To evaluate the results of our program of clipping the thoracic sympathetic nervous system (TSNS) for the treatment of facial flush and/or hyperhidrosis (HH), and to compare the methodology-results of the program development phase (A: January 2007–April 2009) and its consolidation phase (B: May 2009–March 2010).
Material and methodsThe program included a total of 44 patients (88 procedures) subjected to video thoracoscopy and clipping of the TSNS in a one day surgery unit. Data were collected and analyzed retrospectively, and a descriptive and comparative statistical analysis was performed between the two periods (A and B).
ResultsThe overall morbidity was 5 cases (11.3%). The post-surgical occurrence rate of HH was 4.54% (2 cases), and the incidence of compensatory sweating was 65.9% (minimal in 26 of the 29 cases). On comparing period B with period A, there was a significant decrease in surgical time, disappearance of recurrence of HH, a decrease of 30% in morbidity, reduction by half in the incidence of moderate to severe compensatory sweating, and an increase in the level of satisfaction. The clamps were removed in one of the poorly tolerated compensatory sweating cases, resulting in its disappearance.
ConclusionsClipping the TSNS is a safe technique in the one day surgery unit, with a short learning curve (20 cases) after which comparable, or even better, results are obtained than those of sympatholysis. These results, together with their potential reversibility, make it, in our opinion, the technique of choice in the surgery of the TSNS.
Evaluar los resultados de nuestro programa de clipaje del sistema nervioso torácico simpático (SNTS) para el tratamiento del rubor facial y/o hiperhidrosis (HH) y comparar la metodología-resultados de la fase de desarrollo del programa (A: enero 2007-abril 2009) y la fase de consolidación del mismo (B: mayo 2009-marzo 2010).
Población y métodosSe ha incluido a 44 pacientes (88 procedimientos) sometidos a clipaje videotoracoscópico del SNTS en régimen de cirugía mayor ambulatoria (CMA). Los datos fueron recogidos prospectivamente y analizados retrospectivamente. Se ha realizado estudio estadístico descriptivo y comparativo entre los 2 grupos.
ResultadosLa morbilidad global fue de 5 casos (11,3%). La tasa de recidiva postquirúrgica de HH fue del 4,54% (2 casos), la incidencia de sudoración compensadora (SC) fue del 65,9% (mínima en 26 de los 29 casos). Al comparar el período B con el A, se aprecia: disminución significativa del tiempo quirúrgico, desaparición de la recidiva de HH, disminución de la morbilidad en un 30%, reducción a la mitad de la incidencia de SC moderada-severa e incremento del grado de satisfacción. En uno de los casos de SC mal tolerada se retiraron los clips consiguiéndose la desaparición de esta.
ConclusionesEl clipaje del SNTS es una técnica segura en régimen de CMA, con una curva de aprendizaje corta (20 casos) tras la cual se obtienen resultados equiparables o, incluso mejores, que los de la simpaticolisis. Estos resultados, junto a su potencial reversibilidad, la convierten, en nuestra opinión, en la técnica de elección en la cirugía del SNTS.
Primary hyperhidrosis (PH) is a disease of unknown etiology characterized by excessive production of eccrine sweat that can cause severe alterations in patients’ social and professional lives. In many cases, there is a vicious circle of sweating–anxiety–greater sweating that limits the patient's self-esteem and makes it difficult to live a normal life.1
Currently, endoscopic surgery on the thoracic sympathetic nervous system (TSNS) has become an effective option for the treatment of hyperhidrosis and/or facial flushing (FF).2–4 In most cases, this surgery entails sectioning the thoracic sympathetic nerve at one or more levels (sympathicolysis) or, less frequently, the exeresis of one or more ganglia of the thoracic sympathetic nerve chain (sympathectomy), to resolve PH.
