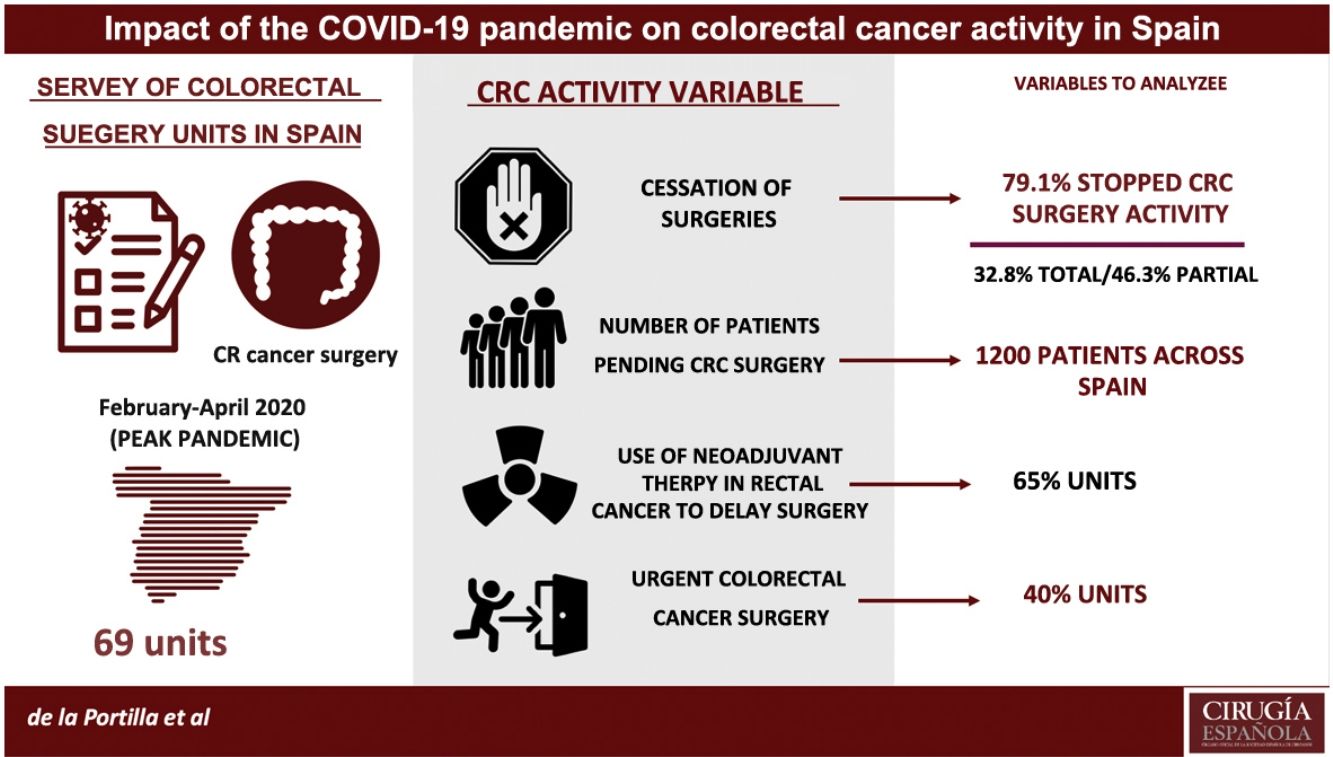
The pandemic has had an impact on colorectal cancer surgery in hospitals. In 2020, up to 75% of colorectal cancer patients are estimated to require surgery. No objective data on the impact of the pandemic on the management of surgical waiting lists is available. We conducted a survey in colorectal surgery units to assess the impact on colorectal cancer surgery waiting lists.
MethodAll personnel in charge of colorectal surgery units nationwide received a survey (from February to April, 2020) with eight questions divided into three sections—cessation date of colorectal cancer surgeries, number of patients waiting for treatment, and use of neoadjuvant therapy to postpone surgery.
ResultsSixty-seven units participated in the study, with 79.1% of units ceasing some type of activity (32.8% total and 46.3% partial cessation) and 20.9% continuing all surgical activity. In addition, 65% of units used or prolonged neoadjuvant therapy in rectal cancer patients and 40% of units performed at least five emergency colorectal cancer surgeries. It was estimated that at least one month of intense surgical activity will be required to catch up.
