Diverticular disease of the appendix is an uncommon condition, with an incidence from 0.004% to 2.1%. It usually occurs between the fourth or fifth decades of life, does not present gastrointestinal symptoms but only insidious abdominal pain. Patients usually delay consultation, leading to increased morbidity and mortality. The aim of this study was to determine the clinical features of diverticular disease of the appendix.
MethodsA retrospective study of all patients undergoing appendectomy in a tertiary hospital between September 2003 and September 2013 was performed.
ResultsDuring this period, 7044 appendectomies were performed, and 42 cases of diverticular disease of the appendix were found, which represents an incidence of 0.59%. A total of 27 patients were male. The mean age was 46.6±21 years. The average hospital stay was 4.5 days. A perforated appendix was identified in 46% of patients. In 80% of the cases, a complementary imaging test was performed. The incidence of neoplastic disease with diverticulum of the appendix was 7.1%.
ConclusionsDiverticular disease of the appendix is an incidental finding. In its acute phase, it presents as an acute appendicitis. The treatment of choice is appendectomy. It presents a higher risk of developing neoplastic disease of the appendix.
La enfermedad diverticular del apéndice es infrecuente, con una incidencia que varía desde 0,004 a 2,1%. Suele presentarse entre la cuarta o quinta década de vida, con ausencia de síntomas gastrointestinales y dolor abdominal insidioso. Los pacientes habitualmente consultan de forma tardía, con el consiguiente aumento de morbimortalidad. El objetivo de este estudio fue determinar las características clínicas de la enfermedad diverticular del apéndice.
MétodosSe realizó un estudio retrospectivo de todos los pacientes operados de apendicectomía en un hospital terciario desde septiembre de 2003 hasta septiembre de 2013.
ResultadosDurante este periodo se realizaron 7.044 apendicectomías, encontrándose 42 casos de enfermedad diverticular del apéndice, que representa una incidencia de 0,59%. De ellos, 27 pacientes fueron de sexo masculino. La edad media fue de 46,6±21 años. El promedio de la estancia hospitalaria fue de 4,5 días. El 46% de los casos presentaban perforación del apéndice. En el 80% de los casos se realizó una prueba de imagen complementaria. La incidencia de neoplasia asociada a enfermedad diverticular fue de 7,1%.
ConclusionesLa enfermedad diverticular del apéndice es un hallazgo incidental. En la fase aguda presenta síntomas indiferenciables de la apendicitis aguda. El tratamiento de elección es la apendicectomía. Presenta una mayor probabilidad de desarrollar neoplasias del apéndice.
Diverticular disease of the vermiform appendix is an uncommon pathology that is diagnosed as a pathological finding in patients who have undergone appendectomy.1 Its incidence varies between 0.004% and 2.1% of surgical specimens, and it is classified according to histopathologic characteristics into 4 different types.1,2
Appendicular diverticulitis is usually erroneously considered a variant of acute appendicitis; nonetheless, there are some differences in both the symptoms as well as the physiopathology of both diseases.3 Generally, patients are in the fourth or fifth decades of life and usually present with localised pain in the right iliac fossa, similar to acute appendicitis, which should be included in the differential diagnosis.4 However, the clinical presentation may occasionally be different, with the absence of gastrointestinal symptoms and mild abdominal pain, so patients visit their physician later on and there is a delay to establish the diagnosis. This increases the risk of perforation, with the resulting increase in morbidity and mortality. Nonetheless, close to 70% of patients with appendicular diverticulitis are treated surgically because of a diagnostic impression of acute appendicitis.5–7
The present study analyses and describes the clinical and pathological characteristics of patients affected by diverticular disease of the vermiform appendix over the last 10 years at the 12 de Octubre Hospital in Madrid.
MethodsWe conducted a retrospective analysis of all the appendectomies done at the 12 de Octubre Hospital from September 2003 to September 2013. In a total of 7044 specimens examined, 42 cases of appendiceal diverticulitis were found.
Clinical and demographic characteristics (age, sex, leukocytes, complementary imaging tests and evolution time from the onset of symptoms until intervention) were collected from the files of patients with appendiceal diverticular disease. Furthermore, data from the pathology studies of the appendices with diverticula were analysed.
This study was based on existing pathology reports. All surgical specimens were analysed by a pathologist.
