymptomatic, except for mild residual edema of the extremity, and radiological studies have shown no local recurrence (MRI) or distant dissemination (thoracoabdominal CT).
Please cite this article as: Brizuela Sanz JA, Estévez Fernández I, Fuente Garrido R, Gutiérrez Castillo D, Vaquero Puerta C. Leiomiosarcoma intraluminal de vena femoral común. Cir Esp. 2016;94:611–613.