ConclusionsCurrently, patients from units with a long waiting list must be redistributed, at least within the country. In the future, in the event of a second wave of the pandemic, an effective program to manage each unit’s resources should be developed to prevent total collapse.
La pandemia ocasionada ha supuesto un impacto sobre la actividad quirúrgica en nuestros hospitales, afectando entre otros al cáncer colorrectal. Para el año 2020 se ha estimado que hasta un 75% de pacientes diagnosticados de cáncer colorrectal precisaría cirugía. No se disponen de datos objetivos del impacto que la pandemia ha tenido sobre la gestión de las listas de espera quirúrgicas. Hemos realizado una encuesta a todas las unidades de cirugía colorrectal con el objetivo de conocer el impacto sobre las listas de espera quirúrgicas por cáncer colorrectal.
MétodoLos responsables de las unidades de cirugía colorrectal a nivel nacional recibieron una encuesta (febrero-abril, 2020) con 8 preguntas divididas en 3 apartados: cese y fecha de parada de las cirugías por cáncer colorrectal, número de pacientes pendientes de tratamiento y uso de neoadyuvancia como recurso de demora.
ResultadosSesenta y siete unidades participaron (todas las comunidades representadas). El 79,1% realizaron algún tipo de cese de actividad (total 32,8%, parcial 46,3%) y no cese el 20,9%. El 65% ha usado o prolongado la neoadyuvancia en pacientes con cáncer rectal. El 40% ha intervenido, al menos, a 5 pacientes de urgencia por cáncer colorrectal. Se ha estimado que al menos se precisará de un mes de cirugía intensa para ponerse al día.
ConclusionesEn el momento actual es preciso redistribuir pacientes de unidades con alta lista de espera. Para el futuro, en caso de repandemia, habría que planificar los recursos de las unidades para obtener un programa efectivo antes del periodo de colapso completo.
There is no doubt that the current pandemic caused by the SARS-CoV-2 virus has had an unprecedented impact on surgical activity in our hospitals and has exceeded all expectations nationally.
At the time of this writing (day 50 of confinement), more than 217 000 cases have already been diagnosed in Spain, with a total of 25 264 deaths. However, the scourge of the pandemic has not affected the entire country equally, and certain regions, such as Madrid and Catalonia, have been more affected.
The declaration of the national ‘state of alarm’ on March 15, 2020 led to the imposition of a national quarantine as well as the establishment of extraordinary healthcare measures. This situation and the consumption of healthcare resources have also caused a significant reduction in the activity of colorectal surgery units, whose surgical activity has been canceled or greatly reduced, both in benign and malignant conditions.
In 2020 in Spain, the Spanish Society of Medical Oncology (SEOM) estimated that 30 000 new cases of colon cancer and about 14 000 new cases of rectal cancer would be diagnosed.1 Of these, it is known that up to 75% will present a disease initially treatable by surgery. Although it is difficult to calculate precisely, in a period of about 60 days of total or partial cessation of activity, at least 1200 patients would not be treated surgically,2if we take into account both secondary and tertiary hospitals.
Under normal conditions, we know that the survival of these patients does not vary if the surgery is delayed 2–3 months.3 However, it has been suggested that this period of limited healthcare resources (human, material and logistical) may have an impact on the survival of these patients, regardless of the effect of the virus and its complications.4,5
Currently, there are no objective data available on the impact that the pandemic has had on the management of surgical waiting lists for colorectal cancer.6 We believe that this is important to determine in order to predict the healthcare pressure that the healthcare system will have to endure after the curve of the pandemic flattens. In addition, it would be interesting to analyze how it has affected the national territory and analyze those areas in which it has been possible to care for patients with colorectal cancer.
Hence, we decided to conduct a nationwide survey in colorectal surgery units, in order to know the impact of the pandemic on the management of patients diagnosed immediately before and during the pandemic, who required elective surgical treatment.
MethodsThe directors of each national colorectal surgery unit received a survey consisting of 8 questions divided into 3 main sections referring to the cessation and stop date of colorectal cancer surgeries, the number of patients pending treatment, and the use of neoadjuvant therapy as a resource for delaying surgical procedures (Table 1).