The data analysis was done with the SPSS version 16.0 statistical programme.
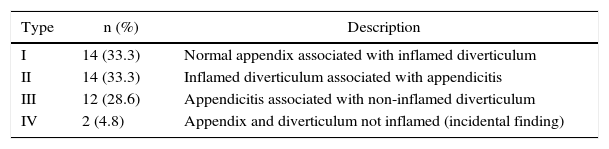
ResultsForty-two cases of diverticulitis of the appendix were found, which represented an incidence of 0.59%. Twenty-seven patients were men, 15 were women, and mean age was 46.6±21.7 (range 9–88). Table 1 shows the classifications of the appendiceal diverticulitis and the incidence observed in our series. Inflammation of the diverticula was present in 66.6% of the cases, while in 61.9% inflammation of the appendix was observed, compatible with acute appendicitis. Combined inflammation of the diverticulum and appendix was observed in 33.3% of the cases.
Classification of Appendiceal Diverticulitis and Its Incidence in this Study.
| Type | n (%) | Description |
|---|---|---|
| I | 14 (33.3) | Normal appendix associated with inflamed diverticulum |
| II | 14 (33.3) | Inflamed diverticulum associated with appendicitis |
| III | 12 (28.6) | Appendicitis associated with non-inflamed diverticulum |
| IV | 2 (4.8) | Appendix and diverticulum not inflamed (incidental finding) |
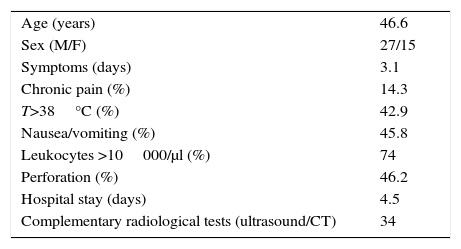
Table 2 shows the clinical and demographic characteristics of patients with appendiceal diverticular disease; also, it can be observed that 46.2% of cases presented a perforated appendix. Mean hospital stay was 4.5 days. In 81% of cases, complementary radiological studies were done, especially ultrasound and computed tomography (CT), when there was no clear diagnosis.
Clinical and Demographic Characteristics of Appendiceal Diverticulitis.
| Age (years) | 46.6 |
| Sex (M/F) | 27/15 |
| Symptoms (days) | 3.1 |
| Chronic pain (%) | 14.3 |
| T>38°C (%) | 42.9 |
| Nausea/vomiting (%) | 45.8 |
| Leukocytes >10000/μl (%) | 74 |
| Perforation (%) | 46.2 |
| Hospital stay (days) | 4.5 |
| Complementary radiological tests (ultrasound/CT) | 34 |
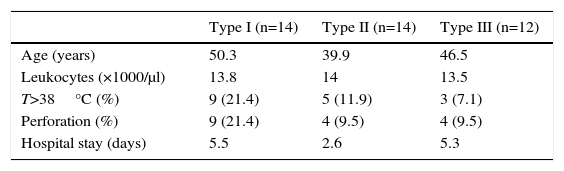
Table 3 shows some clinical characteristics and compares them among the different types of diverticular disease. Types I and II have been observed with greater frequency, representing 66.6% of all patients, while the age at presentation was older in type I. Fever, the incidence of appendiceal perforation and hospital stay were also greater in type I.
Clinical Characteristics According to Type of Diverticular Disease.
| Type I (n=14) | Type II (n=14) | Type III (n=12) | |
|---|---|---|---|
| Age (years) | 50.3 | 39.9 | 46.5 |
| Leukocytes (×1000/μl) | 13.8 | 14 | 13.5 |
| T>38°C (%) | 9 (21.4) | 5 (11.9) | 3 (7.1) |
| Perforation (%) | 9 (21.4) | 4 (9.5) | 4 (9.5) |
| Hospital stay (days) | 5.5 | 2.6 | 5.3 |
Type IV was observed in 2 patients.
The incidence of neoplasms associated with diverticular disease was 7.1% (Table 4).
DiscussionDiverticular disease of the vermiform appendix was reported in 1893 by Kelynack.7 According to their histopathological characteristics, appendiceal diverticula are classified as congenital or true diverticula and acquired or pseudo-diverticula.7,8 Congenital diverticula are unique and located on the antimesenteric border of the appendix; they have been associated with other diseases like trisomy D (13–15) or Patau syndrome.9 Acquired diverticula lack a muscularis propria layer in the wall, are more frequently located in the distal third of the appendix on the mesenteric edge and are usually small in size (2–5mm). These latter type are more prevalent and therefore not associated with colonic diverticula.9,10 In our series, all the patients presented acquired or pseudo-diverticula.
