Between 5 and 15% of cholecystectomized patients can present episodes of abdominal pain similar to the pain that motivated the original indication for surgery.1,2 This is given the name “post-cholecystectomy syndrome”.
The etiology is quite varied and can be secondary to biliary disorders, such as residual choledocholithiasis, biliary dyskinesia, bile leak or stenosis, or other non-biliary diseases.3,4 Although less frequent, there are also reports of cystic duct remnant syndrome.
We present the case of a 55-year-old woman with a history of cesarean section and open cholecystectomy 11 years earlier due to lithiasic cholecystitis. Since the intervention, the patient had experienced sporadic episodes of colicky abdominal pain in the right upper quadrant that was self-limiting and not related with food intake, accompanied by nausea and vomiting, which partially improved with analgesia. The work-up of one of her recent episodes showed mildly elevated transaminase and bilirubin levels, which is why she was referred to us for further studies.
On physical exploration, the right subcostal abdominal scar was observed to have no alterations, no pain and no signs of peritoneal irritation. Lab work parameters (including hemogram, biochemistry with liver enzymes, thyroid hormones, alpha-1-antitripsin, ceruloplasmin, total protein, viral serology and coagulation) were within normal levels. Abdominal ultrasound showed the liver to be normal, with no focal lesions, cholecystectomy, and linear hyperechoic images with posterior acoustic shadow in the gallbladder bed related to the cystic duct, with no other pathological findings.
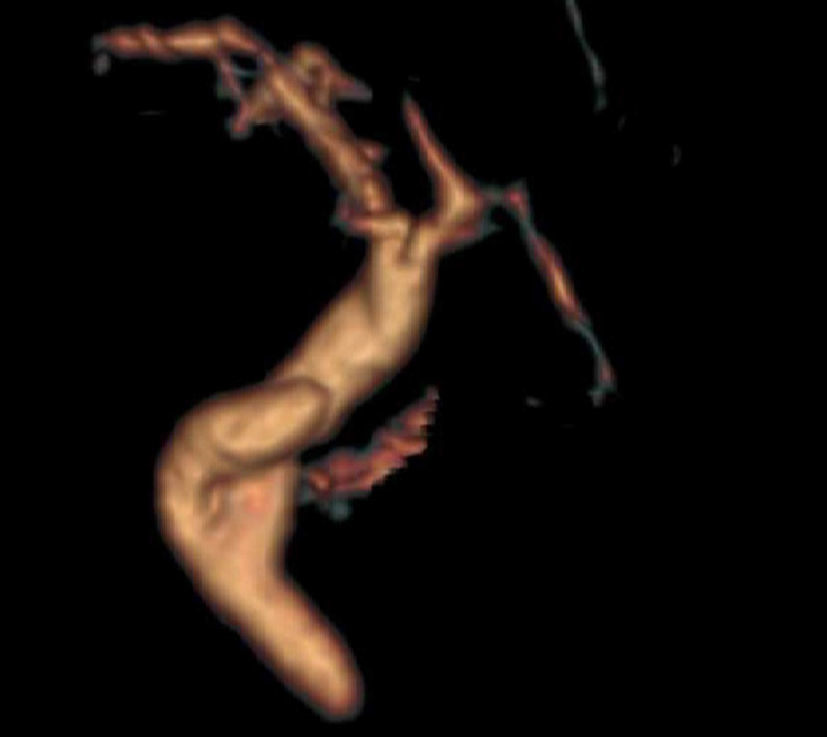
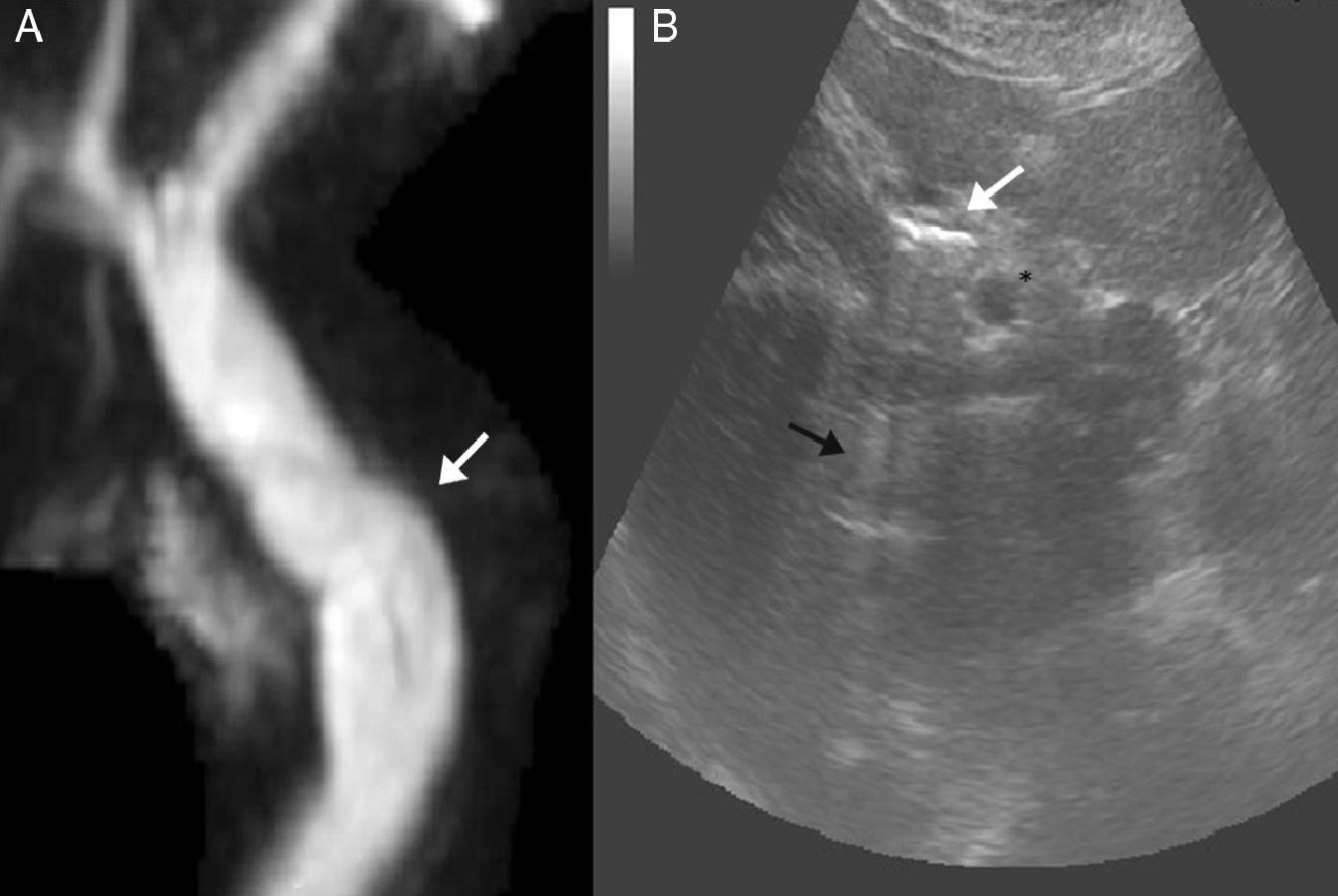
Given the ultrasound findings, a magnetic resonance cholangiopancreatography study reported a long, dilated cystic remnant, with an image of probable calculus in its interior, and normal common bile duct (Figs. 1 and 2).
(A) Magnetic resonance cholangiopancreatography with no clear images of calculi in the interior of the cystic stump; (B) abdominal ultrasound image showing the common bile duct (*) adjacent to the elongated cystic stump, with hyperechoic images in its interior (white arrow) creating a non-artifacted posterior acoustic shadow (black arrow), suggestive of calculi.
With these findings, surgical treatment was proposed, but the patient dismissed this option. Dietary treatment was recommended, and the patient has remained asymptomatic during these 6 months of follow-up.
A cystic duct remnant has been defined as a residual cystic duct greater than 1cm which can cause post-cholecystectomy syndrome when calculi are present in its interior.5,6 This syndrome can occur at any time, from the immediate postoperative period to even years after cholecystectomy,1 producing symptoms similar to biliary colic and even episodes of cholestasis, as in our case. It is an uncommon cause of post-cholecystectomy syndrome, although it is not known whether this condition could become more frequent in the future due to the growing number of laparoscopic cholecystectomies in recent decades.6,7