Multiple-choice questions of the AECP survey.
| Questions | Options |
|---|---|
| 1. Needed to stop surgical activity | No |
| Yes, partially | |
| Yes, totally | |
| 2. If so, date of cessation of activity | Date |
| 3. Number of rectal cancer patients awaiting surgery | None |
| 1–10 | |
| 11–20 | |
| >20 | |
| 4. Number of colon cancer patients awaiting surgery | None |
| 1–5 | |
| 6–10 | |
| 11–15 | |
| 16–20 | |
| >20 | |
| 5. Number of rectal cancer patients treated in this period | None |
| 1–10 | |
| 11–20 | |
| >20 | |
| 6. Number of colon cancer patients treated in this period | None |
| 1–5 | |
| 6–10 | |
| 11–15 | |
| 16–20 | |
| >20 | |
| 7. Number of rectal cancer patients in whom neoadjuvant therapy was indicated in order to delay surgery | None |
| 0–10 | |
| 11–20 | |
| 8. Number of colorectal surgery patients treated with urgent surgery | None |
| 0–5 | |
| 6–10 | |
| 11–15 | |
| 16–20 | |
| >20 |
All data requested refer to the pandemic period (from the end of February to mid-April), before the de-escalation. All questions were created in order to receive direct and unambiguous information on the state of each unit.
When incongruous data were detected, the head surgeon was contacted to review them. The Spanish Association of Coloproctology assisted with the dissemination of the survey.
This is a descriptive cross-sectional study of the situation of the coloproctology units in Spain during the SARS-CoV2 pandemic that uses a survey as a measurement tool. The design is a Likert-type survey composed of 8 questions with multiple-choice answers.
Statistical analysisThe ordinal or nominal categorical variables were described by the number of cases in each category, including the number of missing data, and calculating the percentage of the total. All analyses were performed using SPSS statistical software, version 20 for Mac.
ResultsData for a total of 67 colorectal surgery units were collected by the survey, representing all ‘autonomous communities’ of Spain (except Cantabria) and 31 participating provinces (Fig. 1).
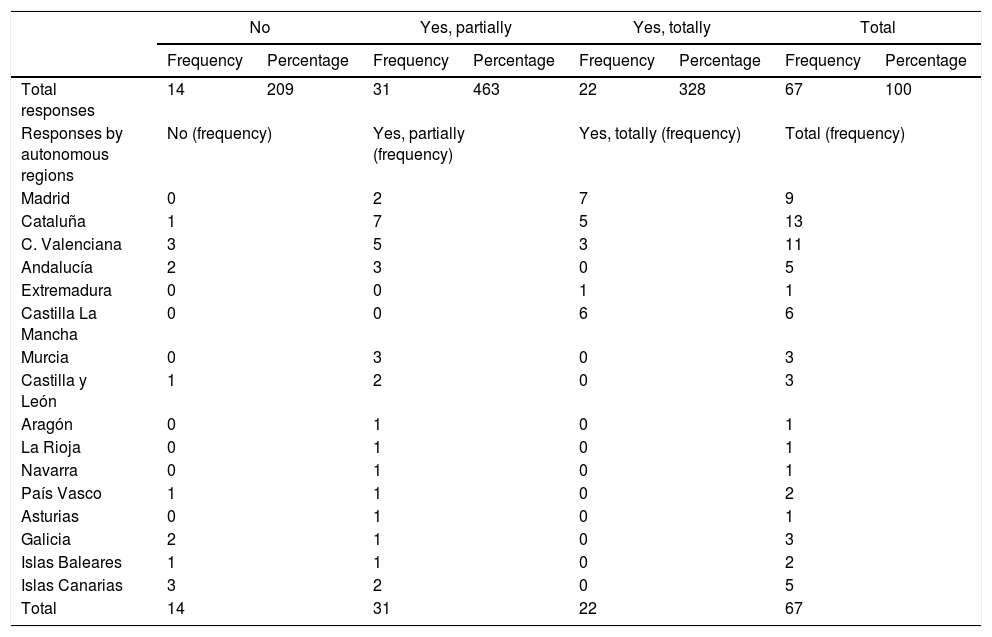
Regarding the cessation of surgical activity in the pandemic, 79.1% (53/67) of the participating units stopped their surgical activity in one way or another, with total cessation of activity at 32.8% (22/67) of the hospitals, 46.3% (31/67) partial, and only 20.9% (14/67) of the hospitals did not stop their activity.
In the regions of Castilla-La Mancha and Madrid (central area), as well as in Valencia and Catalonia (eastern area), the cessation of activity was complete, coinciding with the total collapse of their hospitals. In hospitals in the north and south of Spain, the cessation of surgical activity for colorectal cancer was lower (Table 2).
