Hemangiomas are benign vascular tumors that usually derive from organs such as the skin, liver or kidneys and are usually diagnosed in childhood. Histologically, there are 3 types: cavernous, hamartomatous and arteriovenous malformations. The esophageal location of hemangiomas is uncommon, representing 3% of all benign tumors of this organ; they are usually single lesions situated in the lower third of the esophagus. Esophageal hemangiomas may cause obstructive and/or hemorrhagic symptoms: dysphagia, dyspnea, hypersalivation, episodes of aspiration, recurring respiratory infection, hematemesis and melenas. Diagnosis in adults of a hemangioma in the hypopharynx or the cervical esophagus is a clinical rarity, and only a few isolated cases have been published in the medical literature.1 We present the clinical case of a cervical esophageal hemangioma diagnosed in an adult.
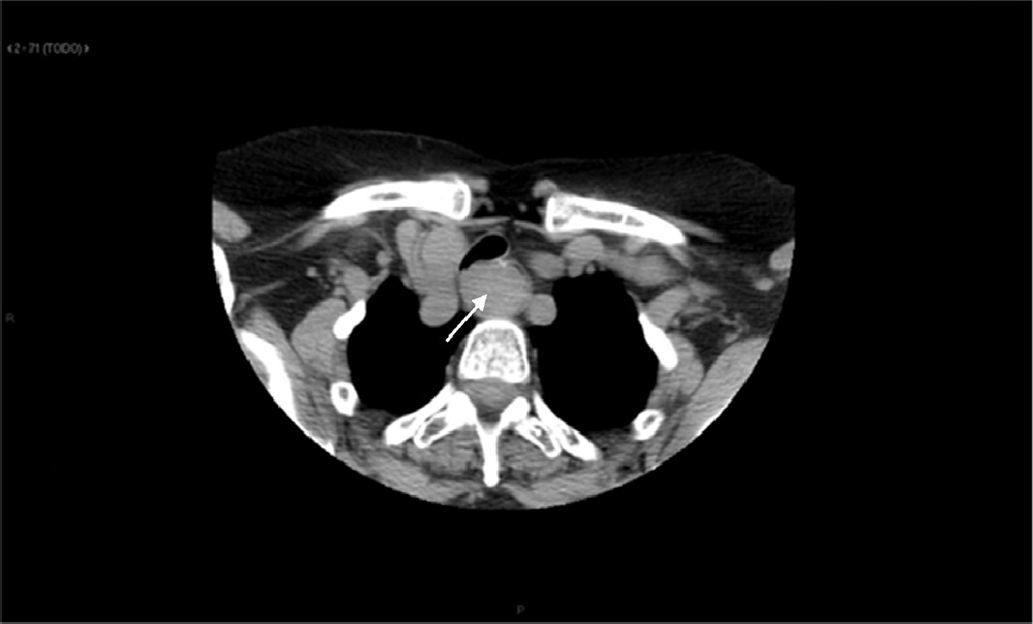
The patient was a 68-year-old woman with no medical history of interest. During computed tomography (CT) study for chronic cough (Fig. 1) a lesion measuring 2.6cm×2.1cm×3.3cm was detected in the proximal third of the esophagus, which obstructed almost the entire lumen and protruded over the posterior wall of the trachea. After the administration of intravenous contrast, there was mild homogeneous uptake, giving the mass a solid appearance. These findings were not considered conclusive for diagnosis. Endoscopic ultrasound (EUS), after passing Killian's area, showed a subepithelial lesion in the right lateral-cervical region that was completely passable and measured 26mm×17mm, which seemed dependent upon the muscular tissue itself. It was rather heterogeneous and presented hypo- and hyperechoic images. The differential diagnosis included leiomyoma and gastrointestinal stromal tumor (GIST). Therefore, a positron emission tomography-CT (PET-CT) was performed, which detected no fluorodeoxyglucose (FDG) uptake in the mass.
With the findings from the EUS and PET-CT, the probable diagnosis of leiomyoma was established. Although the patient reported no digestive symptoms, we decided to operate because of the uncertain exact nature of the lesion and its possible subsequent evolution. We used a left lateral cervical approach, which is the usual approach to the cervical esophagus in our department, and the mass was identified in the esophageal wall. After longitudinal myotomy, the lesion was observed to be benign in appearance, lobulated, dark blue in color and soft in consistency, which are characteristics compatible with hemangioma. We decided to perform an enucleation of the mass. It was closely adhered to the mucous membrane, which we opened in order to complete the separation from the mucosa without rupturing the tumor. The wall was closed on both the mucosal and muscular planes.
