Oncoplastic surgery is an essential tool in the surgical approach to women with breast cancer. These techniques are not absolute guarantee for a good cosmetic result and therefore some patients will have cosmetic sequelae secondary to poor surgical planning, the effects of adjuvant treatments or the need for resection greater than originally planned. The high frequency of these cosmetic sequelae in oncology practice makes it necessary to classify them for optimal surgical planning. The aim of this paper is to present a classification of cosmetic sequelae after oncoplastic procedures to identify those factors that are crucial to its prevention. This classification contains 4 groups: breast contour deformities, asymmetries, alterations in nipple-areola complex (NAC) and defects in the three dimensional structure of the breast. A significant group of these sequelae (asymmetries and deformities) are associated with breast irradiation and need an accurate information process with patients to set realistic expectations about cosmetic results. Finally, there is another group of sequelae (NAC disorders and three-dimensional structure) that are related to poor planning and deficiencies in surgical approach, therefore specific training is essential for learning these surgical techniques.
La cirugía oncoplástica es una herramienta fundamental en el tratamiento quirúrgico de la mujer con cáncer de mama. Sin embargo, la realización de una técnica oncoplástica no es garantía absoluta de un buen resultado estético y, por ello, algunas pacientes pueden presentar secuelas estéticas tras su realización ya sea por una deficiente planificación quirúrgica, por los efectos de los tratamientos adyuvantes o por la necesidad de una resección mayor de la inicialmente prevista. La relativa frecuencia de estas secuelas estéticas en la práctica oncológica hace necesario clasificarlas para optimizar la planificación quirúrgica. El objetivo de este artículo es describir y clasificar las secuelas estéticas que pueden aparecer tras un procedimiento oncoplástico con el fin de identificar aquellos factores que son determinantes en su aparición y prevención. Esta clasificación incluye 4 grupos de secuelas que se corresponden con las deformidades del contorno mamario, las asimetrías, las alteraciones del complejo aréola-pezón (CAP) y los defectos en la estructura tridimensional de la mama. Un grupo significativo de estas secuelas (asimetrías y deformidades) se relacionan con la irradiación mamaria y hace necesario un proceso informativo veraz con las pacientes para fijar unas expectativas reales en el resultado estético. Finalmente, existe otro grupo de secuelas (alteraciones del CAP y estructura tridimensional) que se relacionan con una planificación y ejecución deficiente del procedimiento oncoplástico, lo que hace imprescindible una formación específica para el aprendizaje de estas técnicas quirúrgicas.
Oncoplastic surgery is an essential tool in the surgical treatment of women with breast cancer, which allows improvement of the quality of breast conservation and optimises the irradiation of this organ. Oncoplastic surgery is a set of techniques selected based on the type of breast and the tumour location; these techniques are used to apply the concept proposed by Audretsch et al.1 in 1998 of a specific surgery for each breast and for each tumour. Different studies2–5 have shown that the oncological outcomes of these techniques are comparable to the ones obtained with a traditional, conservative surgery (tumourectomy, quadrantectomy) but are superior in the case of multifocal/multicentric6 cancers and also from an aesthetic viewpoint, since they enable mammary remodelling and symmetry with the opposite breast. These results are applicable both to early7 and locally advanced8,9 breast cancer. However, performing an oncoplastic technique is not an absolute guarantee of a good aesthetic result and, therefore, some patients may have aesthetic sequelae after these procedures due to deficient surgical planning, the effects of adjuvant treatments or the need of a resection larger than initially planned. The incidence of these sequelae has ranged from 0% to 18% according to the systematic reviews conducted by Asgeirsson et al.10 and Haloua et al.11 The relative frequency of these aesthetic sequelae in oncology practice makes it necessary to classify them and critically analyse their characteristics in order to identify those triggering factors that will enable their prevention during surgical planning.
The aim of this paper is to describe and classify aesthetic sequelae after oncoplastic procedures to identify those factors that are crucial to their occurrence and prevention.
Classification of Aesthetic Sequelae in the Operated BreastLogically, the local resection of the breast predisposes to the development of defects in breast contour and volume, although their frequency and severity will depend on the tumour location, the anatomical type of the breast and the amount of resected tissue.12 The breast retraction caused by irradiation over the healing area also adds to those factors. The first classifications of breast aesthetic defects were focused on those derived from tumourectomies or quadrantectomies in women operated with an indication of breast conservation. Thus, Clough et al.13,14 ranked defects into types I, II and III, taking into account the presence of asymmetries, breast contour deformities and the development of a rock-hard breast after radiotherapy, respectively. Munhoz et al.15 have recently proposed a classification that relates the type of breast (low, mid and high volume) and the resected tissue (less than 15%, 15%–40%, more than 40%). This combination results in nine clinical situations for which the authors predict the severity of the deformity and propose a corresponding preventive action. Nevertheless, the usefulness of these classifications is limited. Firstly, because they do not address defects secondary to an oncoplastic procedure, since they are focused only on abnormalities secondary to a tumourectomy/quadrantectomy. Secondly, because they only take into account abnormalities in the breast volume (asymmetries) and contour (deformities) but fail to consider abnormalities in the nipple–areola complex (NAC) or in the three-dimensional structure of the breast. Finally, these classifications cannot be used as a basis for recommendations for the prevention of aesthetic defects following an oncoplastic procedure.