Need to stop surgical activity.
| No | Yes, partially | Yes, totally | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |
| Total responses | 14 | 209 | 31 | 463 | 22 | 328 | 67 | 100 |
| Responses by autonomous regions | No (frequency) | Yes, partially (frequency) | Yes, totally (frequency) | Total (frequency) | ||||
| Madrid | 0 | 2 | 7 | 9 | ||||
| Cataluña | 1 | 7 | 5 | 13 | ||||
| C. Valenciana | 3 | 5 | 3 | 11 | ||||
| Andalucía | 2 | 3 | 0 | 5 | ||||
| Extremadura | 0 | 0 | 1 | 1 | ||||
| Castilla La Mancha | 0 | 0 | 6 | 6 | ||||
| Murcia | 0 | 3 | 0 | 3 | ||||
| Castilla y León | 1 | 2 | 0 | 3 | ||||
| Aragón | 0 | 1 | 0 | 1 | ||||
| La Rioja | 0 | 1 | 0 | 1 | ||||
| Navarra | 0 | 1 | 0 | 1 | ||||
| País Vasco | 1 | 1 | 0 | 2 | ||||
| Asturias | 0 | 1 | 0 | 1 | ||||
| Galicia | 2 | 1 | 0 | 3 | ||||
| Islas Baleares | 1 | 1 | 0 | 2 | ||||
| Islas Canarias | 3 | 2 | 0 | 5 | ||||
| Total | 14 | 31 | 22 | 67 | ||||
Out of the 53 hospitals that stopped their surgical activity to one extent or another, 39.62% (21/67) of them decreased or stopped their surgical activity when the confinement period was decreed, between March 13 and 16. By frequency, this date was followed by March 30 and 23, with the shutdown of 15.09% and 11.32% of hospitals, respectively. It is striking that in 4 units (3 hospitals in Madrid and one in Zaragoza), the cessation of activity began long before the state of alarm was instated.
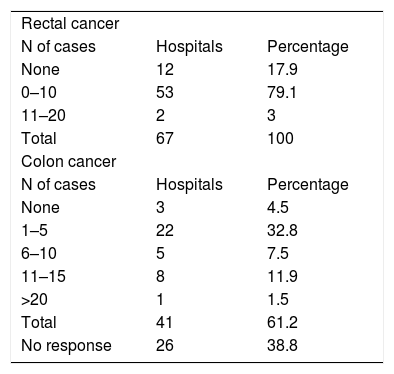
The number of rectal cancers that could not be treated surgically at the peak of the pandemic was less than 10 patients in most units (86.6%), except for 3 units in Catalonia, Asturias and Andalusia, which reported having between 11 and 20 patients awaiting surgery. This roughly shows (considering the limitations) that between 100 and 550 rectal patients would be waiting for surgery.
In the case of colon cancer, 22 units (32.8%) reported less than 5 patients on the waiting list, 8 units (11.9%) between 11 and 15 patients, and 3 units (4.5%) more than 16 patients, the latter being located in Catalonia and Madrid. In this case, we have estimated that between 172 and 320 colon cancer patients were awaiting intervention.
More specifically, the number of cases awaiting surgery was higher in the Madrid and Catalonia units, with more than 15 rectal cases and more than 20 colon cases.
As shown in Table 3, the mean number of patients operated was less than 10 cases, both for rectal and colon cancer.
Number of patients who underwent surgery during the pandemic for rectal and colon cancer.
| Rectal cancer | ||
| N of cases | Hospitals | Percentage |
| None | 12 | 17.9 |
| 0–10 | 53 | 79.1 |
| 11–20 | 2 | 3 |
| Total | 67 | 100 |
| Colon cancer | ||
| N of cases | Hospitals | Percentage |
| None | 3 | 4.5 |
| 1–5 | 22 | 32.8 |
| 6–10 | 5 | 7.5 |
| 11–15 | 8 | 11.9 |
| >20 | 1 | 1.5 |
| Total | 41 | 61.2 |
| No response | 26 | 38.8 |
Up to 65% of the units surveyed indicated having used neoadjuvant therapy or having lengthened the post-neoadjuvant/surgery period in patients with rectal cancer.
In this period, 40% of the units had to urgently treat at least 5 patients surgically due to complications of their colorectal cancer.