In 1989, Lipton et al.11 reported the morphological classification of diverticular disease of the caecal appendix. There are 4 different types, and type I (classical) is the most frequent, with a prevalence of around 40–50%.12 In our study, we observed that types I (33.3%) and II (33.3%) were most frequent.
Certain risk factors have been described for this pathology, such as: age over 30, male sex, history of cystic fibrosis and Hirschsprung disease.9 The disease can present in 2 types: one that is acute, resulting from an inflammatory process similar to acute appendicitis, and another of recurring chronic pain.3,13 In our study, 14.3% of patients presented a history of chronic abdominal pain. The main complication is perforation, with an incidence of up to 66%, which entails a higher mortality rate when compared with acute appendicitis. In our series, perforation was seen in 46% of cases.
The use of diagnostic imaging studies like ultrasound and CT are non-specific for the diagnosis of appendiceal diverticulitis, although they are useful to differentiate it from other causes of abdominal pain.7,13 Lee et al. state that most cases of appendiceal diverticulitis can be differentiated from acute appendicitis with CT when interpreted by experienced radiologists, as the inflamed diverticula have the appearance of small cystic protrusions in the appendix, accompanied by increased IV contrast uptake in the diverticular wall.13,15,16 In our study, complementary radiological tests (abdominal ultrasound and CT) were done in 81% of patients. It is interesting that all the radiological diagnoses were acute appendicitis and that none of the cases were diagnosed as diverticular disease of the appendix.
The complications of appendiceal diverticulitis vary from chronic pain, acute inflammation and perforation to the risk of developing neoplasms.7 In Table 2, it is curious that the age and incidence of perforation of an inflamed diverticulum are greater in type I than in the rest. 42% of low-grade mucinous neoplasms of the appendix are associated with this disease, so it is therefore recommended that all appendectomy specimenss that present diverticula be thoroughly examined to exclude concomitant neoplastic disease.7,17,18
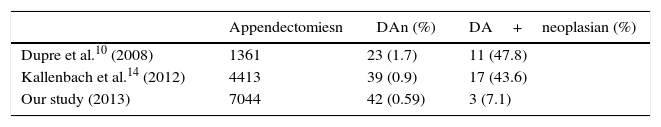
Dupre et al. demonstrated a statistically significant association between the presence of diverticulosis of the vermiform appendix and neoplasms (47.8%), especially carcinoid tumours and mucinous adenomas.10,19 Moreover, there are studies, such as the article by Stockl et al., that report a 42% association between the presence of Schwann cell proliferation in the mucosa and the presence of appendiceal diverticulitis.20 In our series, there are no reports of Schwann cell proliferation. In addition, it has been observed that the association between diverticulosis of the appendix and neoplasms is observed in 7.1%, which is a very low percentage compared to other studies (Table 2).
The treatment of choice for appendiceal diverticulitis is the same as for appendicitis: appendectomy. Laparoscopic appendectomy is feasible in these cases. Prophylactic appendectomy is recommended when appendiceal diverticula are found during a surgical procedure in order to prevent the risk of later complications or the coexistence of neoplasms.
In conclusion, diverticular disease of the appendix is generally an incidental finding. Appendiceal diverticulitis debuts with abdominal pain in the right iliac fossa, with symptoms in the acute phase that are indistinguishable from those of acute appendicitis.
The treatment of choice is appendectomy. Furthermore, prophylactic appendectomy is recommended in all patients in whom appendiceal diverticula are identified as an intraoperative finding due to the greater risk of complications in these cases, such as perforation and associated mortality. In addition, there is a high risk of developing pseudomyxoma peritonei in some patients with appendiceal diverticula as they present a higher incidence of mucinous tumours of the appendix.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Marcacuzco Quinto AA, Manrique M A, Calvo P J, Loinaz S C, Justo A I, Caso M O, et al. Implicaciones clínicas de la enfermedad diverticular del apéndice. Experiencia en los últimos 10 años. Cir Esp. 2016;94:44–47.