Table 1 shows the four groups of aesthetic sequelae that may occur in the breast following resection and oncoplastic remodelling. These groups correspond to breast contour deformities, asymmetries, NAC abnormalities and defects in the three-dimensional structure of the breast.
Types of Aesthetic Sequelae After Oncoplastic Breast Surgery.
| Group | Type of abnormality | Causes | Prevention |
|---|---|---|---|
| Breast contour deformity | Segmental traction of the skin envelope | – Enlargement in the UIQ, small breast and lower pole– Haematoma and breast infection | – Preoperative assessment of the multifocal component– Consider a mastectomy in small breasts– Early evacuation of haematoma/infection |
| Disfiguration of breast contour | – Acting on an irradiated breast. Resection and local remodelling in irradiated tissue | – Limited breast resection– Remodelling with vertical pattern | |
| Bulge in breast contour | – Fat necrosis of breast | – Local resection and remodelling according to fat necrosis extension | |
| Breast asymmetry | Volume asymmetry | – Abnormality due to adjuvant treatment: fibrosis of the irradiated breast, growth of the healthy breast with antihormone treatment– Not performing a technique to correct the asymmetry in vertical and horizontal patterns– Unnecessary technique to achieve symmetry: correcting the asymmetry of the non-dominant breast | – Correct the asymmetry in the vertical and horizontal patterns– Assessment of previous asymmetry and refrain from correcting the asymmetry of the non-dominating breast– Assessment of previous asymmetry– Evaluate the weight of each surgical specimen– Increased resection in the dominant breast |
| Shape asymmetry | – Symmetry is not achieved in small breast resections– Use of vertical patterns with different pedicles | – Correct asymmetry in the vertical and horizontal patterns– Vertical patterns with identical pedicles | |
| Sequelae on the NAC | Necrosis of the areola/nipple | – Venous ischaemia in vertical pattern– Arterial ischaemia in vertical pattern | – Careful dissection of the inferior pedicle– Subcutaneous release of the upper pedicle– Avoid intramammary compartment syndrome– Early identification of vascular suffering |
| Pigmentation abnormality | – Transient ischaemia of the NAC | – Careful dissection of the inferior pedicle– Subcutaneous release of the upper pedicle– Avoid intramammary compartment syndrome | |
| NAC contour deformity | – Limited or irregular [outspread] of the NAC– Fibrous bridle in lateral pattern | – Preparation of a round and wide [outspreading] area– Lateral resection independent from the NAC shift | |
| Asymmetry in diameter and height of NAC | – Wrong choice of areola marker– Wrong measurement of vertical branches | – Use of an areola marker of a gauge similar to the original areola size– Design of vertical branches of identical length | |
| Abnormality in the vertical/horizontal axis | Excessive exposure of the lower pole | – Vertical pattern with prolonged vertical branch– Horizontal pattern in breast pseudoptosis | – Design of vertical branch measuring 5–6cm– Horizontal pattern extended to the lower pole |
| Excessive breast width | – Vertical pattern with very closed vertical branches | – Vertical pattern with open vertical branches | |
| Low breast projection (flat breast) | – Design with closed vertical branches | – Design with open vertical branches | |
| Depletion of the lower pole | – Vertical pattern with an upper pedicle >8cm | – Design of a inferior pedicle | |
| Redundant skin envelope of the breast | – Design of low horizontal branch | – Design of high horizontal branch | |
NAC: nipple–areola complex; UIQ: upper-inner quadrant.
A breast contour deformity is a rare sequelae when the oncoplastic procedure planning is adequate to the process extension and to its location in the breast. Under this premise, planning should consider not only the defect secondary to tumour excision but also the actions needed for defect remodelling. In order to attain this goal, it is crucial to have the information provided by radiological tests, which outline the tumour's local extension and degree of dissemination, and the pathology report, which will guide us with respect to tumours more likely to behave as multifocal/multicentric cancers (extensive ductal carcinoma in situ, infiltrating lobular carcinoma), in which case a larger local excision will be required.
Breast contour deformities may be grouped into three different subtypes depending on their impact on the skin envelope:
Deformities by Local/Segmental Traction of the Skin EnvelopeIt is a more or less extensive depression in the breast contour resulting from the skin retraction due to the absence of tissue in the surgical resection area, which intensifies after breast irradiation.16,17 There are two causes that lead to the development of this aesthetic defect during the postoperative progress: the enlargement of the surgical margins due to an oncological need and the presence of local complications in the surgical bed. In the first situation, the need for a larger excision of local tissue may limit the remodelling capacity of the oncoplastic procedure and, consequently, post-irradiation deformities will appear. The prevention of this adverse effect is based on an adequate preoperatory assessment of the extension and degree of dissemination of the neoplastic process, especially in small-volume breasts where a skin-sparing mastectomy with immediate reconstruction may be the best alternative.