The diagnosis may include ultrasound, computed tomography, sphincter of Oddi manometry and scintigraphy of the biliary system in cases of biliary dyskinesia,3 although magnetic resonance cholangiopancreatography is the current non-invasive technique of choice for the evaluation of the biliary tree in these cases, versus endoscopic retrograde cholangiopancreatography.2,5,8 Nevertheless, other extra-biliary causes should be ruled out, such as irritable bowel syndrome, peptic ulcer, hepatitis or neuromas, among other possible more frequent etiologies.3,9 The implication of this condition in post-cholecystectomy syndrome has been questioned but, when other etiologies have been ruled out and imaging tests demonstrate a long cystic remnant with calculi1 with no other anomalies or findings, it can be considered diagnostic.
In our case, the magnetic resonance cholangiopancreatography showed evidence of an elongated cystic stump, although with no clear observation of calculi in its interior because of the poor resolution (Fig. 2A). Abdominal ultrasound, however, showed the presence of linear hyperechoic images with posterior acoustic shadow in the interior of the residual cystic duct adjacent to the common bile duct, suggestive of calculi (Fig. 2B). The differential diagnosis by ultrasound with metal clips could be considered, but the procedure had been done by open surgery without the use of these materials, and the ultrasound image of such materials is that of hyperechoic material with artifacted posterior acoustic shadow.
This syndrome can be associated with other complications, such as bile leak, stenosis, neuromas, granulomas or mucocele, and it is a potential source of infection.
As for treatment, it has been reported that resection of the remnant seems to resolve the symptoms in a high percentage of cases,5,6,8 although fibrotic changes between the remnant and the main bile duct can entail increased risk in the laparoscopic approach compared with open surgery, although it is not a contraindication.2 Other proposed alternatives to surgical treatment are lithotripsy and CPRE.7
There seems to be a consensus that surgical treatment should be indicated in patients with recurring symptoms and demonstrated residual calculi in the cystic duct remnant, after other etiologies are ruled out. Although it has been proposed that calculi in the cystic stump should be identified and treated during cholecystectomy,10 the prevention of this syndrome should be based on proper dissection and anatomical identification of the union of the cystic and bile ducts.
Please cite this article as: Márquez Rojas J, Medina Ortiz JA, Martínez Mateo YA, Matito Díaz MJ, Arribas Jurado M. Síndrome del muñón cístico: ¿quimera o realidad? Cir Esp. 2014;92:496–497.