DiscussionSince the World Health Organization declared the pandemic on March 11, 2020, much has been written about COVID-19 and its importance in health.
In the field of colorectal cancer, the few publications that exist come from China, where drawing conclusions requires disaggregating data from series that globally contemplate various types of tumors.5 Other studies have merely given general recommendations on how to manage colorectal cancer patients during the pandemic.7–9
Special dedication has been given to rectal cancer, attempting to justify the use of short-cycle neoadjuvant therapy in order to facilitate compliance while avoiding patient risk of exposure, reducing the number of visits to the hospital.10,11
To date, there is no publication that provides data, at least approximate, of the impact that the pandemic has had on the healthcare activity in the field of colorectal cancer surgery. Nevertheless, logic suggests that the stoppage of elective activity must have caused an increase in the number of patients who have not been treated, and this will imply a backwater of patients requiring treatment that the healthcare system must come to terms with in coming months.
In Spain, as in other countries, the pandemic has hit the national territory unevenly, and some hospitals have not had the same reaction capacity as others.
We have detected that some areas of the country, regardless of the date of the declaration by the government of the national ‘state of alarm’, had already begun a total or partial stoppage of surgical activity in their units, although the majority (52.8%) did so after the government declaration.
The unequal impact of COVID-19 in the country has also been reflected in surgical activity. The autonomous communities of Madrid, Catalonia and the Valencian Community have suffered the most, and again, following the pattern of other European countries, the impact in southern Spain was less forceful, or at least more gradual.
Due to its lower incidence, fewer patients with rectal cancer have been affected by the pandemic than those with colon cancer. Also, the possibility of administering a bridge treatment, such as neoadjuvant therapy, may have also had an influence. The survey has indicated that its use or the lengthening of the completion-surgery period has been a resource used in almost 2/3 of the units. We do not have data on the preferential use of short-cycle versus long-cycle in the units surveyed.
With data from the survey, we have estimated that around 266 patients with colon cancer will need to undergo surgery after surgical activity resumes. In areas where the pandemic has had a greater impact, the restart of surgical activity will be slower. It is estimated that, in the best scenarios, the units will have 2–3 operating rooms available per week to resolve neoplastic diseases. Thus, at least a 30-day period will be needed to catch up with the accumulation of patients requiring surgery, assuming no new patients enter the circuit.
In those areas that experienced less pressure on the healthcare systems and in those areas that had the opportunity to react, a greater number of patients were treated surgically, and therefore fewer were left to operate. These units established their own strategies, regardless of the recommendations that were initially given —and later modified— not to operate on any cancer patients unless strictly necessary due to the high possibility of complications.12,13 In this context, the Spanish Association of Coloproctology adopted a more proactive position, recommending one approach or another depending on the pressure at that time of the pandemic on the local healthcare system. Thus, the ‘window of opportunity’ concept was established, in which patients with colorectal carcinoma were treated electively whenever possible.8,9 This has undoubtedly had an impact on the future of care in each hospital, as observed in our analysis.
One might expect that there would be an increase in the number of patients requiring urgent surgery at hospitals where elective activity was reduced. However, we have not detected this fact, and the number of urgent surgeries in the different Spanish ‘autonomous communities’ has remained similar, regardless of the impact on their healthcare system.
Bearing in mind that the survey does not represent the totality of coloproctology units in Spain, and with the limitations that this causes, the foregoing deserves deep reflection about the implications in the short and long term, especially if the pandemic spikes again. One would expect that, in a global national healthcare system, one not compartmentalized by autonomous communities, in order to avoid a collapse of its capacity to treat patients with colorectal cancer, patients should be allowed to be transferred and treated by trained units under less pressure. This would guarantee that patients would not have to wait for a long period of time, which would undoubtedly have an impact on prognosis.
Our second reflection is for the future. We must learn from this experience and plan surgery unit resources in a way that allows us to establish an effective protocol, before the collapse of the system impedes it.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the colorectal surgeons for their collaboration and participation in answering the survey of the Asociación Española de Cirugía Colorrectal, who assisted by sending the survey to its members.
Please cite this article as: de la Portilla de Juan F, Reyes Díaz ML, Ramallo Solía I. Impacto de la pandemia sobre la actividad quirúrgica en cáncer colorrectal en España. Resultados de una encuesta nacional. Cir Esp. 2021;99:500–505.