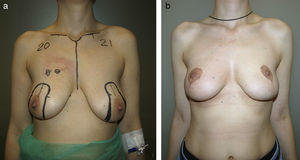
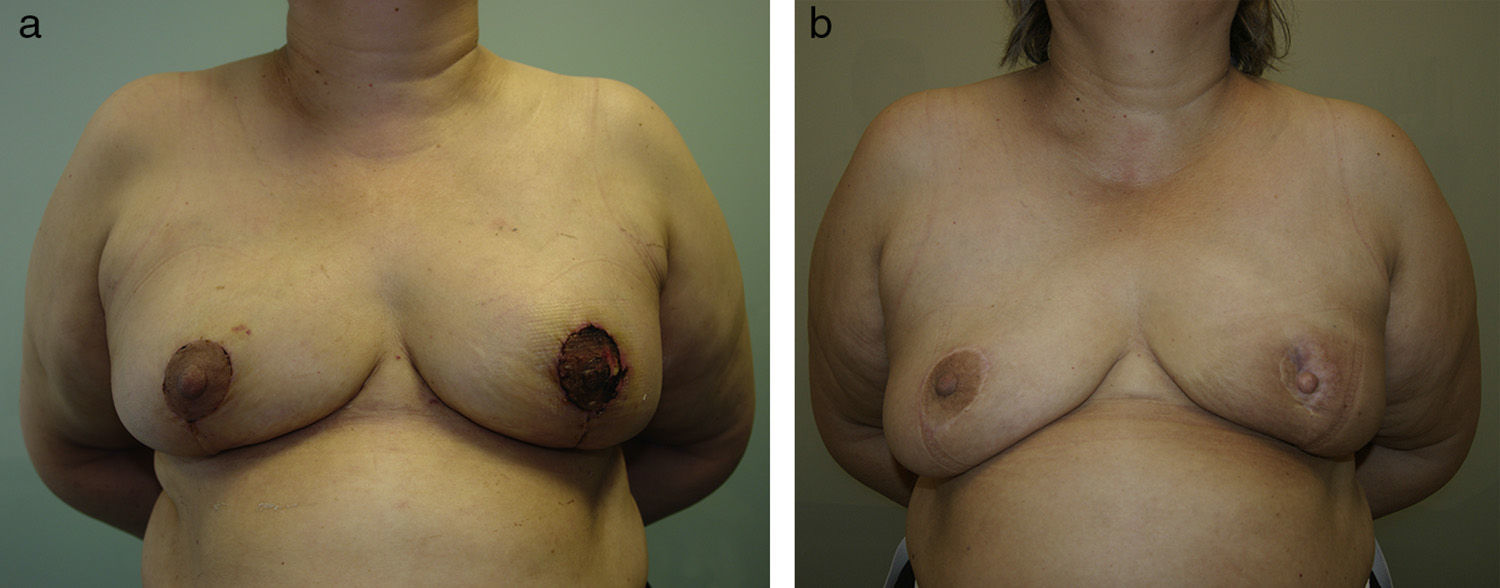
Additionally, the occurrence of local complications (bleeding, infection, skin necrosis) during the postoperative period of an oncoplastic procedure increases the possibility of breast contour deformities due to the loss of local tissue by the lysis of fat and mammary parenchyma (Fig. 1). An early evacuation of the haematoma or abscess is a decisive factor to mitigate the impact of these events on the aesthetic result.
Overall Disfiguration of the Breast ContourIrradiated breasts react unpredictably to the surgical actions performed on them but, in any case, there is always a high risk of breast contour deformities: the greater the remodelling, the higher that risk will be. The vertical pattern is the oncoplastic procedure that yields the best results in irradiated breasts since, in most cases, only an umbilication of the vertical wound will be visible, without further deformities in the breast contour.
Bulges in the Breast ContourOnce the presence of local recurrence has been ruled out, the presence of a prominence as a breast contour deformity is exclusive of fat necrosis. In Tenofsky's18 experience, fat necrosis occurs in 25% of oncoplastic procedures and 9.5% of tumourectomies. It is a complication with a wide clinical variability during the postoperative course of an oncoplastic procedure. At one end, there are local involvements, common in the remodelling of post- tumourectomy defects by dermoglandular flaps, which only require anti-inflammatory treatment and whose aesthetic repercussion is minimal since it is limited to a palpable nodule that does not alter the breast contour (Fig. 2). At the opposite end, there are extensive fat necroses that manifest themselves by segmental plaques that protrude over the breast contour or deform it by the traction exerted on the skin. This kind of complication is typical of vertical mammoplasties in large-volume breasts, especially gigantomastia, and with a great amount of fatty component. In these cases, the local resection of the necrosis will cause large defects and significant breast deformity, particularly in irradiated breasts, requiring oncoplastic remodelling either with the resources from the breast itself or with a myocutaneous flap.
