Wandering spleen (WS) is an uncommon entity originated by a congenital or acquired laxity of the peritoneal ligaments, which causes an ectopic location of the spleen in the abdominal cavity.
The first description of this clinical entity was reported by Van Horne in 1667 as an incidental finding in an autopsy. The real incidence of this problem is not known, but its rareness has been documented in a series of 1413 splenectomies where the incidence was 0.16%. It usually presents in middle aged adults and is more common in women in a proportion of 20:1.1
Symptoms are usually vague and non-specific, although in cases of torsion of the vascular pedicle it can present as an acute abdomen. This presentation is uncommon.
We present two cases of wandering spleen, one an incidental finding and the other that presented as an acute abdomen.
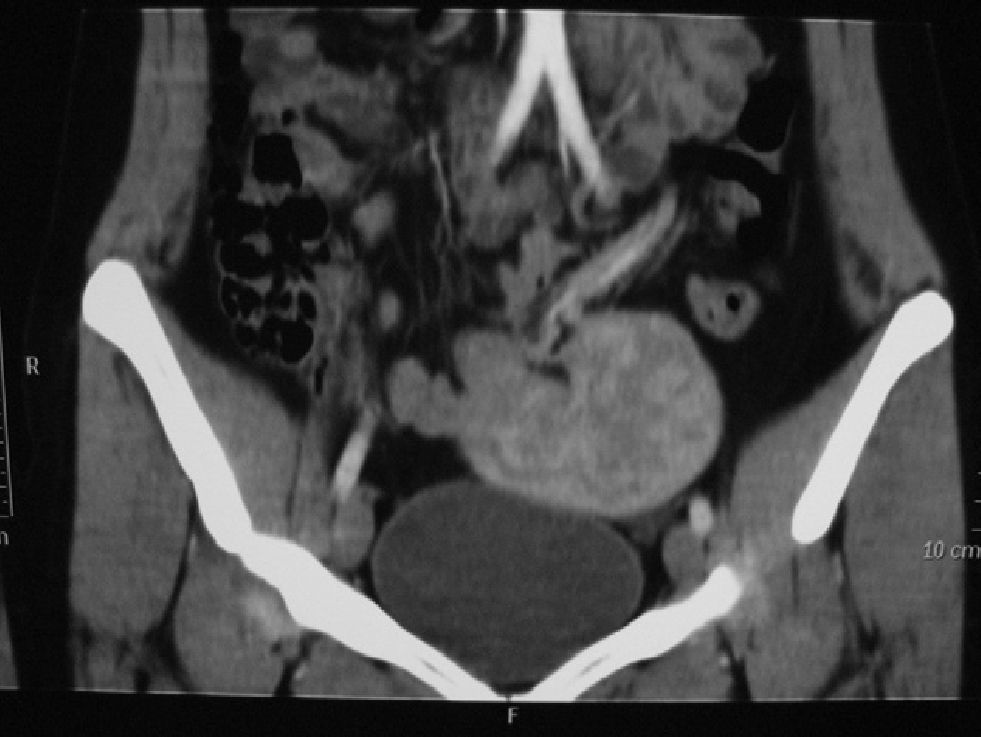
Case 1A 30 year-old woman with no prior medical history was diagnosed of a pelvic mass in a routine gynecological exam. A CT scan of the abdomen identified a homogenous mass on top of the bladder with hilar vessels compatible with a wandering spleen; the vascular pedicle descended from the left upper quadrant (Fig. 1).
Elective surgery was scheduled. A laparoscopic splenectomy was performed using a Hasson trocar for creation of the pneumoperitoneum and two 10mm trocars. The vascular pedicle was dissected with a white GIA and the spleen was removed through the umbilical trocar.
The patient had an uneventful recovery and was discharged three days after surgery. Three weeks after surgery an antipneumococcal vaccination was administered.
Case 2A 25 year old woman with no prior medical history presented to the emergency department for abdominal pain located in the left upper quadrant and vomiting. On arrival she presented a temperature of 38°C and on physical examination had diffuse abdominal pain with signs of peritoneal irritation.
Blood tests revealed leukocytosis of 20.06×103μl−1, with neutrophils of 857% and fibrinogen of 10g/l; all other parameters were normal.
An abdominal CT scan revealed splenomegaly with no contrast uptake and a “whirl sign” at the vascular pedicle, indicative of torsion.
A left subcostal laparotomy was performed that revealed an enlarged spleen with no ligament fixation that was free in the peritoneal cavity, and torsion of the vascular pedicle. After de-torsion the spleen remained ischemic and a splenectomy was performed. The patient had an uneventful postoperative recovery and was discharged 8 days later. Three weeks after surgery an antipneumococcal vaccination was administered.
DiscussionA wandering spleen is caused by the absence or abnormal development of the normal ligaments that hold the spleen into position: the gastrosplenic ligament, the splenorenal ligament and the phrenocolic ligament. This laxitude allows the spleen to be mobile and can fall freely into the peritoneal cavity, and be predisposed to complications.2,3
The clinical presentation is variable; it can be an incidental finding in an asymptomatic patient or can cause different symptoms in cases of torsion, depending on the degree of vessel rotation.4
Imaging methods are very useful for the diagnosis of this entity. Ultrasound can show its abnormal location, and can frequently show an enlarged spleen with homogenous echostructure or heterogeneous structure (infarction or congestion) depending on the degree of torsion. In cases of torsion or infarction, a CT scan can show a “whorled appearance” of the vascular pedicle and an absence of intravenous contrast uptake.5,6
Treatment of the wandering spleen has changed over time. Initially an expectant management was defended, but this was associated with a high rate of morbidity, and therefore splenectomy was advised in all cases. In recent years the importance of the spleen for immunity has been better studied and conservative management is again recommended when possible.
At present, the treatment of choice is de-torsion and splenopexy when there are no signs of irreversible ischemia; in these cases a splenectomy should be performed. A splenopexy can be performed using different techniques: fixing the splenic capsule to the left upper quadrant or the anterior abdominal wall; with or without the use of polyglycolic acid mesh. In recent years laparoscopic de-torsion and splenopexy using mesh has been described with apparent similar results to open surgery.7
Please cite this article as: Pérez-Legaz J, Moya Forcén P, Oller I, Arroyo A, Calpena R. Bazo ectópico. ¿Cirugía urgente o programada? Cir Esp. 2013;91:344–345.