Psychogenic causes for some somatic symptoms have been widely recognised. In Ophthalmology however, there are few studies that address this issue, and current Ophthalmology Training Programs do not include formal teaching in Psychosomatics. Psychosomatic phenomena in ophthalmology are probably under-diagnosed, which may reduce therapeutic effectiveness, decrease patient and physician satisfaction, and increase health costs due to multiple consultations and prescriptions. The aims of this study were to describe patients with unexplained visual/ocular symptoms (UVOS), and to estimate the prevalence of psychological distress (PD) among them.
Materials and methodsConsecutive adults with UVOS were recruited over a 12 month period. Complete medical history and ocular examination were performed to rule out organic disease. Psychological Distress was defined by the presence of one or more of the following criteria: psychiatric diagnosis, use of psychotropic medication, psychosomatic disease in other organs, and biographical crisis in the last 6 months. Results were compared with a control group.
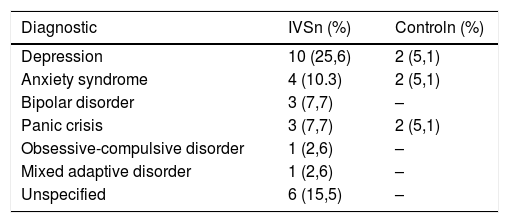
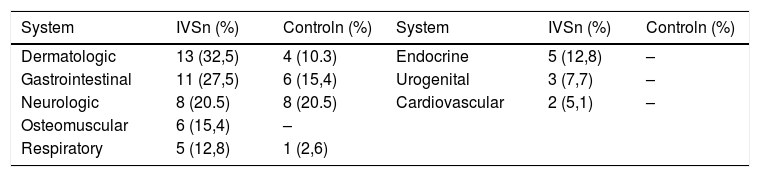
ResultsA total of 39 cases of UVOS were recruited, corresponding approximately to 3% prevalence. The large majority (74%) were female. The mean age was 41.8 years. The most common complaints were ocular surface irritation symptoms (51%) and unspecific visual disturbances (17%). At least 1 of the PD criteria was found in 100%, including 46.2% with psychiatric comorbidity, 48.7% with psychotropic medications, 64% with psychosomatic disease in other organs, and 48.7% with recent life-stressful events. PD indicators were statistically higher compared with control group (P<.05).
ConclusionsThere was a high frequency of Psychological Distress indicators in patients with UVOS. Although the causative role of PD remains unclear, the presence of UVOS should warn the ophthalmologist of an underlying psychic conflict and to make an appropriate psychological intervention.
Es reconocida la asociación de algunos síntomas somáticos sin causa orgánica con conflictos psíquicos. En Oftalmología existen pocos estudios que evalúen esta asociación, y en los actuales Programas de Formación de Residentes en Oftalmología no se incluye entrenamiento formal en Psicosomática. Esto determina que los fenómenos psicosomáticos en la clínica oftalmológica no sean reconocidos, reduciendo la eficacia terapéutica, la satisfacción de pacientes y médicos, e incrementando los costos en salud. El objetivo de este estudio fue caracterizar pacientes con Síntomas visuales/oculares idiopáticos (SVI), y estimar la prevalencia de indicadores de conflictos psíquicos (CP) en ellos.
Materiales y MétodosSe reclutaron pacientes con SVI durante 12 meses en una consulta oftalmológica. Descartando causa orgánica, se pesquisó en la historia clínica indicadores de CP: diagnóstico psiquiátrico, uso de psicofármacos, enfermedades psicosomáticas en otros órganos, y presencia de crisis biográficas recientes. Se comparó resultados con grupo control.
ResultadosSe registró 39 pacientes con SVI, con una incidencia aproximada de 3%, siendo 74% mujeres, y su edad promedio 41,8 años. Los SVI más frecuentes fueron: irritación de la superficie ocular (51%) y trastornos visuales inespecíficos (17%). Todos los pacientes presentaron al menos un criterio de CP, incluyendo 46,2% psicodiagnóstico, 48,7% usuarios psicofármacos, 48,7% crisis biográficas recientes y 64% enfermedades psicosomáticas en otros órganos. La frecuencia de psicodiagnóstico y enfermedades psicosomáticas en otros órganos fue estadísticamente superior (p<0,05) en relación al grupo control.
ConclusionesPacientes con SVI presentan una alta frecuencia de indicadores de conflicto psíquico. Aunque no es posible asumir un rol causal de los CP en los SVI, su presencia debe alertar al oftalmólogo de la necesidad de la apropiada evaluación e intervención psicológica.