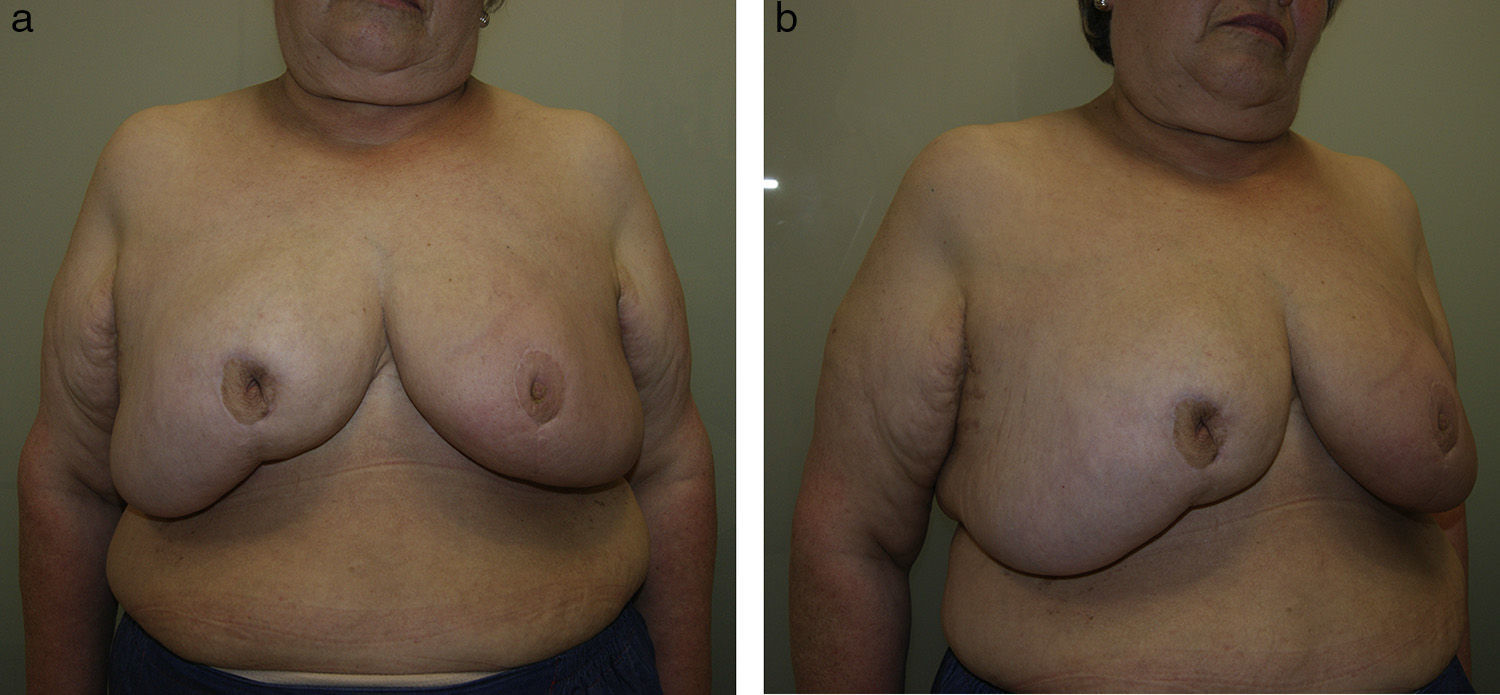
AsymmetriesEven though asymmetry is a natural condition of the female breast, conservative surgeries always involve an enhancement of volume and shape differences between both breasts due to the effects of resection and irradiation on the sick breast. The study of Exner et al.19 has shown that age and tumour size are the variables related to the development of asymmetry and, therefore, asymmetry will be more common in elderly women and patients with larger-sized tumours. Asymmetries after an oncoplastic procedure may be due to abnormalities in the breast volume or shape.
Breast Volume AsymmetriesThis is the most frequent aesthetic abnormality following an oncoplastic procedure due to the impact of adjuvant treatments on the breast, which may be summarised as fibrosis, with reduced volume, in the sick breast and increased volume in both breasts as a consequence of antihormone therapy. It is important to check for asymmetry prior to the oncoplastic procedure to avoid enhancing the asymmetry during the postoperative period. Thus, the most common mistake is to try to seek symmetry in women with a predominant sick breast, since many of them will not require a resection in the healthy breast, which would preserve the previous asymmetry, but only a resection of the cutaneous component of the pattern to guarantee a similar shape between both breasts.
The second cause of volume asymmetry is failing to indicate a correction of the asymmetry in the healthy breast during oncoplastic planning. The larger the amount of resected tissue, the more intense the asymmetry; therefore, the patterns with a greater capacity of resection (vertical and horizontal mammoplasty) are the ones that have a stronger impact on symmetry compared to procedures with a lower resection volume (tumourectomies by tunnelling, round-block, lateral approaches). For this reason, the correction of breast volume asymmetry is necessary in the vertical and horizontal patterns whereas, in the remaining patterns, acting on the healthy breast would be indicated for the prevention of breast shape asymmetry.