One of the most worrisome side effects of these surgical treatments for hyperhidrosis is the appearance of compensatory hyperhidrosis (CH), which is sweating that appears in different anatomical areas than the PH (generally back, gluteus and/or thighs) after surgery of the TSNS. Its incidence varies depending on the series (from 14% to 90% of patients); it is mild in up to 90% of cases and severe in 1%–30% of patients who undergo surgery.5 There is currently no consensus about what factors condition the appearance of CH,6 but there is growing scientific evidence demonstrating that the higher the level of the TSNS interruption, the higher the incidence of CS; this is especially true if clipping is at the level of or above the second thoracic sympathetic ganglion.5,7–9
Neurophysiology studies by Denny-Brown et al.10 demonstrated that nerve conduction could be suppressed by exerting continuous pressure ≥44g for 2 weeks on the nerve with spring clips. Based on these results, in 1998, Lin et al.11 demonstrated the efficacy of the technique for treating palmar PH and defended the reversibility of the procedure in cases of intolerable CS by removing the clips. The physiological mechanism of this reversibility is not well understood4; and the maximum time that the TSNS can be clipped while still being able to recover nerve conduction after unclipping has not been clearly established. Nonetheless, there is growing evidence that clip removal in cases of intolerable CS leads to either total or partial remission in 50%–80% of cases9,12,13 which, furthermore, may not be accompanied by reappearance of PH in nearly 50% of unclipped patients.4
In our TSNS major ambulatory surgery (MAS) program, we introduced the clipping technique in January 2007. Since then, TSNS clipping has been used as an alternative to sympathectomy/sympathicolysis according to preferences of the patient or surgeon.
This study evaluates the results of our program and compares the methodology and results of the developmental phase of the program (period A: January 2007–April 2009) and consolidation phase (period B: May 2009–March 2010).
Patients and MethodsFrom January 2007 to March 2010, 99 patients (198 procedures) were treated in the MAS program. All patients gave their informed consent (IC) for the intervention and the use of the data for research purposes.
Out of a total of 99 patients, 44 cases (88 procedures) were included in the study. The cases have been divided into two study periods: period A, January 2007–April 2009 (22 cases); and period B, May 2009–March 2010 (22 cases).
All patients underwent preoperative evaluation that included detailed anamnesis and physical examination, chest X-ray, general blood tests, and thyroid function tests in cases with suspicion for thyroid disease.
Surgical TechniqueAll patients underwent video-assisted thoracoscopic surgery under general anesthesia with sequential selective ventilation in a semi-Fowler position. In all cases, a continuous temperature sensor was placed on the index finger in order to monitor the effectiveness of the procedure during surgery (correct TSNS clipping if increased ≥0.5°C). The surgical protocol included 2 ports in the hemithorax: one measuring 5mm diameter in the 3rd intercostal space on the midaxillary line in order to insert a thoracoscope (Karl Storz® optic, 5mm 0°); and another working port measuring 12mm in diameter in the 5th intercostal space on the anterior axillary line to order to insert the instruments, including ultrasonic scalpel (Ultracision®, Ethicon Endosurgery, Cincinnati, OH, USA) or electrocoagulation (monopolar diathermy) and later insertion of the right-angle clip applier with 20 8-mm titanium clips (Acuclip™, Covidien®). The procedure continued with skeletonization of the sympathetic chain at the selected level using ultrasonic or electric scalpel (in cases of FF/craniofacial PH, always with ultrasonic scalpel) and avoiding thermal damage to the TSNS fibers. Finally, the thoracic sympathetic nerve chain was clipped, taking care to avoid any traction that could cause avulsion or ganglion damage.
With regard to the clipping level, our technique has varied over time in accordance with published scientific evidence.9,12,14 Thus, at the start of the program, for craniofacial PH/flushing we clipped at the cranial edge of the second rib (R2); for axillary PH, we isolated T3 (R3–R4) and for palmar PH T2–T3 (R2–R3–R4). We have progressively changed to isolating T3 (R3–R4) for palmar PH and isolating T4 (R4–R5) for axillary PH, maintaining R2 clipped in cases of FF/craniofacial PH. In all cases, we cut any possible communicating nerve branches by lateral extension of the coagulation at the corresponding ribs. In the contralateral hemithorax, the same procedure was repeated.
Immediate Post-op and Follow-upAfter being extubated in the operating room, the patients were transferred to the MAS recovery room and analgesia was administered in gradually decreasing dosages (initially, intravenous NSAID±morphine, then oral NSAID and morphine at discharge). Once proper oral tolerance was confirmed, pain was controlled with oral analgesia and X-rays showed no alterations, the patients were discharged.
Follow-up was by phone after 24h, then in the outpatient clinic at 2 weeks, then at 4, 12 and 24 months
Data Collection and Statistical AnalysisAll the data were collected with a questionnaire that was specifically designed to study the surgical treatment of TSNS, recorded prospectively and analyzed retrospectively.
