Less than 3% of osteomyelitis cases are osteomyelitis of the clavicle. Depending on the microorganism involved, patients typically present localized or acute pain associated with regional edema and positive blood cultures, or a more chronic and indolent form of the disease. Fever (60%), localized edema or mass (30%) and soft tissue abscesses (30%) are the most frequent symptoms. Staphylococcus aureus is the most commonly involved microorganism. Nonetheless, other types of microorganisms may be involved, such as gram-negative bacteria or Mycobacterium tuberculosis.1
Our patient is a 54-year-old male with a personal history of morbid obesity, arterial hypertension, diabetes mellitus and hepatocarcinoma, who was not a candidate for liver transplantation and had been treated with chemoembolizations. One year before, he presented a painful cervicothoracic mass associated with cellulitis. Cervical ultrasound showed a suprasternal soft tissue mass with inflammatory characteristics and gas in its interior. It protruded into the mediastinum and seemed to originate in the acromioclavicular joint. At that time, the patient was treated by the Thoracic Surgery Department with drainage of cervical, right infraclavicular and anterior mediastinal abscesses, followed by closure in a second stage. Cultures of the samples obtained during surgery showed growth for Escherichia coli-ESBL. The patient was discharged and continued follow-up with the Thoracic Surgery Department.
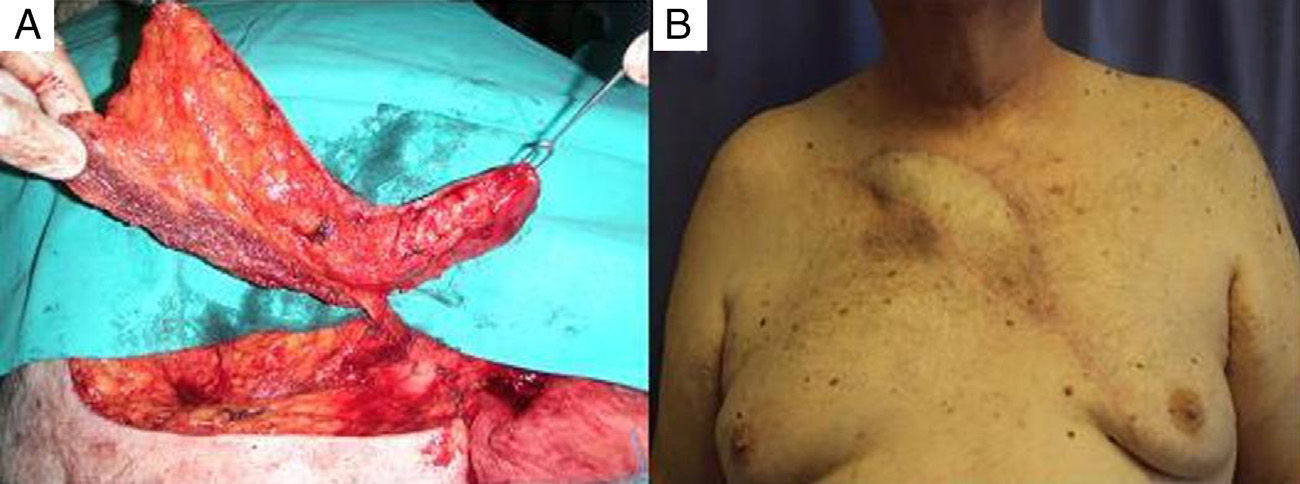
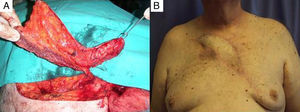
One year later, the patient reappeared in our consultation, once again with symptoms of reddening of the cervicothoracic region and the presence of a fistula in the sternoclavicular region with purulent liquid discharge (Fig. 1). The culture was positive for E. coli and had the same characteristics as the culture from the previous intervention. At that time, another cervicothoracic CT scan was performed, which demonstrated a skin ulcer of approximately 7cm, associated with a fistulous tract that reached the right sternoclavicular joint, irregular surfaces of the right sternoclavicular joint and subchondral sclerosis at the proximal end of the first rib as well as in the manubrium of the sternum. A persisting soft tissue mass that surrounded the acromioclavicular joint was observed. Given these findings, the Plastic Surgery and Thoracic Surgery teams decided to operate together. In this second surgery, all of the soft tissue and bone that were involved were resected, including the right sternoclavicular joint, manubrium of the sternum, first right sternocostal articulation and the medial third of the first rib. The coverage of the defect created was performed using a skin and muscle “propeller” flap of the left pectoralis major, based on the internal mammary artery perforator of the second intercostal space (Fig. 2A). After 2 years of follow-up, the patient presented stable coverage and the symptoms have not reappeared (Fig. 2B).
Clavicular osteomyelitis is a rare condition in adults. It is associated with a series of predisposing factors, such as rheumatoid arthritis, diabetes, immunosuppressant therapies, intravenous drug addiction, previous joint trauma, head and neck surgery, and subclavian vein catheterization.2
The most commonly isolated etiologic agent is S. aureus. Septic arthritis due to gram-negative germs, as in the case of our patient, are less common and usually appear in patients with chronic diseases that weaken the immune system, such as diabetes mellitus, cirrhosis of the liver and cancer.2
Imaging tests are essential to establish whether there is bone and joint involvement, and cervicothoracic CT is the test of choice.3 To reach a definitive diagnosis, however, it is necessary to culture the microorganism involved in the bone fragment, joint fluid, or blood culture.4
The basic pillar in the treatment of patients with osteomyelitis is debridement. This procedure is surgeon-dependent and, when done correctly and after having eliminated all the devitalized soft tissue and bone from the wound, a large part of the bacterial inoculum is eliminated along with unviable tissue that may contain bacteria.
The following step in treatment is to achieve adequate, stable coverage of the defect that has been created by incorporating richly vascularized tissue. This allows the area to heal and also provides better penetration of antibiotics and defenses, transforming an anaerobic area into an aerobic one. The use of muscle flaps or perforating flaps that include the muscle paddle, as in this present case, has been shown to be clearly superior to skin flaps or grafts to cure chronic osteomyelitis.5,6
The third step in the treatment of chronic osteomyelitis is the prolonged use of intravenous antibiotics. Several experts recommend a total duration of between 4 and 6 weeks of intravenous treatment.7,8 Currently, empirical therapy with a third-generation cephalosporin is recommended, which is later adjusted according to the antibiogram.1
Please cite this article as: Lima Sánchez J, Sánchez Medina MT, García Duque O, Fernández-Palacios J. Osteomielitis crónica esternoclavicular: cirugía de rescate con colgajo de perforante de arteria mamaria interna. Cir Esp. 2015;93:129–131.