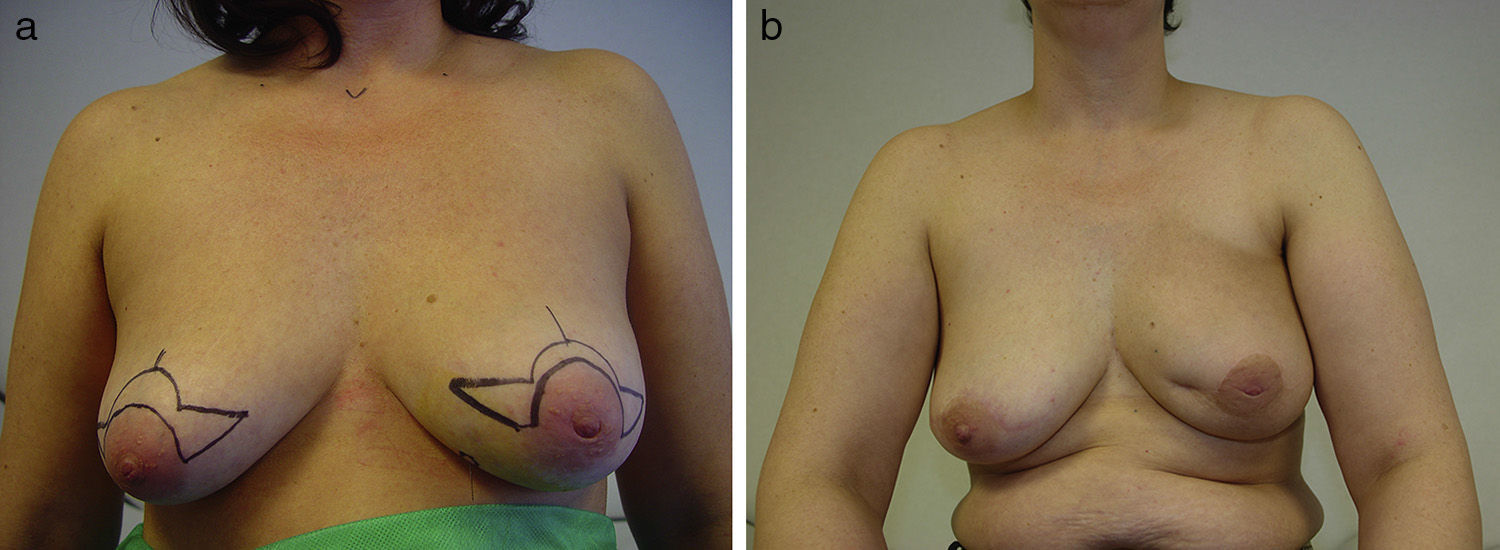
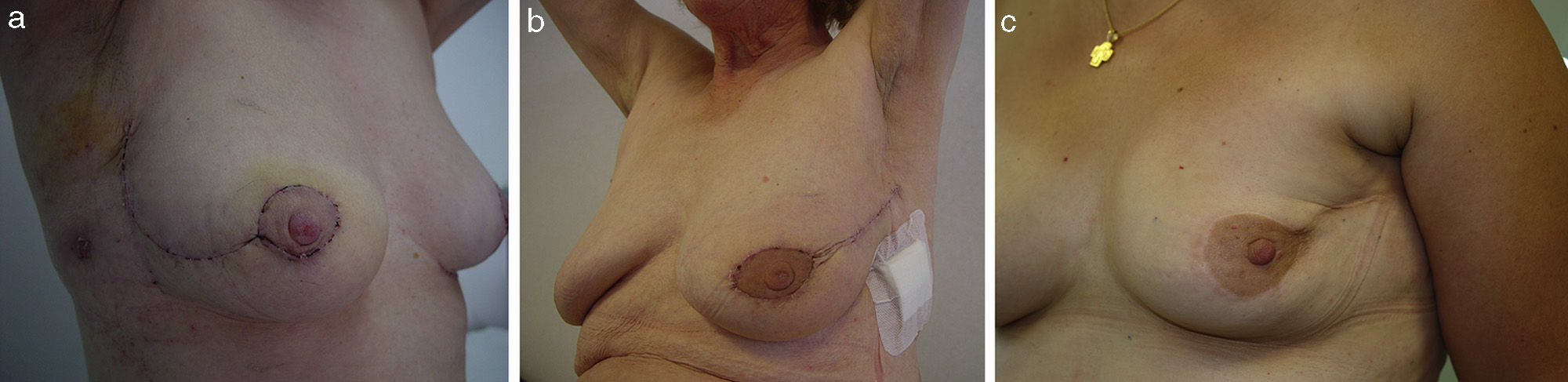
Breast Shape AsymmetriesUnlike the above, the main cause of breast contour asymmetry is the very planning of the oncoplastic procedure. Thus, failure to act on the healthy breast in women with an indication of vertical or horizontal pattern may result in breasts of identical volume, when resections are smaller than 50g, but with an asymmetry in the shape of the breast (Fig. 3). The second cause of contour asymmetry affects patients with a bilateral vertical pattern in whom the vascularisation of the NAC is planned with different pedicles. In most cases, this difference in lower pole fullness is compensated over time, except if irradiation in the breast is started a few weeks after the surgical procedure.
Breast shape asymmetry after a unilateral vertical pattern. This patient rejected a procedure for symmetry on her left breast after the indication of a vertical mammoplasty. Even though the amount of tissue removed from the right breast was scarce, performing a unilateral vertical pattern resulted in breast shape asymmetry although both breasts have a similar volume.
The NAC is a decisive item in normal breast morphology and, consequently, sequelae in this complex have a relevant impact on the definitive aesthetic result of an oncoplastic procedure. The final objective of an oncoplastic plan is that the NAC be located at the centre of the new breast, with a regular and wide areolar expansion. However, there are intraoperative circumstances conditioning the defects in the aesthetic result of the NAC, which may be summarised in the following abnormalities.