In the descriptive statistical study, the quantitative variables have been expressed by means of measures of central tendency (mean±SD for data with symmetrical distribution, or median+interquartile range [IRI] for asymmetrical data). The qualitative variables were expressed with frequency tables and valid percentages. The analysis of quantitative variables was performed using Student's t-test or the Mann–Whitney test. For the qualitative variables, we used the chi-squared (χ2) or Fisher's exact test. A P value ≤.05 was considered significant.
The SPSS v. 15 statistical package (SPSS Inc., Chicago, IL, USA) was used.
ResultsMean age was 29 (±9.5), with a predominance of women (72.7% of cases). Most patients were Spaniards (77.3% of cases), followed by Latin Americans (18.2% of cases). 61.4% of our patients had been referred by their family physician, while 31.8% had been referred by dermatologists. Before the first office visit in our Department, 27 patients (61.4%) had previously used topical treatment, 2 patients (4.6%) iontophoresis, another 2 (4.6%) psycho-pharmacological treatment and the remainder had not received any prior treatment. Among those who had been treated previously, the effectiveness of the treatments was non-existent in 83.9% of the cases and dose-dependent in the rest.
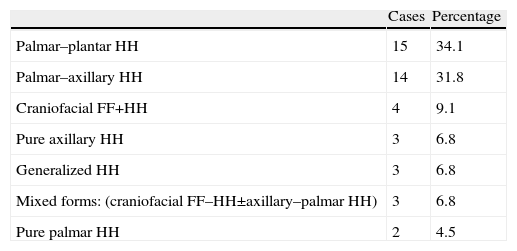
The indications for surgery are summarized in Table 1. All the patients underwent bilateral interventions. There were no severe intraoperative complications, re-operations during the immediate post-op period or mortality in the series. Total morbidity of the series was 5 cases (11.3%): 3 cases of poorly controlled pain and 2 cases of post-surgical pneumothorax that required insertion of a chest drain. The overall percentage of patients who underwent surgery in the MAS program was 90.9%, and 4 patients required hospitalization due to minor post-surgical complications. The rate of post-surgical relapse of HH was 4.54% (2 cases); in both cases, the patients were re-operated on (sympathetic chain cut at clip levels) on the left side in one patient and bilaterally in the other. In both cases, post-surgery anhidrosis was achieved. In the series, the incidence of CH was 65.9% (29 cases), of which 26 cases presented minimal CH, while 2 cases presented moderate and one severe CH.
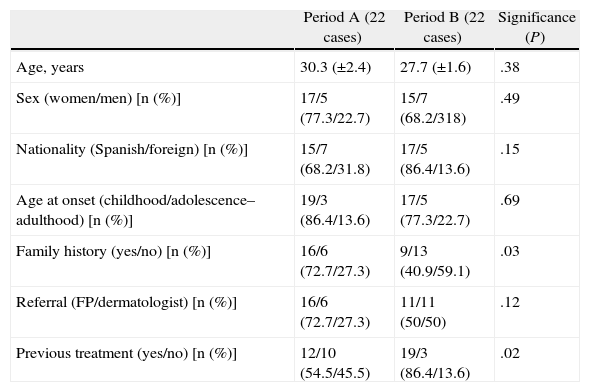
Table 2 summarizes and compares the clinical and demographic characteristics of the 2 study groups.
Clinical and Demographic Characteristics of the 2 Study Groups.
| Period A (22 cases) | Period B (22 cases) | Significance (P) | |
| Age, years | 30.3 (±2.4) | 27.7 (±1.6) | .38 |
| Sex (women/men) [n (%)] | 17/5 (77.3/22.7) | 15/7 (68.2/318) | .49 |
| Nationality (Spanish/foreign) [n (%)] | 15/7 (68.2/31.8) | 17/5 (86.4/13.6) | .15 |
| Age at onset (childhood/adolescence–adulthood) [n (%)] | 19/3 (86.4/13.6) | 17/5 (77.3/22.7) | .69 |
| Family history (yes/no) [n (%)] | 16/6 (72.7/27.3) | 9/13 (40.9/59.1) | .03 |
| Referral (FP/dermatologist) [n (%)] | 16/6 (72.7/27.3) | 11/11 (50/50) | .12 |
| Previous treatment (yes/no) [n (%)] | 12/10 (54.5/45.5) | 19/3 (86.4/13.6) | .02 |
FP: family physician.
Data expressed as mean±standard deviation or number of cases and percentage.
Statistics used: Student's t-test for unpaired data, chi-squared or Fisher's exact test as necessary. A P value ≤.05 was considered significant.