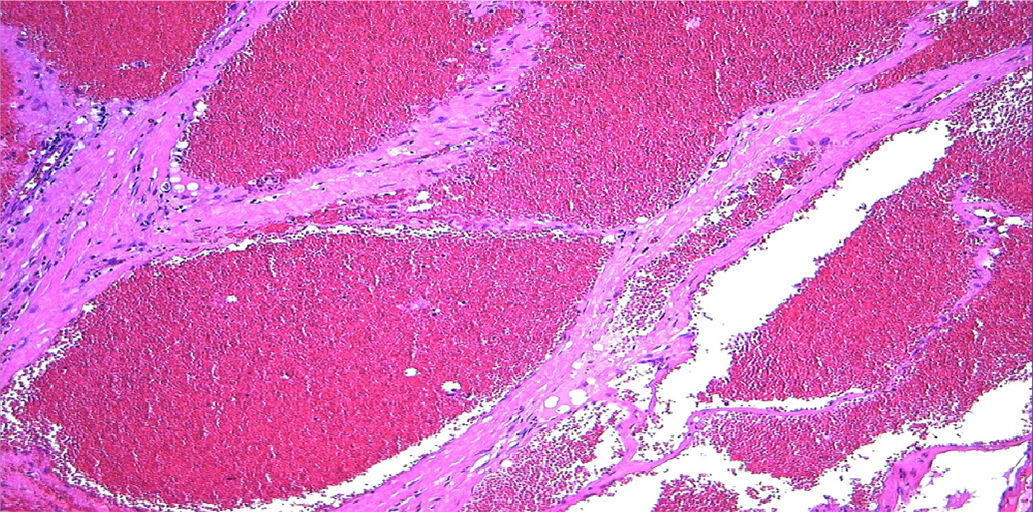
The pathological study with hematoxylin-eosin stain established the diagnosis of cavernous hemangioma (Fig. 2). The postoperative recovery was uneventful, with good tolerance to oral intake and a follow-up radiological transit series that showed no fistula or stenosis. The patient was discharged on the fourth day post-op.
Although we currently have sufficient available preoperative tests to be able to adequately direct the diagnosis, the low incidence of esophageal hemangiomas means that this pathology is often not thought of when establishing the differential diagnosis of a submucosal lesion in this organ, as occurred in our case. A barium swallow study can show evidence of the mass, but its findings are not specific. EUS is the most sensitive and specific diagnostic test for determining the location, depth and tumor size. EUS-Doppler shows the characteristic vascular changes within the hemangioma.2 On CT, these lesions usually appear as well-defined masses of soft tissue within the esophageal wall and show a marked uptake after the administration of intravenous contrast material. Calcifications – phlebolites are evident on CT and are considered specific findings of this tumor.3,4 Given the absence of phlebolites, as in our case, the radiological diagnosis is less certain and the differential diagnosis should include leiomyomas, polyps, neurofibromas and GIST. Other imaging tests that can be helpful are magnetic resonance imaging (MRI) or PET.2
Histological diagnosis by biopsy is also useful but not recommended as it may cause hemorrhage. Therapeutic options for hemangiomas depend on the severity of the symptoms and their evolution. They include a wide spectrum of options, from the administration of systemic or intralesional steroids to an endoscopic approach with different modalities: sclerotherapy, laser fulguration (KTP/YAG) and endoscopic mucosal resection (EMR).5,6 EMR or endoscopic polypectomy are especially indicated when the tumor is pedunculated and small in size (<25mm). Large tumors may predict the need for surgical resection. Thus, the indication for surgery is reserved for those cases in which other therapeutic modalities are not possible.2 Different surgical approaches have been used, from esophagectomy to the enucleation of the tumor by means of thoracotomy or laparoscopy. Surgical resection by esophagotomy is a safe and simple technique, especially when the tumor is large or located in the cervical esophagus.7
With this clinical case, we want to insist on the need for refining the preoperative differential diagnosis of submucosal esophageal lesions. In spite of its low incidence, hemangioma should be considered as it could substantially condition both the type of treatment as well as the approach and technique.
Please cite this article as: Alvarez Martín MJ, Garcia Navarro A, Diez Vigil JL, Becerra Massare P, Ferrón Orihuela A. Hemangioma de esófago cervical. Cir Esp. 2014;92:494–495.