Necrosis of the Nipple–Areola ComplexThe limited vascularity of the NAC plays a key role in the viability of this anatomical structure and in one of its morphological qualities: pigmentation. Vertical mammoplasty is the procedure with the highest risk for this adverse event, which is exceptional in the remaining oncoplastic techniques where the NAC irrigation is guaranteed. The incidence of necrosis of the NAC following a vertical mammoplasty for cancer is similar to the incidence seen in aesthetic surgeries,20 ranging from 0% to 10%,21 although the risk increases in women with gigantomastia.22 Necrosis due to an insufficient venous drainage is the determining factor in most cases of necrosis of the NAC and, in most instances, it is related to planning an inferior pedicle, since in those cases the NAC is disconnected from the breast's superficial drainage, thus limiting the venous return to the intercostal perforating vessels. On the contrary, the upper pedicle preserves the superficial vein network, ensuring the drainage of the NAC and reducing the likelihood of venous necrosis. These ischaemic phenomena can be prevented with a careful dissection of the inferior pedicle, ensuring good implantation in the chest wall to collect the highest possible number of perforating vessels, as well as an early detection of the insufficient venous drainage during pattern closure.
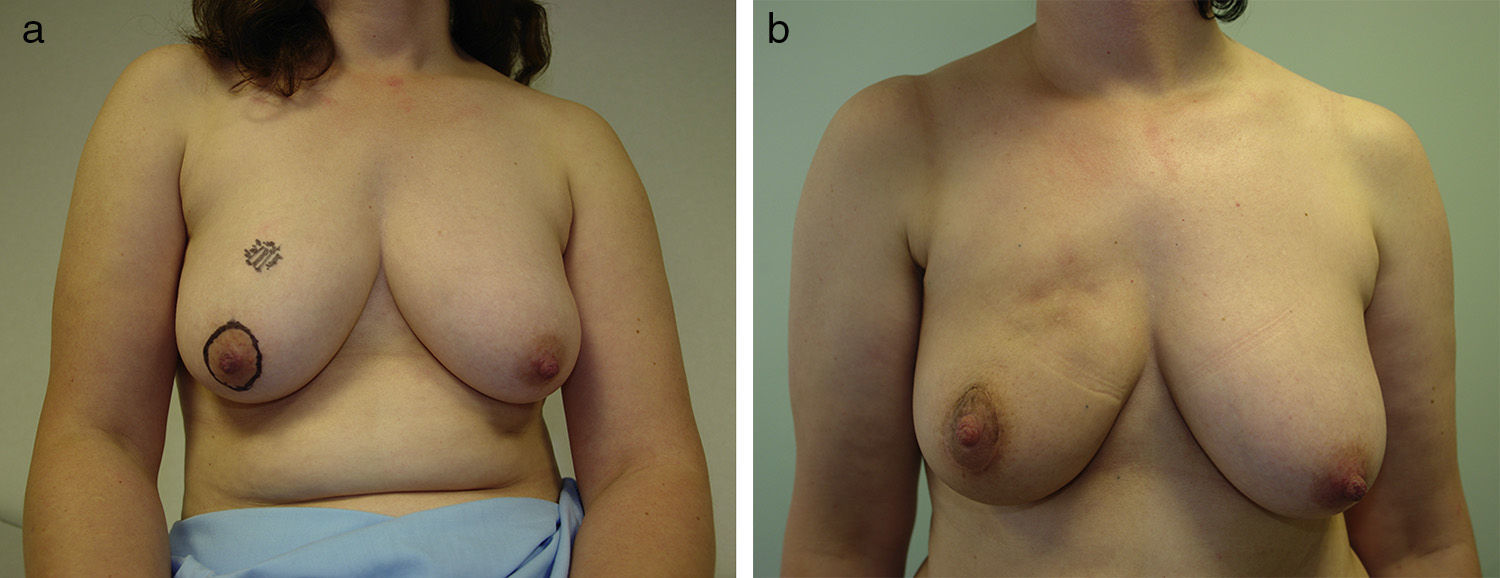
Pigmentation Abnormalities in the Nipple–Areola ComplexPigmentation sequelae also relate to episodes of transient ischaemia in the NAC that result in the selective death of some melanocytes. This complication is noted some weeks after the surgical procedure and, in most cases, it is preceded by a superficial necrosis of the epidermis (Fig. 4). Once the skin cover of the areola has regenerated, the pigmentation defect becomes evident in the area affected by the superficial necrosis. Pigmentation sequelae are more evident in darker areolas and go unnoticed in patients with areolas with little pigmentation. Tattooing this defect with a pigment similar to the original colour is the best option for its resolution.