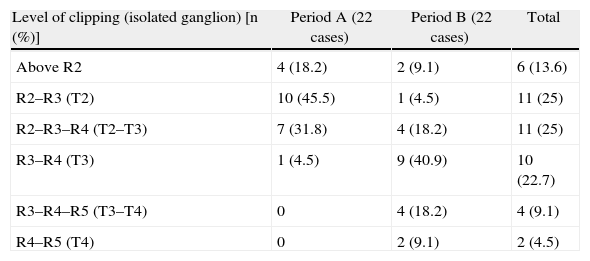
Table 3 shows the clipping level of the sympathetic chain in our series and how it has been modified during the intervention period.
Level of Clipping of the Thoracic Sympathetic Chain.
| Level of clipping (isolated ganglion) [n (%)] | Period A (22 cases) | Period B (22 cases) | Total |
| Above R2 | 4 (18.2) | 2 (9.1) | 6 (13.6) |
| R2–R3 (T2) | 10 (45.5) | 1 (4.5) | 11 (25) |
| R2–R3–R4 (T2–T3) | 7 (31.8) | 4 (18.2) | 11 (25) |
| R3–R4 (T3) | 1 (4.5) | 9 (40.9) | 10 (22.7) |
| R3–R4–R5 (T3–T4) | 0 | 4 (18.2) | 4 (9.1) |
| R4–R5 (T4) | 0 | 2 (9.1) | 2 (4.5) |
R: rib.
Percentage of the entire study period (column).
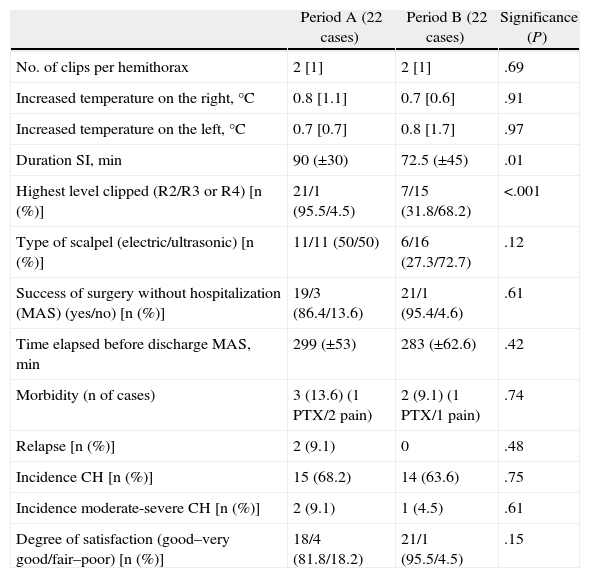
Table 4 compares the surgical technique in each intervention period and the differences obtained in the results.
Surgical Technique and Results According to the Intervention Period.
| Period A (22 cases) | Period B (22 cases) | Significance (P) | |
| No. of clips per hemithorax | 2 [1] | 2 [1] | .69 |
| Increased temperature on the right, °C | 0.8 [1.1] | 0.7 [0.6] | .91 |
| Increased temperature on the left, °C | 0.7 [0.7] | 0.8 [1.7] | .97 |
| Duration SI, min | 90 (±30) | 72.5 (±45) | .01 |
| Highest level clipped (R2/R3 or R4) [n (%)] | 21/1 (95.5/4.5) | 7/15 (31.8/68.2) | <.001 |
| Type of scalpel (electric/ultrasonic) [n (%)] | 11/11 (50/50) | 6/16 (27.3/72.7) | .12 |
| Success of surgery without hospitalization (MAS) (yes/no) [n (%)] | 19/3 (86.4/13.6) | 21/1 (95.4/4.6) | .61 |
| Time elapsed before discharge MAS, min | 299 (±53) | 283 (±62.6) | .42 |
| Morbidity (n of cases) | 3 (13.6) (1 PTX/2 pain) | 2 (9.1) (1 PTX/1 pain) | .74 |
| Relapse [n (%)] | 2 (9.1) | 0 | .48 |
| Incidence CH [n (%)] | 15 (68.2) | 14 (63.6) | .75 |
| Incidence moderate-severe CH [n (%)] | 2 (9.1) | 1 (4.5) | .61 |
| Degree of satisfaction (good–very good/fair–poor) [n (%)] | 18/4 (81.8/18.2) | 21/1 (95.5/4.5) | .15 |
CH: compensatory hyperhidrosis; SI: surgical intervention; PTX: pneumothorax.