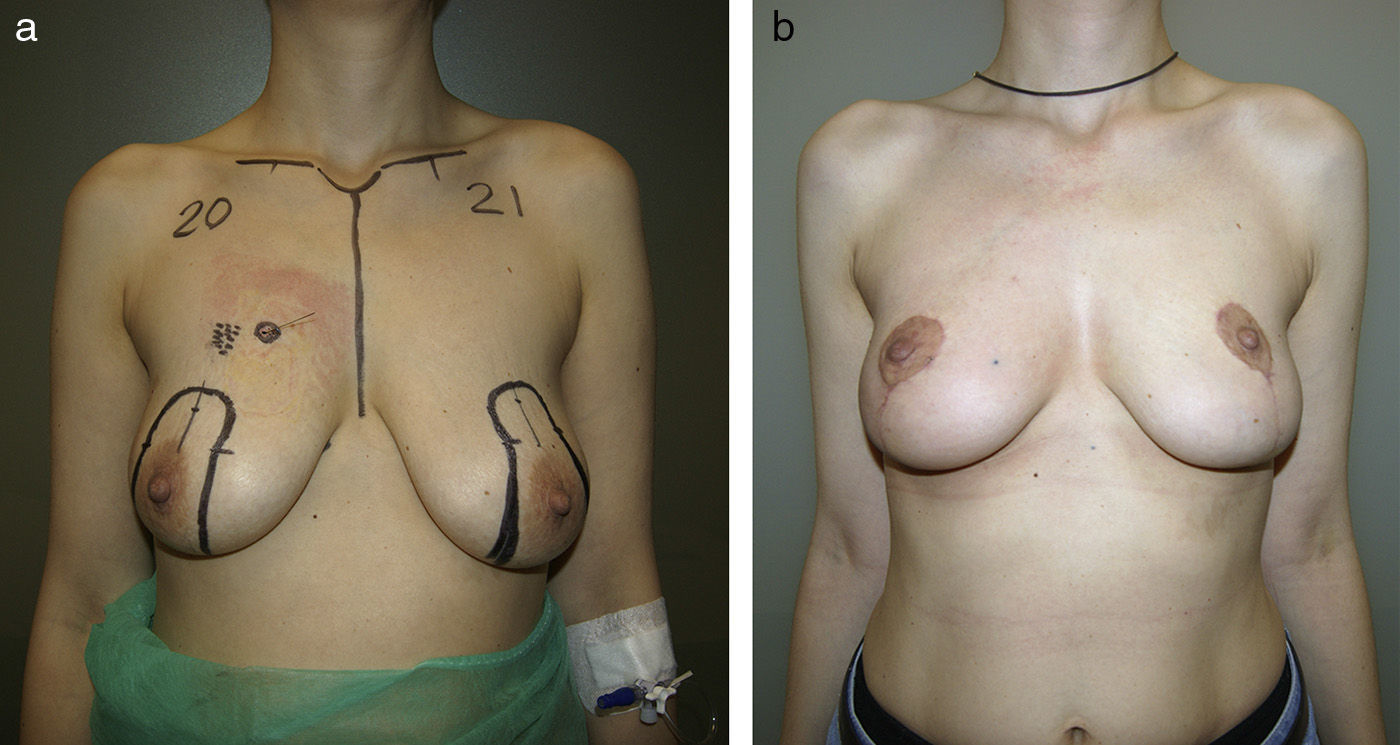
Contour Deformities in the Nipple–Areola ComplexThese sequelae result from poor planning during NAC closure (Fig. 5). The most common defects are small-sized areolas (minimal visibility) and areolas with a distorted contour (elliptical areola). The prevention of these defects is simple: outspreading the areola on a circular pattern with the areolar marker during the last phase of the surgical closure. This action ensures round, extended areolas with sufficient diameter for an optimal visualisation of the NAC at the centre of the new breast. In patients undergoing a lateral mammoplasty, a contour distortion of the NAC secondary to the lateral traction of the surgical wound can be seen. Its prevention is based on a separate design of the lateral and the circular patterns so that both wounds will not be in contact.
Asymmetry of the Nipple–Areola ComplexThe asymmetry of the NAC can occur in two circumstances. The first one is related to differences in the NAC diameter when the oncoplastic procedure is unilateral, and is usually associated with a NAC of large diameter which, after the surgery, is reduced to the size of the areolar marker used. The second circumstance is related to an asymmetry at the NAC level following a bilateral vertical mammoplasty. The source of this asymmetry is an unequal planning of the height of the pattern's vertical branches, either by a mistake in the pattern preparation or due to the participation of two different surgical teams.
Abnormalities in the Three-Dimensional Balance of the BreastPerforming an oncoplastic procedure requires that the new breast look harmonic in its three dimensions: height, width and projection. For that purpose, surgical planning should consider the procedure's impact on each of these variables to avoid sequelae attributable to a disproportion among them. Undoubtedly, the vertical pattern is the procedure demanding the greatest effort to achieve this goal and, therefore, most aesthetic sequelae in this group will occur in patients undergoing this procedure.
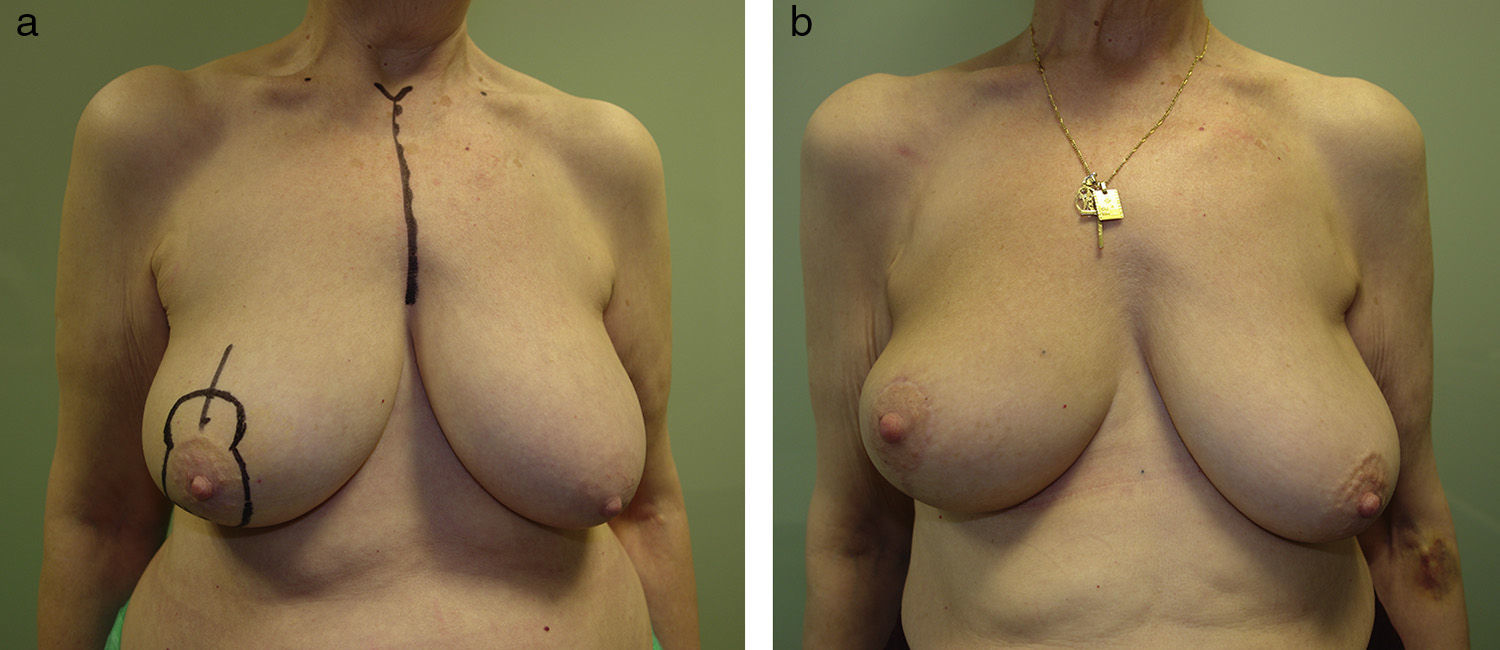
Excessive Exposure of the Lower PoleActions conducted on the breast's horizontal axis have an impact on the new breast's NAC height and are responsible for situating this anatomical structure at the centre of the new breast. Inappropriate planning may lead to the NAC being placed above the breast's horizontal axis, which visually translates into an excessive lower pole and the sensation that the NAC is excessively elevated (Fig. 6). In surgical practice, this excessive exposure of the lower pole may occur with either a horizontal or vertical pattern. In the first case, the excessive exposure is due to a significant shift of the NAC in very ptotic breasts. A simple preoperative assessment can prevent these sequelae by manually moving the NAC to its new location to check whether there is an excessive exposure of the lower pole; if that is the case, a horizontal pattern extended to the lower pole should be planned. On the other hand, the vertical pattern may display an excessive exposure of the lower pole in two circumstances. The first one is related to planning an excessively long vertical branch (longer than 7–8cm), in which case prevention will be based on preparing a 5-cm long vertical branch. The second circumstance is related to the occurrence of pseudoptosis after a vertical procedure, i.e., the NAC remains at the level of the inframammary fold but most of the breast contents go down to the lower pole, depleting the upper pole. This outcome is typical of fatty breasts with little glandular component and its prevention is difficult.
Redundant Skin EnvelopeThe second sequelae associated with the breast's horizontal axis is a redundant skin envelope, a defect exclusive of vertical patterns and characterised by the presence of a skin flap surpassing and hanging from the inframammary fold (Fig. 7). The source of this abnormality is based on planning a horizontal branch too low while designing a Vise [sic: Wise] pattern for voluminous breasts; its prevention is based on a high outline of the horizontal branch, particularly the lateral one.
Breast Projection AbnormalitiesActions on the vertical axis have an influence on breast projection. The aesthetic defect most frequently associated with this arrangement is creating a scarcely projected breast as a consequence of faulty planning of the pattern's vertical branches. In this case, the design of vertical branches with little opening will result in the creation of a flat breast with little projection, a defect that may be easily prevented if the pattern is designed with a wider opening of the vertical branches, especially in women who have fatty breasts with little glandular component.
In conclusion, the oncoplastic surgery of breasts presents a wide range of aesthetic sequelae; it is necessary to know and classify such sequelae in order to prevent them. A significant group of these sequelae (asymmetries and deformities) are related to breast irradiation inherent to the conservative management of breast cancer. Therefore, we must provide patients with truthful information in order to set realistic expectations vis-à-vis aesthetic results. Finally, there is another group of sequelae (NAC and three-dimensional abnormalities) that are related to the faulty planning and execution of the oncoplastic procedure, which makes specific training crucial to learning these surgical techniques.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Acea Nebril B, Cereijo Garea C, García Novoa A. Secuelas estéticas en cirugía oncoplástica de la mama. Clasificación y principios para su prevención. Cir Esp. 2015;93:75–83.








![Areola contour abnormalities: (a) lack of [outspreading] in the lower pole; (b) elliptical areola due to a mistake when [outspreading] the circular pattern; (c) distortion of the areolar contour by traction of the surgical wound in a lateral mammoplasty. Areola contour abnormalities: (a) lack of [outspreading] in the lower pole; (b) elliptical areola due to a mistake when [outspreading] the circular pattern; (c) distortion of the areolar contour by traction of the surgical wound in a lateral mammoplasty.](https://static.elsevier.es/multimedia/21735077/0000009300000002/v1_201501230041/S2173507714005341/v1_201501230041/en/main.assets/thumbnail/gr5.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)