Data are expressed as means (±standard deviation), median (interquartile range) or number of cases and percentages. Statistical analyses used: Student's t or Mann–Whitney. For qualitative variables: chi-squared (χ2) or Fisher's exact test. A P value ≤.05 was considered significant.
As for the appearance of compensatory hyperhidrosis, the 3 cases of moderate-severe CH were from the group of patients in whom the TSNS had been interrupted at the R2 level (associated or not with interruption at other levels), and no cases of moderate-severe CH were seen in the group of patients with clipping at level R3 or lower. This difference, although clinically relevant, is not statistically significant (Fisher's exact test, P=.28). In one of the 3 cases of moderate-severe CH, the clips were removed 4 months after the operation, achieving reversibility 4 months after the 2nd operation.
DiscussionEndoscopic surgery on the TSNS is currently the treatment of choice in patients with HH and/or FF that are refractory to medical treatment.2–4 Since the publication of the papers by Lin et al.,11 sympathicolysis coexists with the clipping technique, which has been demonstrated to be a safe technique that provides comparable results,15,16 with the advantage of being potentially reversible in up to 80% of cases when the clips are removed.4,11,17
This paper demonstrates that a TSNS clipping program can be implemented in our setting with no mortality and acceptable morbidity, although somewhat higher than reported in the international literature.4,16 This was especially true in the initial stage of the program, which highlights the learning curve, in spite of which there have been no complications requiring conversion to open surgery (in some series, this is reported in up to 2.8%)18 or any appearance of major complications such as chylothorax,18 damage to major vascular structures,17,19,20 brachial plexus,20 or Horner's syndrome (with a reported incidence of between 0 and 5.2%, in different series).18,21 Different risk factors for these complications have been described, including the diffusion of the electric current from the monopolar scalpel,21 excessive traction of the TSNS20 or an erroneous localization of the second rib. In this study, we demonstrate that, even in the initial phases of the TSNS clip implantation, the traction exerted on the TSNS for clipping is not a risk factor for the appearance of Horner's syndrome if done cautiously and after correct dissection of the TSNS.
As in other previous studies,4,16 in our series we have observed that TSNS clipping is associated with a low recurrence rate (4.5%) but our data suggest that these cases might be related with the learning curve because in the consolidation phase of our program there were no recurrences. These data are comparable to the results obtained with sympathicolysis.5 Despite there being no significant differences between the incidence of cranial, palmar or axillary HH or its combinations between the two study periods (data not shown) and following the related scientific evidence published,7,9,10 we have modified our surgical technique by progressively lowering the level at which the TSNS is clipped. This is shown in the fact that in 95.5% of patients of the initial period, the clip was placed more cranially at the level of the 2nd rib, while this percentage decreased significantly in the consolidation period in which the 2nd rib was only clipped in 31.8% of cases. As was expected according to the review by Weksler et al.7 or the study by Yanguo Liu et al.,22 this change meant a decrease (although not statistically significant) in the incidence of total CH with disappearance of moderate-severe CS in the consolidation group. These differences, although they do not reach statistical significance, are quite probably the reason why the degree of satisfaction among patients operated on in the second period is greater, although we want to comment that the satisfaction rate throughout the series is high and comparable to other published series.11,17
As for the reversibility of clipping, the topic has been widely discussed in the literature and in this study we can only mention that it is a simple technique, even for groups without prior experience, like ours. Unfortunately, as we only had one case with clip removal, we cannot provide any type of consistent scientific evidence. Finally, we would like to comment that the limited number of patients included in this study and the technical variations that have been developed throughout the study period could be a limitation for some of the results obtained; but, we believe that the main objective of this study, which was demonstrating the feasibility of successfully establishing a TSNS clipping program in our setting, is not compromised by these possible limitations.
In conclusion, TSNS clipping is a safe technique with good results, low morbidity and no mortality even in the initial phases of its implementation. There is an evident learning curve, after which the results are equal to or even higher than those obtained with other surgical techniques. All these factors, together with the potential reversibility of the technique, make TSNS clipping the technique of choice in TSNS surgery for treating primary hyperhidrosis and/or facial flushing.
Conflict of InterestsThe authors declare no conflict of interests.
Please cite this article as: Martinez-Barenys Carlos, et al. Experiencia inicial de un programa de clipaje del sistema nervioso simpático para el tratamiento de la hiperhidrosis y el rubor facial. Cir Esp. 2013;91:115–120.